Wednesday, November 21st, 2012 - Mount Saint Vincent University
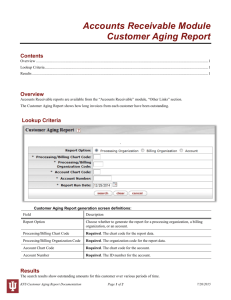
advertisement

Program Abstracts November 21st-23rd, 2012 Delta Halifax Halifax, Nova Scotia, Canada Table of Contents Wednesday, November 21st………………………………………………………………………pg2 Keynote Speaker: Andre Picard…………………………………………………………………pg2 Thursday, November 22nd…………………………………………………………………………pg2 Keynote Speaker: Ann Martin-Matthews……………………………………………………pg2 Oral Presentations Session A………………………….….……………………………………..pg2 Poster Presentations Session A……………………..………………………………………….pg8 Workshops Session B……………………….…………………………………………………….pg13 Oral Presentations Session C………………………………………………………………….pg16 Kathryn Allen Weldon Public Lecture: Dr. Kenneth Rockwood……….………….pg25 Friday, November 23rd……………………………………………………………………………pg25 Panel: Multi-perspective Look at Dementia……….…………………………………….pg25 Oral Presentations Session D………………………….….…………………………………..pg26 Poster Presentations Session D…………………………..………………………………….pg32 Keynote Speaker: Susan Kirkland…………………..………………………………………pg38 Nova Scotia Centre on Aging Page 1 Wednesday, November 21st, 2012 7:00-8:30 pm Keynote Speaker: Andre Picard, The Globe and Mail THE GREYING OF MEDICARE: CAN CANADA’S AGING HEALTH SYSTEM BE REVITALIZED? Much is written about the aging of the population and its impact on health costs. But what about the health system itself – is the 1950s model of healthcare able to deliver 21st century care? A veteran healthcare journalist examines how Medicare should adjust to the needs of the population – and not vice-versa. ______________________________________________________________________________ Thursday, November 22nd, 2012 9:00-10:00 am Keynote Speaker: Anne Martin-Matthews, University of British Columbia THE FUTURE OF AGING: INTERDISCIPLINARY RESEARCH, PRACTICE AND POLICY PARTNERSHIPS There is tremendous diversity and variability in the aged population, which is not always reflected in the current language of research, policy and practice. This presentation situates the aging of Canada’s population within an international context to expand awareness of the complexity of research on aging, and with it, the possibilities and challenges of developing and implementing interdisciplinary evidence-based research partnerships and collaborations. Implications of the heterogeneity of aging populations for health services and systems will be considered, along with multidisciplinary paradigms for thinking about aging. Reflections on the importance of recognizing the diversity and complexity of aging; the need for interdisciplinary research platforms, and practice and policy partnerships; and the benefits of creating linkages across existing projects and data systems conclude the presentation. 10:30 am -12:00 pm Oral Presentations Session A Supporting Care AGING AT HOME: IDENTIFYING SAFETY MARKERS FOR HOME CARE RECIPIENTS Marilyn Macdonald, Dalhousie University; Ariela Lang, VON Canada; Janet Storch, University of Victoria; Lynn Stevenson, Vancouver Island Health Authority Canada’s aging population is advancing; by 2036, 25% of the Canadian population will be over the age of 65. As individuals are living longer, their likelihood of developing one or more chronic illnesses increases. Those who suffer from Chronic Obstructive Pulmonary Disease (COPD) and Congestive Heart Failure (CHF) require a great deal of intricate care. The Nova Scotia Centre on Aging Page 2 majority of this care is provided in the client’s home by family caregivers. Although patient safety is a clear and pressing issue in institutional settings, client safety is a new frontier within the home care context. To address this gap, a CIHR funded scoping review was conducted on home care literature to identify meaningful safety markers for recipients of home care. Results generated seven safety markers attending to the experiences of home care clients and their caregivers: a sense of being left ‘home alone’ to deal with their illness, receiving a ‘fixed’ set of information in a ‘foreign’ clinical language; dealing with numerous health professionals or ‘strangers’ in the home; fulfilling multiple roles; managing medication regimes; being left ‘out of pocket’ due to the costs of required resources in receiving and providing care at home; and risking caregivers ‘own health through increased responsibilities of caring for a loved one at home. Identifying these safety markers will help to inform safety related knowledge and policies within home care practices. The knowledge gained may also help mitigate risks, improve quality of life for clients and caregivers, and assist in supporting a more sustainable health care system. ______________________________________________________________________________ UNDERSTANDING ALZHEIMER’S DISEASE AND OTHER RELATED DEMENTIA Linda Lane, We Care Home Health Services; Rosanna Dolinki, We Care Home Health Services Dementia will affect 1.1 million Canadians in less than 25 years. With between 2% and 10% of all cases of dementia starting before the age of 65, the impact will be seen across the aging population. In conducting staff surveys, client surveys, central intake requests and a national educational needs assessment, we uncovered that clients with Alzheimer’s and other related dementia needed a better care experience in the community. In response to this, we moved ahead on 2 fronts - the development of focused education for our staff and development of an education guide for informal caregivers. Understanding Alzheimer’s Disease is a program for unregulated staff that guides through the basics of caring for clients with Alzheimer’s disease and other related dementia. The focus of the program is to provide staff the skills and knowledge to help clients and their families better cope with the disease as it progresses. We are reviewing the effectiveness of the program – launched in January 2012 - through client and staff surveys and focus groups, to assess the impact of the program on enhancing the client experience. The 2nd step in our journey to enhance client experience was the creation of a Caregiver’s Guide for families looking after loved ones with Alzheimer’s. This guide offers tips on physical and emotional care for the client and for the caregiver. It has been developed using the knowledge of our clinical leaders and through consultation with experts in the field of Alzheimer/Dementia care. 1 http://www.alzheimer.ca/en/Get-involved/Raise-your-voice/WHO-report-dementia-2012 “DOING WHAT COMES NATURAL”: THE DIRECT CAREGIVERS’ EXPERIENCE OF CARING FOR RESIDENTS WITH DEMENTIA Sandee Hicks-Moore, University of New Brunswick Objectives/Perspectives: Direct caregivers, namely personal support workers (PSWs) and licensed practical nurses (LPNs) caring for persons with dementia living in long-term care Nova Scotia Centre on Aging Page 3 (LTC) encounter multiple challenges in their work, yet a clear understanding from their unique perspective of their experiences are missing from the literature. This research identifies their understandings of dementia care and the realities they experience daily at work. Method: This research is informed by hermeneutic phenomenology. Two questions guided the study: 1) What meanings do direct caregivers –PSWs and LPNs – in long term care develop about their experiences of caring for persons with dementia? 2) How may these meanings change, if at all? Fifteen direct caregivers from five different LTC facilities located in rural and urban settings in southern New Brunswick explained their experiences in dementia care. Results: Three themes emerged from the analysis of the data: 1) Adaptation which refers to the caregivers’ abilities to adjust to the unpredictable and often psychological and physically overwhelming situations they experience in caring for residents with dementia. 2) Inclusion which refers to how the caregivers seek ways to stabilize themselves and gain acceptance in the workplace. 3) Denied professionalism indicates the lack of credit given to their knowledge and skills by co-workers, supervisors and administrators of higher status. Conclusion: The findings of this research will be explained in an effort to broaden our understanding of the experiences of the direct caregivers and may be useful in enhancing educational and support programs for PSWs and LPNs. Aging in Place BUILDING AGE-FRIENDLY COMMUNITIES FROM THE COMMUNITY UP: THE NOVA SCOTIA EXPERIENCE Pamela Fancey, Mount Saint Vincent University; Jacqueline Campbell, Nova Scotia Department of Seniors; Brenda Hattie, Mount Saint Vincent University; Janice Keefe, Mount Saint Vincent University Making our communities age-friendly is one of the most effective approaches for responding to our aging demographic. Age-Friendly Communities (AFC) addresses the environmental and social factors that hinder active and healthy aging. Informed by the original research conducted by the World Health Organization (2005) and within Canada by the Public Health Agency of Canada (2007), the Nova Scotia Department of Seniors and the Nova Scotia Centre on Aging have been supporting more than 10 municipalities in Nova Scotia with a strategic planning process aimed at helping them become more age friendly. This work has involved developing broad based advisory committees, community consultation, communications and promotion, and planning for implementation. Support is provided to each municipality individually through the process, as well as support is provided to build a community of practice around age-friendly communities across municipalities. Each municipality has its own strengths and capacities and the Nova Scotia AFC initiative builds upon these in different ways. Results from this inter-sectoral partnership are beginning to emerge demonstrating that the approach being taken is important in helping communities become more age friendly. This presentation will highlight the dialogical approach to this community-based collaborative initiative, and some of the key learnings that have emerged. The messages from this presentation will be beneficial for other jurisdictions interested in age-friendly community at the community, practice or policy levels. Nova Scotia Centre on Aging Page 4 THE CHALLENGES OF AGING-IN-PLACE AS A LONG TERM CARE OPTION Suzanne Dupuis Blanchard, Université de Moncton Seniors want to stay in their homes for as long as possible. While only 7% of seniors currently live in a long term care facilities, over half of seniors living at home wonder how long they will be able to do so. Along with the aging of our population, many questions about the Canadian health care system, and especially our long term care options, have been asked. The goal of this presentation is to present a culmination of qualitative health research on aging-in-place in New Brunswick. Interviews have been conducted with a variety of participants: seniors who have their names on wait lists for relocation in a senior designated apartment building, others who have relocated from their homes, seniors who are currently aging-in-place, and various community agencies who provide services to seniors. Results reflect current challenges for seniors, their families and all levels of governments for aging-in-place as a long term care option. The presentation will highlight the various reasons seniors struggle to age in their homes while also providing a number of solutions. In conclusion, today’s tendency to build nursing homes creates an unbalanced approach to long term care. The results indicate the need the revise existing services and emphasize the importance of developing public policy for aging-in-place. DEVELOPING EVIDENCE-BASED HOUSING FOR OLDER ADULTS Lori Weeks, University of Prince Edward Island; Donald Shiner, Mount Saint Vincent University; Robin Stadnyk, Dalhousie University; Dany J. MacDonald, University of Prince Edward Island To provide evidence about the amount and type of housing that will be needed by older adults, we explored the housing preferences of older adults, the variables that predict housing preferences, and how these results can inform the development of future housing. Our sample included 1,670 Atlantic Canadian older adults who completed a mailed survey as part of the Atlantic Seniors Housing Research Alliance research program. We used hierarchical logistic regression to determine the characteristics of respondents who preferred various types of housing. We also analyzed data from an open-ended question on ideal living arrangements. While a large number of older adults prefer to remain living where they are now, the majority do desire a different housing option in the future. Health and wealth variables yielded some interesting predictors of housing preferences, along with other socio-demographic variables. It is clear that there is no one particular form of housing that will meet the needs of all older adults. However, future forms of housing that ensured an independent living unit such as an apartment, options geared specifically to older adults, and provide access to assistance were most highly preferred by the participants. The results of this study are useful in informing decisions about housing options to develop supports for older adults who prefer to remain living in their homes and their communities and to create forms of housing that best meet the needs of our diverse older population. Nova Scotia Centre on Aging Page 5 Sciences and Dementia BUTYRYLCHOLINESTERASE IMAGING AGENTS TO VISUALIZE PATHOLOGY IN ALZHEIMER’S DISEASE Ian Macdonald, Dalhousie University; Ian Pottie, Mount Saint Vincent University; Earl Martin, Mount Saint Vincent University; Sultan Darvesh, Dalhousie University Background: Butyrylcholinesterase (BuChE) is an enzyme that, among other functions, catalyzes the hydrolysis of the neurotransmitter acetylcholine. Increased levels of BuChE are associated with the pathology of Alzheimer’s disease (AD). This association makes BuChE a suitable target for disease-specific imaging of this neurological disease. We propose that BuChE-specific radiopharmaceuticals can be used for brain scanning to detect this enzyme in vivo, and thus the pathology associated with AD. As a preliminary step towards this goal, imaging agents have been synthesized and evaluated in rodent and human brain tissues. Methods: BuChE-specific radioligands were administered to wild type and transgenic AD rodents as well as incubated with post-mortem normal and AD human brain tissues. The distribution of radioactivity was determined via autoradiography. BuChE inhibitors were used to confirm specificity of the radioligand binding to this enzyme. Results: Autoradiographic analysis of rodent and human brain tissues indicated accumulation of radioactivity in areas known to contain BuChE as determined by histochemical analysis. Furthermore, presence of a BuChE inhibitor attenuated accumulation of radioactivity. Preliminary results indicate that AD tissues can be distinguished from normal human brain. Conclusions: BuChE has previously been implicated in the pathology of neurological diseases. We have synthesized several BuChE imaging agents. Autoradiography, in experimental animal and human brain tissue indicates that these agents have the potential to provide a non-invasive means for early diagnosis and treatment monitoring of AD using brain scanning. WHAT DO MOUSE MODELS TEACH US ABOUT AGING? Richard Brown, Dalhousie University; Rhian Gunn, Dalhousie University; Timothy O’Leary, Dalhousie University; Kurt Stover, Dalhousie University Our lab studies the neurobehavioural changes in genetically modified mice as they age. There are three purposes for these studies. First, to understand the basic behavioural changes associated with aging. Second, to understand the neural and genetic mechanisms underlying these changes, and third, to use these mouse models to develop new treatments for age-related disorders. We have examined mouse models for glaucoma and Alzheimer's disease. The DBA/2J mouse develops age-related glaucoma and is functionally blind by 12 months of age. We examined the effects of blindness on learning and memory in these mice and showed that treatment of glaucoma with Timoptic XE improved visual ability and performance on visuo-spatial tests of learning and memory. We are testing a number of mouse models of Alzheimer's disease and are finding that these mice have age-related visual and motor control problems as well as cognitive decline. For example, the double transgenic APPswe/PS1de9 mouse shows deficits in visual acuity but not in olfaction. One of our goals is to dissociate the sensory and motor deficits from deficits in cognitive function. Another goal is to examine sex and strain differences in the development of age-related Nova Scotia Centre on Aging Page 6 disorders. Data will be presented on age-related behavioural deficits in the 3X-Tg and 5x FAD mouse models of Alzheimer's disease. The development of new drugs depends on a complete knowledge of the neurobiological mechanisms underlying diseases of aging and the goal of our research is to uncover these mechanisms. Supported by NSERC of Canada. Retirement Opportunities and Challenges COMPREHENSIVE RISK MANAGEMENT IN THE THIRD AGE: WOMEN’S SPECIAL CHALLENGES Brigitte Neumann, Retired; Leroy Stone, Université du Montreal Comprehensive risk management involves a network of strategies designed to address an array of possible losses so as to achieve the best available, or the optimum, allocation of one’s limited coping resources. This is important for individuals and families in the Third Age, especially women due to their greater chances of reaching advanced age. Women’s special challenges occur in a variety of domains, including the following: (a) the risks of outliving one’s financial resources, particularly in light of the likelihood of becoming widowed; (b) women’s greater chances of experiencing years with serious disability in later life; (c) social risks including the loss of family, friends and social networks as one’s age cohort dies off; and (d) risks of experiencing years with caregiving responsibility in later life. Such issues faced particularly by women give rise to the question of whether they are better prepared than men to address retirement’s challenges. Our research, based on the 2007 General Social Survey, shows that generally they are not as well prepared as men, and that there are key population segments in which the lesser preparedness of women is marked. These population segments with relatively low retirement preparedness include married immigrant women; women who are single, widowed or divorced; and women at the highest and lowest level of education and income. The presentation concludes with some recommendations for specialists who work on behalf of senior women. AGING AND MOBILITY: INTERNATIONAL MIGRATION AS A RETIREMENT STRATEGY Liesl Gambold, Dalhousie University There are 10.1 million baby boomers in Canada, which is a proportion of the population far greater than other countries. Thus, understanding the lifestyle choices of retirees and the government policies within which they make these choices has never been so crucial. These individuals’ decisions will have far-reaching implications culturally, politically and economically. Since larger numbers of seniors are living their retirement years in economically challenging situations, this paper examines the mobility of elderly men and women in the form of international retirement migration as an increasingly popular strategy to ameliorate levels of economic and general well-being. This paper examines retirement as a process reflecting individual histories and preferences as well as shifting global, cultural, and ideological values. Employing standpoint theory, used by many feminist scholars, this paper begins by taking “everyday life as problematic” and the understanding that the aged are socially and culturally marginalized. With a growing aging population, however, this marginalization will surely be altered. International retirement migrants face the same challenges as the aging population at large such as health changes and concerns, mobility issues, financial questions and their over-all sense of well-being. However, they face the Nova Scotia Centre on Aging Page 7 complex aging process in a foreign country and have the added difficult task of manoeuvering cross-culturally. Based on empirical, anthropological research done in Mexico, Spain, and southern France, this paper highlights the efforts of retirees to forge a new path, choose a new homeland and, perhaps, reinventing themselves a bit along the way. AN EXPLORATION OF THE RELATIONSHIP BETWEEN RETIREMENT REASONS AND RETIREMENT CONGRUENCY Aine Humble, Mount Saint Vincent University; Jan Boswell, Mount Saint Vincent University Research has typically regarded retirement as forced or chosen, but the retirement decision is not necessarily a dichotomous one. According to Schellenberg and Silver (2004), three types of retirement congruency (RC) are possible: (a) low (forced), (b) moderate (part forced/part wanted), and (c) high (chosen); however to date, limited research has been carried out on the moderate category. The relationship between various retirement reasons (in particular, beyond job and health loss) and RC has also not been explored in multivariate analyses. Thus, using a modified version of Szinovacz and Davey’s (2005) perceptions of forced retirement model, we explored the relationship between retirement reasons and an individual’s assessment of their RC. Secondary data analysis of the 2007 General Social Survey was conducted on a subsample of 1166 individuals who retired between ages 50 to 78 years. Percentages in the RC categories were: high: 30% (n = 347), moderate: 53% (n = 615), and low: 17% (n = 204). Multinomial logistic regression showed that moderate RC is theoretically different from low and high RC. Eight variables were significant in the low/high RC comparison; nine variables in the low/moderate RC comparison (of which three were unique—life satisfaction, discrimination, and having worked at an early age); and five variables significant in the moderate/high comparison (of which three were unique—CPP/tax rules, work stressful/physical, and work part-time/change career). This study provides insight into how retirement reasons are related to RC. Policy implications for employers, unions, educators, and government officials are presented. 10:30-12:00 Poster Presentations Session A Disability, Health Services, Building Capacity CDKTN: LINKING KNOWLEDGE TO KNOWLEDGE USERS Cheryl Cook, Geriatric Medicine Research/Canadian Dementia Knowledge Translation Network As the number of people with dementia grows, challenges for their care partners also grow including timely access to research-based evidence, practices, services and resources in their communities. The Canadian Dementia Knowledge Translation Network (CDKTN) was established to facilitate knowledge translation with the aim of improving the care and health of Canadians with dementia. CDKTN helps researchers, students and practitioners translate their work into practice and works to distribute it to those who need it most – people with dementia, families and care partners. Our areas of focus include Education and Training in Knowledge Translation (for researchers), the Canadian Dementia Resource and Knowledge Exchange (for a wide spectrum of frontline professionals) and Person and Care Partner Nova Scotia Centre on Aging Page 8 Centered Knowledge Translation. We also have a new area of focus in Policy, which is headed partly by Dr. Janice Keefe at the Nova Scotia Centre on Aging. This presentation will share the practical tools and services that CDKTN is providing now and in the future. These include a variety of web-based resources for professionals, persons with dementia and families, as well as upcoming training programs for researchers, and dementia guideline dissemination projects aimed at physicians and health care professionals. PHYSICAL ACTIVITY IN PATIENTS WAITING FOR KNEE REPLACEMENT Logan Lawrence, University of Alberta; Allyson Jones, University of Alberta; Bob Haennel, University of Alberta; Bruce Dick, University of Alberta Background: As with many chronic conditions, exercise is recommended for persons with osteoarthritis (OA). However, daily physical activity (PA) levels and participation patterns remain relatively unknown in end stage arthritis. Objective: This pilot study examined PA and associated health factors in older adults with end stage OA who were awaiting knee replacements. Methods: Participants completed a structured interview regarding activity level, function, fear of pain, and other psychosocial measures. PA was measured using the SenseWear™ Pro Armband (SWA; Body Media, Pittsburgh, PA). The SWA was worn continuously for 4 consecutive days and estimated daily energy expenditure, steps/day, and time spent at sedentary, low, moderate, and vigorous activity intensities. Self-report PA was measured using the Yale Physical Activity Survey. Descriptive analysis of PA, clinical symptoms, and health status was completed. Results: 10 participants (age: 56 – 83 yrs) reported a mean 204 ± 63 minutes of daily moderate to vigorous PA, compared to the SWA mean of 86 ± 76 minutes. Daily sedentary time was 85% ± 8.6%. Western Ontario and McMaster University Arthritis Index mean joint pain and function scores were 52.5 ± 13.7 and 52.4 ± 11.8. Mean quality of life Knee Injury and Osteoarthritis Outcome Score was 50.8 ± 18.3. Most participants reported leisurely walking as the most popular activity. Six recorded less than 7500 steps/day. Implications: Findings from this pilot suggest that PA measures need to evaluate both active and sedentary activities. Further methods to identify patients who are not meeting Canada’s recommended PA guidelines are required. PROPORTIONS OF FRAIL AND FITTEST COMMUNITY-DWELLING OLDER ADULTS IN EUROPE Olga Theou, Dalhousie University; Thomas Brothers, Dalhousie University; Michael Rockwood, Dalhousie University; Arnold Mitnitski, Dalhousie University Objectives: To compare the proportions of frail and fittest older adults across 15 European countries. Methods: Fifteen countries (Austria, Belgium, Czech Republic, Denmark, France, Germany, Greece, Ireland, Israel, Italy, Poland, Netherlands, Spain, Sweden, Switzerland) were included the Survey of Health, Ageing, and Retirement in Europe. A frailty index was constructed for 16759 participants aged 65+ years (mean 74.3 ± 6.9 years; 59% female), from 70 age-related health measures associated with adverse outcomes. Frail older adults were defined as those with a frailty index score ≥0.25 and the fittest older adults as those with a frailty index score ≤0.03. Gross domestic product per capita (GDP) was used to Nova Scotia Centre on Aging Page 9 examine the relationship between national income and proportions of frail and fittest older adults. Results: 36.4% of participants were identified as frail and 1.5% were identified as the fittest. For the frail group, mortality was 14.6% at 24 months and 21.7% at 40 months, and for the fittest group, mortality was 0.2% and 2.5%, respectively. The proportion of frail older adults in each country ranged from 13.2% (Switzerland) to 63.2% (Poland), while the proportion of older adults classified as the fittest varied from 0.1% (Spain) to 4.4% (Denmark). GDP was correlated with the proportion of both frail (r= -0.83, p<0.001) and fittest older adults (r= 0.72, p<0.01). Conclusions: The proportions of frail and fittest older adults differ across countries; the wealthiest countries demonstrated the lowest levels of frailty and the highest levels of fitness. STOPP/START CRITERIA: BENCHMARKING PRESCRIBING QUALITY IN OLDER PERSONS AND DETERMINING CLINICAL, HUMANISTIC AND ECONOMIC IMPACT Barbara Hill-Taylor, Dalhousie University; Ingrid Sketris, Dalhousie University; Jill Hayden, The Nova Scotia Cochrane Resource Centre; Stephen Byrne, Dalhousie University; David O’Sullivan, University College Cork The STOPP criteria (Screening Tool of Older Persons’ Potentially inappropriate Prescriptions) were developed to facilitate systematic screening for potentially inappropriate drug prescribing in older persons. Researchers in Nova Scotia and Ireland are collaborating to conduct a systematic review that assesses the impact of using STOPP criteria. We conducted a comprehensive search for published studies in the standard medical databases between January 2007 and January 2012. We searched databases of conference abstracts and reference lists of included articles. We contacted authors of abstracts and non-English publications. We selected studies that used STOPP criteria in patients aged 65 years and older, and examined health-related and cost outcomes. Two reviewers independently assessed risk of bias and extracted data for analysis. We have included 16 international studies, including three that used partial or modified versions of the STOPP criteria. The primary outcome measures are the identification of the rates of potentially inappropriate prescribing, adverse drug events, and costs associated with potentially inappropriate drug use. The majority of the studies are observational. Metaanalysis of the study findings may not be possible due to heterogeneity. Where study outcomes cannot be combined, a narrative synthesis will be performed. Optimization of drug prescribing in older persons is a priority due to the significant humanistic, clinical and economic impacts of drug-related adverse events. This synthesis will provide valuable groundwork and benchmarking to inform research into the local adaptation of the STOPP criteria. ACCUMULATION OF NON-TRADITIONAL RISK FACTORS PREDICTS CORONARY HEART DISEASE EVENTS Lindsay Wallace, Dalhousie University; Olga Theou, Dalhousie University; Michael Rockwood, Dalhousie University; Susan Kirkland, Dalhousie University; Karina Davidson, Columbia University; Daichi Shimbo, Columbia University; Kenneth Rockwood, Dalhousie University Objective: To examine the ability of traditional and non-traditional risk factors to predict adverse events related to cardiovascular disease (CVD). Methods: 3157 community-dwelling Nova Scotia Centre on Aging Page 10 adults participated in the Nova Scotia Health Survey (mean age 48.4, 49.8% males). Two different frailty index (FI) measures were constructed for each participant. One version included 15 health deficits not known to predict CVD (the non-traditional risk factors frailty index; FI-NTRF). The other version (FI-C) combined the 15 non-traditional risk factors with 6 traditional risk factors: history of diabetes, hypertension, smoking, high body mass index, and high levels of cholesterol and triglycerides. All-cause mortality and CVD-related hospitalization and death were followed for 10 years after baseline (1995-2005). Results: In a logistic regression model adjusted for age and sex, each traditional risk factor was independently predictive of CVD event. The FI-NTRF score was predictive of CVD events (OR 1.23, ρ<0.001, CI 1.11-1.37), even when all independent traditional risk factors were added to the model (OR 1.23, ρ=0.001, CI 1.09-1.38). FI-C score was also predictive of CVD events (OR 1.36, ρ<0.001, CI 1.23-1.50). The FI-NTRF discriminated people who had CVD events at follow-up from those who did not with an area under the receiver operating characteristic (ROC) curve of 0.71, while the FI-C had an area under the ROC curve of 0.72. Conclusions: Non-traditional and traditional risk factors add unique contributions to the prediction of adverse outcomes related to CVD. General health status should be considered in addition to traditional risk factors for the prediction of late-life disease. ATTENTION NETWORKS AND THEIR INTERACTIONS IN HEALTHY AGING Yoko Ishigami, Dalhousie University; Michael Lawrence, Dalhousie University; Raymond Klein, Dalhousie University; Gail Eskes, Dalhousie University Changes in attention are common in older adults and can impact a variety of daily activities, including work and driving. Attention is not a unitary system, but includes multiple independent, yet interacting brain systems that underlie functions related to alerting (responding to unexpected events), orienting (ability to identify and focus on important information), and executive control (managing multiple task demands). However, changes in these networks and especially in their interactions with normal aging are not clear. The efficiency and interaction of these networks can be measured by the computerized Attention Network Test and its modified version. They differ in the type of orienting they measure (voluntary vs. automatic) and modality of alerting (visual vs. auditory). Both tests were administered to healthy young (aged between 18-30, n=10), middle aged (aged between 36-52, n=7), and older (aged between 65-76, n=10) adults. Participants indicated the direction of a target arrow surrounded by distractors. The arrows were preceded by visual and/or auditory cues. Overall, reaction time slowed but error rate improved with age. With increasing age, sensitivity to alerting cues depended upon modality, but alerting could improve the other attention networks under the right conditions. Increased network scores of orienting and executive control speed were often compensated by decreased network scores in error with age, making interpretation complex. These results can be used to understand how attention changes with age and in what ways it can be improved. Understanding how to maintain good attention is important especially for developing effective aging interventions. Nova Scotia Centre on Aging Page 11 FRAILTY IN IMMIGRANT AND NON-IMMIGRANT MIDDLE-AGED AND OLDER EUROPEANS Thomas Brothers, Dalhousie University; Olga Theou, Dalhousie University; Michael Rockwood, Dalhousie University; Arnold Mitinski, Dalhousie University; Kenneth Rockwood, Dalhousie University Objective: The purpose of this study was to compare characteristics of frailty in immigrant and non-immigrant middle-aged and older community-dwelling Europeans. Methods: Fifteen countries participated in the first two waves of the Survey of Health, Ageing, and Retirement in Europe study. A frailty index (FI) was constructed for 36 306 participants aged 50+ years (mean 65.2 ± 10.4 years; 55% female), from 70 age-associated health measures. Results: 10.8% (n=3 923) of participants were immigrants, with an average 42.5±18.3 years since migration. Compared with non-immigrants, immigrants were older (65.5±10.1 vs. 64.7±10.1 years; p<0.001) and more educated (ISCED-1997 level 2.78±1.6 vs. 2.47±1.5; p<0.001), and showed a similar distribution by sex (55% female; p=0.3). Immigrants had a higher FI score than non-immigrants (0.19±0.14 vs. 0.16±0.13; p<0.001), even after controlling for age, sex, and education level (p<0.001). Among immigrants, a longer time since migration was associated with a lower FI score (R=0.17, p<0.001). All-cause mortality between groups was similar at 24 months (3.5% vs. 3.6%; p=0.8) and 40 months (5.5% vs. 6.1%; p=0.5). When matched by age, sex, education level, and country of residence (2982 matched pairs), immigrants maintained a higher FI score than non-immigrants (p<0.001), and similar all-cause mortality at 24 (p=0.7) and 40 months (p=1.0). Conclusion: Middleaged and older European immigrants demonstrate a higher level of frailty than their nonimmigrant peers. Multiple interacting medical, socioeconomic, and cultural factors may contribute to this phenomenon. DEVELOPING A RESEARCH COMMUNITY IN AGING Scott Grandy, Dalhousie University; Colin Hebb, Dalhousie University; Jerome Singleton, Dalhousie University It is estimated by the year 2035 that 25 percent of the global society will be over 65. The perception of aging in industrial societies that is emerging shifts the perception of Aging from a negative impact on society to one that has economic and social benefits to a society. The purpose of this study was to engage researchers interested in aging in a dialogue regarding this shift in the paradigm of Aging. Two focus groups were conducted in Eastern Canada. The following themes emerged. First, it was recommended that aging be viewed as a continuum across the entire life course instead of simply an issue to be addressed once an individual/population has reached the age of 65. Secondly, how do lifestyle decisions across the life course relate to physical activity and exercise, access and use of technology, retirement, location of residence (urban versus rural), persons occupation, type of residence, social experience and the persons culture effect how a person ages. This presentation will provide insights into the directions suggested in this study to develop a multidisciplinary research community related to the shifting paradigm. Nova Scotia Centre on Aging Page 12 THE LONGEVITY DILEMMA - REDUCING POVERTY IN OLD AGE THROUGH PRIVATE SAVINGS Beverley Preddie, University of Westminster Research problem: The provision of social insurance in old age clearly represents a fiscal burden for Governments on a global scale. With longevity increasing, new reforms have been proposed in the United Kingdom (UK) to boost individuals savings towards retirement. Given the fact there are high levels of unemployment, part-time employment and self employment combined with very little disposable income, many individuals are likely to face poverty in retirement. Aim and objectives: The purpose of the paper is to predict the likelihood of individuals to plan more effectively for old age. The research objectives include an assessment of the labour market trends to determine the extent of disparities within the labour market restricting the ability the save effectively. Methodology: Extensive empirical analysis will be carried out using the UK Labour Force Survey to provide a comprehensive view of the labour market progression of individuals. This analysis is undertaken using Statistical Package for Social Sciences (SPSS) to address the research questions. Findings and contribution to knowledge: Although preliminary findings suggest that the majority of individuals will be incapable of meeting the new private savings obligation, this study seeks to empower and build an awareness of the importance of planning and saving for retirement. The patterns and trends retrieved through the study can aid significantly in developing and promoting a framework through which the UK Government can refine their pension strategies. 1:30-3:00 pm Workshops Session B Ageism: The Other Side of the Aging Coin AGEISM: THE OTHER SIDE OF THE AGING COIN Glen Hougan, Nova Scotia College of Arts and Design University This workshop explores the physical changes associated with ageing and our perception of aging. The objective of this workshop is help participants examine ageing issues and ageist attitudes in order to gain a better understanding of the problems and opportunities in designing and delivering products and services for our ageing population. Using an ‘ageing suit’, which simulates the physical changes of ageing, participants will undertake a number of activities exploring the perceptions and realities associated with ageing. Through these activities participants will examine their perceptions and reactions to ageing, and examine ways to address ageism in our society and in their work. How we as a community responds to the needs of an ageing population, whose growth and numbers will be unprecedented in human history, will be important to those involved in developing services and products for this demographic. Ageism, discrimination based on age, is widespread but one of the least addressed prejudices. The workshop is an immersive experience that explores issues of ageing and ageism in our community with the goal of helping participants understand the realities of ageing, challenge ageist attitudes, and understand how ageism can be reflected in our lives and work Nova Scotia Centre on Aging Page 13 Raising Awareness about the Abuse of Older Adults: A PEI Network Response RAISING AWARENESS ABOUT THE ABUSE OF OLDER ADULTS: A PEI NETWORK RESPONSE Lori E. Weeks, University of Prince Edward Island; Olive Bryanton, University of Prince Edward Island; Gloria McInnis-Perry, University of Prince Edward Island; Paul Chaulk, Atlantic Evaluation Group We recently completed a two-year project funded by New Horizons for Seniors to raise awareness about the abuse of older adults on PEI. In this workshop, our objectives are to provide participants with information about specific components of the awareness-raising activities we completed and the evaluation results of these activities. Workshop participants will be given the opportunity to explore how the materials, activities, and processes that we developed can be adapted for use in other jurisdictions. In addition, we will explore how to incorporate mechanisms to ensure the sustainability of a network focusing on raising awareness about the abuse of older adults. The specific components of our project that we will share during the workshop are our successes, challenges, and lessons learned in 1) developing a presentation for peer educators to deliver in the community, 2) training older adults to be peer educators, 3) implementing the peer education process, 3) organizing two provincial forums, 4) creating materials to be distributed through the Women’s Institute of PEI, and 5) developing an intersectoral network of academics, practitioners, policymakers, and older adults. All of the materials that we developed during our project will be made available to workshop participants. We received ethical approval to use our evaluation results for research purposes, and the evaluation results of the various components of our project will be shared and used to help identify how participants can best utilize the processes (i.e. communication systems) and materials (i.e. educational resources) that we developed. Expanding Our Horizons: Building Capacity for Interdisciplinary Research in Aging EXPANDING OUR HORIZONS: BUILDING CAPACITY FOR INTERDISCIPLINARY RESEARCH IN AGING Janice Keefe, Mount Saint Vincent University; Gail Wideman, Memorial University In the ‘changing landscape’ of aging studies, practice, and policy, an interdisciplinary collaborative approach is increasingly recognized as essential to the future of aging research (Piccinin & Hofer, 2008). The purpose of the workshop is to bring together academic discipline-based, policy, and applied perspectives to converge on the issue of collaborative research on aging. In this workshop, two researchers with experience with interdisciplinary aging-related research collaborations, and a facilitator with expertise in team-building, grant application and peer-review, will share their experiences related to fostering interdisciplinary collaborations in aging-related research. The specific objectives of this workshop are: 1) To identify areas of interest in aging-related research; 2) To identify researchers, practitioners and policy makers with expertise and interest in interdisciplinary aging-related initiatives and collaborations; 3) To examine the characteristics for successful interdisciplinary collaborations. To achieve its objectives, the workshop will include examples from two Atlantic Canadian research initiatives: a multidisciplinary, multi-sectoral provincial aging health network, and a nationally-funded research project examining nursing home models of Nova Scotia Centre on Aging Page 14 care. Participants will discuss opportunities and challenges around multi-sectoral inter- and multidisciplinary work, explore opportunities for collaborations with their colleagues, and examine the conditions and characteristics required for successful networks and/or research collaborations. The workshop is expected to identify potential research areas of interest, capabilities and mechanisms for possible collaborations to emerge. Works Cited: Piccinin, A., & Hofer, S. (2008). Integrative analysis of longitudinal studies on aging: Collaborative research networks, meta-analysis, and optimizing future studies. In Hofer, S. & Alwin, D. (Eds.), Handbook of cognitive aging: Interdisciplinary perspectives. Pp. 446-476. Thousand Oaks, CA: Sage Publications. Enriching Your Projects Through Collaboration: Using a Pro-Action Café to Facilitate Effective Sharing, Learning and Collaborating in Research on Aging SO HERE WE ALL ARE…NOW WHAT? USING THE PRO-ACTION CAFÉ METHOD FOR EFFECTIVE SHARING, LEARNING AND COLLABORATING IN YOUR PROJECTS Cheryl Cook, Geriatric Medicine Research; Sherri Fay, Geriatric Medicine Research In this 1.5 hr workshop, participants will learn about and use Pro-Action Café to harness collective knowledge, information and resources in a gathering of people over a short period of time. A Pro-Action Café allows multiple participants to put their burning topics, questions or projects on the table - quite literally. Other participants then offer their insights, knowledge and resources in three rounds, addressing: 1.What is the question behind this project? 2. What am I missing? 3. What steps do I need to take/ what help do I need? Pro-Action Café is scalable from 15 people to hundreds, and offers an action-oriented approach to questions and issues. The workshop begins with a brief introduction to the origins and purpose of Pro-Action Café. The standard structure is outlined and we offer examples of its use in a variety of settings. Participants then take part in a condensed Pro-Action Café. The overarching topic is Research on Aging in Nova Scotia. Participants can bring their topic/question around a research project/collaboration on which they are hoping for some input or assistance from other participants. After three rounds of input, a discussion period follows for participants to share insights and reflect on how this tool can be used to enhance or inform projects and collaborations. Resources for further learning and use of Pro-Action Café (as well as Open Space Technology and World Café) will be provided to all participants. Connecting Interprofessional Education and Long term care: Learning Collaboratively CONNECTING INTERPROFESSIONAL EDUCATION AND LONG TERM CARE: LEARNING COLLABORATIVELY Tanay Sharma, Maplestone Enhanced Care, Shannex; Anne Godden Webster, Dalhousie University; Heidi Lauckner, Dalhousie University; Tom Mersereau, Superstore Pharmacy, Nova Scotia Centre on Aging Page 15 Bedford, NS; Vonda Hayes, Dalhousie University; Nancy Edgecombe, Dalhousie University; Ellen Hickey, Dalhousie University; Jennifer Isenor, Dalhousie University Room for capacity building exists in the long term care (LTC) sector to respond to the complex needs of older adults in a way that maximizes the potential of the interprofessional team. To address this, a partnership was formed between Shannex, a family-owned provider of seniors’ care services, and Dalhousie University’s Faculty of Health Professions and Department of Family Medicine to create the first academic nursing home of its kind in Atlantic Canada. Located at Maplestone Enhanced Care, a licensed LTC facility in Halifax, the Collaborative Learning Center (CLC) is an interprofessional learning environment that aims to facilitate a positive change in learners’ attitudes towards long term care and to equip learners with the competencies necessary for interprofessional collaboration (IPC). To date, over 204 learners from 12 professions have completed clinical rotations through the CLC. Informal feedback suggests positive changes at student and organizational levels, with coordination of learner schedules an ongoing challenge. This workshop aims to build on the experiences of the CLC in order to promote discussion and planning around interprofessional learning and collaboration in other LTC settings. By the end of this workshop, participants will: 1. Be introduced to one example of collaborative learning in LTC as shared through the perspectives of different stakeholders 2. Identify and share potential challenges and opportunities related to collaborative practice and learning in LTC 3. Generate strategies for promoting learning opportunities in a range of settings In this workshop, an overview of the CLC will be provided as one example of collaborative learning in LTC from the perspective of students, clinicians, administrators and educators. Participants will then be invited to share how other settings are currently promoting IPC and other opportunities for IPE. In small groups, workshop participants will discuss challenges and opportunities related to promoting collaborative care and interprofessional learning experiences in their own contexts. Through this discussion, interested stakeholders will identify resources and strategies for promoting learning opportunities related to collaborative practice in a range of settings. A list of potential resources and contacts will be generated to support the establishment of IP clinical education opportunities in different settings. 3:30-5:00 pm Oral Presentations Session C Models of Care: Shifting Perspective FROM HORROR TO HOTEL: CANADIAN LITERARY DEPICTIONS OF THE NURSING HOME Patricia Life, University of Ottawa Due to its grim beginnings in Victorian workhouses, late-life institutional care in the West has long borne a horrific public image. In twentieth-century literature dealing with late life, such as Margaret Laurence’s novel The Stone Angel, Edna Alford’s short stories A Sleep Full of Nova Scotia Centre on Aging Page 16 Dreams and Constance Rooke’s edition Night Light, the nursing “home” plays the role of spectre, the dreaded fate that waits to seize us all. However, for the last two decades, writers such as Richard B. Wright, Alice Munro, Joan Barfoot, Lola Lemire Tostevin, and Sara Gruen have begun to portray more positive lifestyles within these facilities. Collectively, these writers suggest that residents of today’s “homes” have the potential to retain attitudes and behaviours previously associated with youthfulness, despite advancing chronological age. This recent change in representation of the “home” is not surprising when we consider that these writers reflect a twenty-first-century Canada where the boomer generation believes it can stay vigorous forever; where government and media increasingly require independence in the old; where globally dispersed relatives make familial care less available to the old; where the range of institution types is broadening to meet a growing market; and where a heightened standard of care is now available for those who can afford it. My conference paper will focus on Joan Barfoot’s darkly humorous novel Exit Lines as an illustration of what I would argue is the Western public’s reimagined picture of the late-life “home” or long-term-care institution: a place where residents can choose to maintain control of their own destiny. THREE PERSPECTIVES ON NURSING HOME QUALITY OF LIFE IN NS: RESULTS FROM A PROVINCE WIDE SURVEY OF NURSING HOME RESIDENTS, FAMILY MEMBERS AND STAFF Janice Keefe, Mount Saint Vincent University; Kevin Kelloway, Saint Mary’s University; Marie Earl, Dalhousie University; John Hirdes, University of Waterloo In Nova Scotia, the continuing care sector is undergoing significant changes including an emphasis on resident-centered care, shifts in staff scope of practice and innovative physical designs. It is important to explore and understand the advantages and disadvantages of innovations currently under way. The Care and Construction project explores the extent and ways in which differences in models of care in Nova Scotia nursing homes impact resident quality of life (QOL). Nursing home residents, family members and nursing home staff members from more than 20 nursing homes sites across the province completed the interRAI Resident Quality of Life survey from their respective perspective. This presentation will offer preliminary results from the survey data, across the three respondent groups, pertaining to key elements of quality of life. Similarities from each group will be described and differences highlighted to underscore the value of myriad perspectives in understanding the QOL experiences of residents. This research has implications for furthering the understanding of the experiences of resident QOL and will help to understand the utility of the interRAI Resident Quality of Life survey for families and staff. LEARNING ABOUT NURSING HOME MODELS OF CARE AND RESIDENT QUALITY OF LIFE: BENEFITS OF A CASE STUDY APPROACH Robin Stadnyk, Dalhousie University; Marie Earl, Dalhousie University; Grace Warner, Dalhousie University; Thea Brown, Mount Saint Vincent University The Nova Scotia long term care system has embraced new models of nursing home care which include changes to physical design, staffing models and philosophies of care. This presentation shares preliminary results of case study research examining resident quality of life in relation to 3 different models of nursing home care in Nova Scotia. The theoretical Nova Scotia Centre on Aging Page 17 framework driving the research, developed from a review of literature on models of care, links the 3 aspects of models of care to 5 components of quality of life: relationships, activities, autonomy, affect and home-likeness of the facility. Six qualitative case studies are being conducted, 2 each in 3 nursing homes representing 3 different models of care. Each case study comprises of interviews with a resident, a family member and a staff member involved in their day to day life; activity monitoring; and participant observation. Interviews and participant observations focus on the 5 quality of life components. Data will be collected at 3 times over an 8 month period; this presentation focuses on the first data collection period. The objective of this presentation is to show how the different data sources contribute to our understanding of resident quality of life, and how aspects such as care delivery, staff-resident-family relationships and resident functional status are revealed differently through different data sources. Taken together these data demonstrate a view of resident quality of life that is unique, adding to researchers’ and decision makers’ understanding of the complexity of the interactions between care models and resident experiences. Rethinking Resilience in Aging HEALTHY AGING, HIV, AND CHRONIC ILLNESS IN CANADA: IS THERE ROOM FOR PEOPLE LIVING WITH HIV WITHIN HEALTHY AGING FRAMEWORKS? Alexandra Hill-Mann, Dalhousie University; Jacqueline Gahagan, Dalhousie University; Eric L. Ross, Acadia University; Denver Lewellen, Dalhousie University Significant advancements in antiretroviral (ARV) therapies since the mid-1990s have lead to a growing population of people living longer and aging with HIV. As a result of this extension of life expectancy following an HIV diagnosis, it has been suggested that HIV become reclassified as a chronic disease. The current policies and practices surrounding healthy aging and chronic disease in Canada do not adequately address the episodic nature of the illness and the impact of stigma and discrimination on people living with HIV (PHA). This is in part due to the lack of space within conventional frameworks related to ‘Healthy Aging’ for chronic episodic illnesses. This work seeks to find space for PHAs within frameworks of ‘Healthy Aging’. In particular, the Episodic Disability Framework (O’Brien et al., 2008) is used to illustrate the needs of this emerging population. A scoping review of the policy and programming literature from 1995 (the year ARVs became widely available) and onward pertaining both to ‘Healthy Aging’ and to HIV as a chronic illness were undertaken. Gaps were identified in existing frameworks of healthy aging as well as in national strategic documents that endeavour to guide healthy aging and wellness policies and programming. This synthesis of the literature seeks to present recommendations for adapting frameworks of healthy aging to enable policymaking that is inclusive of, responsive to, and appropriate for PHAs. These include: adopting a more inclusive strategic vision of healthy aging; modifying and maintaining HIV exceptionality; and expanding research and eliminating policy gaps. Nova Scotia Centre on Aging Page 18 RE-EXAMINING ASHRA’S DETERMINANTS OF HEALTH IN RELATION TO THE SALUTOGENIC APPROACH TO ASSESS RESILIENCE AMONG ATLANTIC CANADIAN SENIORS Judy-Lynn Richards, University of Prince Edward Island; Kathleen Cruttenden, University of New Brunswick In this re-analysis of a current Canadian study, we apply a salutogenic framework to the qualitative findings from the 15 focus groups of the Atlantic Senior’s Housing Research Alliance (ASHRA). The salutogenic framework (Antonovsky 1989; Wiesmann and Hannich 2010) advances a successful aging framework, concentrating on the causes of health and its maintenance and promotion, rather than on pathogenesis and prevention of disease or illness, to reveal further insights about several dimensions of health, such as resilience in the areas of mental, physical, and self-assessed health. Resilience generally refers to the capacity to bounce or spring back from a physical, emotional, financial, or social challenge. Contributing such knowledge on resilience about seniors in rural Atlantic Canada is critical because life in this region is unique, presenting several barriers to the Canadian social determinants of health (e.g., housing, finances, access to health and social care, culture, etc.), all of which can affect one’s ability to be resilient. Moreover, Atlantic Canada has one of the highest percentages of seniors nationally. Using the salutogenic framework (i.e., identifying generalized resistance resources, sense of coherence, and balance of healthease/disease), our analysis provides insight into how seniors in the ASHRA project were able to be resilient, i.e., maintain or sustain their mental, functional, and social health. This type of information will be informative for policy makers and planners to help them identify how to address barriers affecting resilience. THE ROLE OF NARRATIVE CARE IN ENHANCING RESILIENCE AMONG OLDER ADULTS Clive Baldwin, St. Thomas University; William Randall, St. Thomas University; Daphne Noonan, York Care Center; Sue McKenzie-Mohr, St. Thomas University Of growing interest to gerontologists are the factors that inform resilience in older adults, namely the ability to respond to the adversities and deficits of later life so as to continue truly growing old and not merely get old (Randall, in press). Bohlmeijer et al (2009) have shown that narrative-based interventions help reduce symptoms of depression, increase personal mastery and enhance personal meaning; and McAdams (2001) suggests that strong life stories reflect such characteristics as coherence, differentiation, generative integration, and openness. We report on a pilot study of the differences between the stories of those who rank highly on a valid and reliable resilience scale and those who score poorly. The Connor-Davidson resilience scale (2003) was administered to 100 older adults. The five who scored highest and the five scoring the lowest, together with the five nearest the median score were selected for narrative based interviews, focusing on issues of later life. Five older adults were also interviewed, having completed the resilience scale, who have participated in the “Narrative Care Program” at York Care Centre, a large nursing home in Fredericton, NB. This program, which provides residents the opportunity to tell their life stories to open and respectful listeners, assists them in dealing with a number of late-life developmental tasks: life review, meaning-meaning, death preparation etc. (Noonan, 2011). Interview data were analyzed in terms of narrative complexity, characterization, irony, Nova Scotia Centre on Aging Page 19 openness, flexibility etc and compared across resilience scores and with data from participants in the narrative care program. New Models of Delivery PROMOTING ORAL CARE IN CONTINUING CARE THROUGH A UNIQUE UNIVERSITY/COMMUNITY COLLEGE COLLABORATION IN NOVA SCOTIA Mary McNally, Dalhousie University; Marlene MacLellan, Nova Scotia Community College; Karen McNeil, Dalhousie University; Sandra Crowell, Atlantic Health Promotion Research Centre Background: The Oral Care in Continuing Care research project used a participatory approach to engage personal care providers, nurse managers and directors of care to develop, implement and evaluate a comprehensive daily oral care program in three longterm care facilities in rural Nova Scotia. The primary output of this project was a comprehensive education and resource package entitled “Brushing up on Mouth Care”. Knowledge translation activities have led to the recognition of additional relevant audiences for these materials, including students at the Nova Scotia Community College (NSCC). NSCC delivers education to almost 65% of the Continuing Care Assistants who will work in Nova Scotia and 100% of Practical Nurses. Purpose: To profile a unique university-college partnership that developed between Dalhousie University and NSCC as a result of this research project. Results: NSCC’s expertise in training for the continuing care sector and commitment to research collaboration has resulted in: a formal introduction of enhanced mouth care education for CCAs and LPNs in all campuses across the province; implementation of “hands on” demonstration resources (i.e., head and neck mannequins, resource manuals and toolkits) in personal care laboratories; development and submission of learning resources and outcomes for provincial policy-makers; a strengthened partnership that is committed to ongoing facilitation of resources for other educators as well as for care providers already working in continuing care. Conclusions: The lessons learned, materials and resources arising from this partnership have implications for dissemination to other relevant education programs. A NEW MODEL OF DEDICATED PRIMARY CARE PHYSICIAN AND TEAM APPROACH FOR LONGTERM CARE FACILITIES. PRELIMINARY FINDINGS OF A MIXED METHOD STUDY Emily Gard Marshall, Dalhousie Family Medicine; Michelle Boudreau, Dalhousie Family Medicine; Fred Burge, Dalhousie Family Medicine; Barry Clarke, CDHA/Dalhousie Family Medicine This mixed method study of Care by Design, a coordinated model of dedicated family physician and team approach in long term care facilities (LTCF), evaluates the structures, processes, and outcomes of care. Several indicators of care and outcomes are measured in ten Capital District LTCF pre- and post-implementation (Sept-Feb 2008-9/2011-12) through reviews of acute care, LTCF and Emergency Health Services (EHS) charts. We also explore how the model is being experienced by multiple stakeholder groups (i.e., residents/families, physicians, administrators, extended care paramedics [ECP], and nurses) through qualitative inquiry. Framework analysis using Atlas.ti and triangulation data model will be used. Nova Scotia Centre on Aging Page 20 Preliminary qualitative findings show communication among care team members are augmented by increased family physician accessibility. Use of a comprehensive geriatric assessment has improved the ability of family physicians and ECP to make clinical decisions. Delivery of primary care is reported to be easier within the LTCF with a perceived reduction in transfers to emergency departments (ED). EHS data shows 451 calls during the pre-implementation period with 352 of those calls resulting in a transfer to the ED. During the post-implementation period there were 652 calls with 228 resulting in a transfer to ED and 305 resulting in care provided on site by ECP and the care team. In addition, of those transfers to ED, many are facilitated by ECP and the care team to reduce wait times in acute care. RESULTS OF TWO STUDIES ON A NOVEL PARAMEDIC-LONG TERM CARE PROGRAM Jan L Jensen, Emergency Health Services Nova Scotia/Dalhousie University; Andrew H Travers, Emergency Health Services Nova Scotia/Dalhousie University; Darrell J Bardua, Emergency Health Services Nova Scotia; Thomas Dobson, Emergency Health Services Nova Scotia; Bruce Cox, Emergency Health Services Medical Communications Center; Ed Cain, Dalhousie University; Robert Merchant, Emergency Health Services Nova Scotia; Jennifer McVey, Emergency Medical Services/Dalhousie University; Raewyn Bassett, Dalhousie University; Stephen Leadlay, Emergency Health Services/Dalhousie University; Alix JE Carter, Emergency Medical Services/Dalhousie University. Background: Long-term care (LTC) patients with acute illnesses or injuries are usually sent to emergency departments (ED) by ambulance. In a recently implemented Extended Care Paramedic (ECP) program, specially trained paramedics collaboratively manage LTC patients on-site. Objective: To report on two recently completed studies. Methods: Study One was a pilot study in which dispatch determinants and transport dispositions were collected for Halifaxregion LTC patients managed by ECP versus emergency crews. Unexpected relapse emergency calls within 48 hours for patients not transported for a related reason (‘bounceback’) was determined. Study Two was a qualitative study which identified insights gained and lessons learned during implementation and operation of the program, and explored the experiences of the ECPs in this novel role. Results: In Study One, 238 calls were received; 140 attended to by ECP (58.6%) and 98 by emergency paramedics (41.2%). The three most frequent dispatch determinants were the same for ECP and emergency paramedics. Transport outcomes for ECP calls were: 98 treat and release (70.0%), 9 urgent ambulance transport (6.4%) and 33 ECP-arranged transfer (23.6%). Transport outcomes for emergency paramedic calls were: 21 no-transport (21.4%), 77 transport to ED (78.6%). Six bounce-backs occurred after ECP treat and release (6.1%), and none after emergency paramedics non-transport. In Study Two, Twenty-one participants took part in four homogeneous focus groups. Key themes identified were: [1] program implementation, [2] ECP process of care, [3] communications, [4] end of life (EOL) care. Conclusion: In these two exploratory studies, it was discovered ECP involvement in LTC calls reduced transports to emergency with low bounce-back, that the ECP program has implications for paramedic education and system operations, and ECPs have a role to play in EOL care, which is novel for paramedic practice. Nova Scotia Centre on Aging Page 21 Family and Friend Caregiving SESSION THEME - Family and Friend Caregiving SESSION DATE AND TIME - Thursday, November 22 (3:30-5:00 pm) ROOM LOCATION - TBC MANAGING IN-HOME ELDERCARE: TRANSLATING KNOWLEDGE THROUGH RELATING Lynn Jansen, University of Saskatchewan; Carol McWilliam, University of Western Ontario; Dorothy Forbes, University of Alberta; Cheryl Forchuk, University of Western Ontario Limited investigation has addressed the process of knowledge translation (KT) to manage inhome eldercare for chronic conditions such as urinary incontinence (UI). Although UI can be managed conservatively, it is a principal reason for the breakdown of family-care and care recipient admission to long-term care. As well, Canadian families sustain annualized inhome UI expenditures of $2.6 billion. This grounded theory study explored the process of KT, building on a phase one phenomenological study that illuminated social interaction as an important component of family caregivers’ learning about UI. Using theoretical sampling techniques, in-depth interview data were collected from 23 family caregivers, homecare recipients, and interdisciplinary homecare providers who were registered nurses, therapists, social workers, and personal care workers. Constant comparison and Glaser’s analysis criteria were used to create the substantive theory of Translating Knowledge Through Relating. The core process and sub-processes of this theory that included developing comfort, easing into working relationships and facilitating knowledge exchange suggested that bi-directional relational interactions are interlinked with tacit and experiential knowledge. These findings contrast with traditional educational approaches of didactic transfer of information and afford understandings about how relational practice is necessary to foster social construction of KT. Insights gained may help in evolving policy that supports family-centered KT strategies related to the co-creation and co-facilitation of evidence for chronic care. The practical application of this work may constitute an important component of promoting health as a resource for everyday living with UI and minimize costs associated with adverse UI-related outcomes. CREATIVITY AND CARE-GIVING IN NEWFOUNDLAND: AN ARTS-BASED INQUIRY INTO THE RELATIONSHIP BETWEEN CREATIVITY AND HEALTHY AGING Megan Morrison, Memorial University of Newfoundland This research looks at the benefits of creative engagement for caregivers of individuals with dementia. The objective includes exploring arts-based methods as a supportive intervention for care-givers, and as a beneficial research tool. The methods include an interview, a freeform journal, and three creative care-giving themed workshops. The anticipated outcome of this project is for the care-givers to be able to share their creative pieces with the larger community and to experience benefit from creative skills. The presentation will include an outline of the project and its background, a presentation of images and profiles of participants, and an overview of the initial findings from the analysis. Nova Scotia Centre on Aging Page 22 "THERE WAS AN OLD WOMAN": GENDER ANALYSIS IN STUDIES OF AGING AND ELDER CARE Susan Bradley, Carleton University; Pat Armstrong, York University; Hugh Armstrong, Carleton University; Albert Banerjee, York University Although it is widely agreed that gender matters in issues of aging and elder care, how to conceptualize and account for gender in aging and elder care research, policy and practice is widely disputed. This paper draws upon the research –in-progress from an international comparative study of promising practices in long-term residential care to learn from three interdisciplinary approaches to gender analysis and assess their strengths and weaknesses for studies of aging and elder care. Drawing on theories of intersectionality, de-construction and critical realism, this paper outlines an approach-in-development that aims to produce contextualized gender analyses that keep the constraints of research, policy and practice environments in mind. With an explicit goal of contributing to a broad range of equity and social justice aims, this dialectical approach moves between evidence and theory to produce grounded and doable interdisciplinary gender analyses that can support research, policy and practices. A matrix for thinking about, planning and producing this kind of gender analysis is provided. SUPPORTING FAMILY CAREGIVERS: CANADA'S INVISIBLE HEALTHCARE SYSTEM Sue Kelly, We Care Home Health Services Life expectancies are increasing and Canadians are staying in the work force longer. These working Canadians are facing challenges outside of balancing their career obligations. They may be in the position of supporting their adult children, while witnessing their aging parents experience greater healthcare needs, cope with higher levels of chronic and complex diseases and, as such, require more care and assistance. These family caregivers may fall into the role with no training, support or respite. An estimated four to five million Canadians provide care for family members, contributing to an estimated $5 billion in unpaid labour annually. Over the years, we have witnessed an alarming trend among family caregivers – many find the role to be emotionally, physically and financially overwhelming. Concerned by this, we responded by creating practical information resources: the Being a Family Caregiver Guide, Get Going to Keep Going Guide and our Personal Caregiver Assessment tool - to provide caregivers with information and resources to take care of themselves. Additionally, we commissioned a survey to further examine Canadians’ attitudes and thoughts around their preparedness for undertaking a family caregiving role. This presentation will highlight results of the surveys as well as demonstrate practical use of the tools. The presentation will include interactive group work in which real life case studies will be analyzed. Insights on caregiver stress will be shared from a recorded podcast, health and safety tips will be highlighted through digital video and all attendees will be provided with our educational guides. Diverse Approaches: Gender and Frailty OLDER WOMEN'S EXPERIENCES WITH AND VIEWS OF HEALTH CARE Hazel McRae, Mount Saint Vincent University Nova Scotia Centre on Aging Page 23 Despite the fact that women constitute the majority of the older population, and older women interact more frequently with physicians and the health-care system than older men and younger persons, knowledge and understanding of older women’s experiences with health care is surprisingly limited. The main objective of this study was to explore older women’s health- care experiences, perceptions, and beliefs, and the extent to which they are satisfied with the care they receive. This research was guided by a symbolic interactionist theoretical framework and insights derived from feminist theory. In-depth, face-to-face, interviews were conducted with 23 women aged 55 years and older, all of whom lived in the province of Nova Scotia. The findings reveal that most of the women adopt a functional approach in their interpretation of what “good health” means to them, although some do make reference to mental health and quality of life as well. The vast majority of the women are very satisfied with their relationship with their physician; they are less satisfied with their experiences with specialists. Most of the women rate the health-care system as “good,” and most are relatively satisfied with the care they themselves have received, however, wait times, inadequate in-home support, and too few specialists are among a number of the health-care concerns expressed. Based on the women’s own ideas, the paper offers suggestions about ways in which the existing health-care system could be improved so that older women’s health-care needs and concerns could be more adequately addressed. “I WILL SLEEP WHEN NIGHT FALLS”: A FILM ABOUT A DAY IN THE LIFE OF AN OLDER WOMAN Olga Theou, Dalhousie University Research for my PhD project, “Physical Function During Performance-Based Tasks and Throughout Daily Life. Is It Different Across Levels of Frailty?” was conducted in a rural area of Greece. After screening 53 community-dwelling older women for frailty, I fitted them with four devices (accelerometer, HR monitor, EMG device, and GPS watch) in an attempt to “quantify” their daily life. The resulting data were published in scientific peer-reviewed journals, but a reader of these quantitative studies would not be able to see the actual daily activities of these women nor hear their thoughts on their daily lives. I created a film inspired by my experiences with these women, and what they chose to share with me beyond my scientific research questions. The short film (approx. 21 minutes), entitled “I Will Sleep When Night Falls”, documents a day in the life of an older Greek woman, focusing on activities and objects that the participants in my study thought were most important. I feel that this film complements the objective distance of my PhD dissertation, in creating a medium to give voice to those typically unheard. WIDOWERS DO HAVE FRIENDS: THE CHANGING NATURE OF MALE-TO-MALE FRIENDSHIPS Deborah van den Hoonaard, St. Thomas University; Kate Bennett, University of Liverpool There is relatively little research focusing on older widowers' friendships and it is commonly assumed that older widowers do not have close male friendships. This paper examines the nature of widowers' friendships with other men. The data are taken from qualitative interviews with 66 British and 26 North American older widowers. The results suggest that male-to-male friendships are not uncommon but that their nature is more hidden than in Nova Scotia Centre on Aging Page 24 women's friendships. A number of themes emerge from the data. Men have friendships through common interests. They are characterised by doing things together side-by-side rather than face-to-face. There is evidence of homophily, i.e. Men being friends with people like themselves. The British men talked, too, counter to our expectations, about life-long friendships and close supportive friendships. On the other hand, the North American men talked about friendships without firm commitments that allowed for spontaneous, unplanned activities. The nature of these two ways of being friends is explored in detail, with a focus on their function, on reciprocity and on cross-cultural similarities and differences. Finally, the hidden nature of close male-to-male friendships is discussed in relationship to the preservation of masculinity. 5:30-8:00 pm We are pleased to present the: Reception & Kathryn Allen Weldon Public Lecture, “WHY HAVE NONE OF THE NEW ALZHEIMER’S DRUGS WORKED?” by Dr. Kenneth Rockwood, Dalhousie University Friday, November 23, 2012 09:00-10:15 am PANEL: MULTI-PERSPECTIVE LOOK AT DEMENTIA Sultan Darvesh, Melissa Andrew, Hazel MacRae, Ardra Cole Moderator: Lloyd Brown, Executive Director Alzheimer Society of Nova Scotia Aging is multi-dimensional and so are the issues and challenges associated with an aging population that has a high prevalence of dementia. This multi-perspective panel on dementia will introduce conference participants to the diversity in perspectives on dementia, will showcase regional leadership in dementia research and will encourage attendees to explore potential connections between and across perspectives in dementia-specific research, policy and care practice. The panel features expertise in dementia research from four distinct perspectives: 1) clinical/biomedical; 2) health services and applied social sciences; 3) humanities-based research; 4) arts-informed research. Each panelist will offer a distinct angle on the meaning of dementia, spanning from medicine to healthcare providers and professionals, to the person with dementia, to the ways the relations between these diverse perspectives and experiences are mediated through artistic expression. In introducing participants to the diversity of perspectives on dementia, this panel has the potential to expand awareness and understanding of the complexity of an increasingly important issue facing continuing care and health systems and convey to participants the value of considering a holistic approach to issues in aging. Nova Scotia Centre on Aging Page 25 10:45-12:15 am Oral Presentations Session D Using a Cultural Lens THE AFRICAN NOVA SCOTIAN EXPERIENCE AT END OF LIFE Victor Maddalena, Memorial University; Wanda Thomas Bernard, Dalhousie University; Donna Smith, Cancer Care Nova Scotia Background: On the spectrum of aging, the period known as “end of life” is an underexamined area of inquiry, particularly in Nova Scotia’s Black community. Methods: Our research team partnered with the Health Association of African Canadians, a community based organization, to conduct three studies examining of end of life care in Nova Scotia’s Black community. Qualitative research methods, including participatory action research, were used to explore various aspects of the end of life experience, including the experiences of caregivers, the use of complementary and alternative medicine, their knowledge of palliative care services and the role of spirituality. Significance: Our research represents the first studies examining end of life care in the African Canadian community in Canada. Findings: For many African Canadians end of life is characterized by care provided by family in the home setting and limited access to health services, in particular palliative care services. Spirituality and close kinship bonds play an important role in terminal illness and end of life care. Equitable access to palliative care services remains an elusive goal, due in part to a lack of knowledge of available services, a lack of culturally competent palliative care services and systemic racism. Policy Implications: Palliative and end of life care services need to understand and support the preference of African Canadian families to provide end of life care in the home setting. There is a need to further engage Black communities and palliative care services in developing culturally appropriate palliative care services. THE HEALTH STATUS OF ANGLOPHONE SENIORS IN QUEBEC AND FRANCOPHONE SENIORS IN THE REST OF CANADA: SIMILARITIES, DIFFERENCES AND COMPARISON WITH THE GENERAL CANADIAN POPULATION Hubert Alimezelli, University of Saskatchewan; Anne Leis, University of Saskatchewan; Chandima Karunanayake, University of Saskatchewan; Wilfrid Denis, University of Saskatchewan Introduction: Language barriers have been shown to be a deterrent to seeking health services that may be preventive. Studies emphasize the importance of speaking one’s own language with regards to health issues. Objectives: #1: Identify some of the major determinants of health for official language minority seniors #2: Compare minority Francophone seniors’ health determinants with those of their Anglophone counterparts and with those of the general population of Canadian seniors Methods: The 2006 post-census Survey on the Vitality of Official-Language Minorities (SVOLM) carried out by Statistics Canada is used as well as the 2007 Canadian Community Health Survey (CCHS). The SVOLM will help assess factors associated with the self-rated health of minority Francophones. The CCHS will complement the SVOLM and allow for comparability with the general population. Statistical analyses such as descriptive, univariate, and multiple linear regression analyses are carried out. Results: Official language minority seniors in Quebec Nova Scotia Centre on Aging Page 26 and outside of Quebec share a similar profile in terms of the determinants of their self-rated health but there are a few striking differences for example with regards to visibility, sense of belonging, and vitality of minority community. The descriptive aspect of this study confirms the findings of other studies that show that people in a minority situation have a poorer selfrated health than the majority population but multivariable analyses fail to demonstrate such an association. Conclusions: New sampling approaches and new analytical methodologies need to be considered when dealing with official language minority populations. WORKING TO DEATH: DIVERSE EXPERIENCES OF ECONOMIC SECURITY AMONG OLDER IMMIGRANTS Natalie Weiser, York University; Nancy Mandell, York University; Meg Luxton, York University; Valerie Preston, York University The economic security of older immigrants in Canada is gendered and racialized with women and minorities reporting lower average incomes and fewer assets than other seniors. On average, immigrant seniors also have less economic security than the Canadian-born, however, the experiences of immigrants are very diverse. We explore how gender and ethnoracial background influence the economic security of immigrants using information from focus groups with seniors from diverse ethnoracial groups in Toronto and Peel region. The focus group transcripts describe the demographic characteristics of participants, relevant aspects of their migration history and their current family and economic circumstances. Many seniors reported economic vulnerability; social isolation; racial barriers to integration; language barriers; intergenerational conflict; heavy family responsibilities; and mental health issues. The findings confirm that the majority of immigrant seniors face economic challenges caused by the difficulties of paying high living costs with low incomes and they confirm the diverse experiences of immigrant seniors. A minority of participants who have had success in the Canadian labour market describe themselves as economically well off and secure. Unexpected and substantial gender and ethnoracial differences also emerge. Even well-established and successful immigrants are fearful about their economic security as they age. Addressing Emerging Health Conditions GETTING LONG IN THE TOOTH: PLANNING FOR FUTURE ORAL HEALTH NEEDS IN NOVA SCOTIA Debora Matthews, Dalhousie University; Martha Brillant, Dalhousie University; Mary McNally, Dalhousie University; Joanne Clovis, Dalhousie University Purpose: To determine differences in the oral health status and care needs of the “baby boomer” generation and the current seniors cohort, for future service planning and policy creation. Background: An epidemiologic survey measured the clinical oral health status of two cohorts of adults (age 45-64 and ≥65), living independently in rural and urban Nova Scotia. The survey comprised a telephone survey and clinical examination. The cohorts were compared for differences in oral health status and predictors of poor oral health. Results: 747 adults Nova Scotia Centre on Aging Page 27 (n= 411 aged 45-64; n= 336 aged ≥65) completed the survey. The younger cohort was less likely to be edentulous (no natural teeth) (2.6% vs 15.7%) and had more natural teeth (mean 22.1 vs 15.1) than the older. As a proportion of retained teeth, the older cohort had more filled crowns (51% vs 45%) and roots (12% vs 5%). Among those with natural teeth, the older cohort had higher rates of periodontal disease than the younger (71% vs 43%). Age ≥65 was a predictor of increased decayed/filled roots (OR 2.089) and periodontal disease (OR 3.367). Having chronic health conditions increased the odds of having decayed/filled roots for both age groups (OR 6.13, aged 45-64; OR 4.65, aged ≥65). Conclusions: Our evidence suggests that older people with natural teeth are more prone to oral disease than younger. Younger adults have more natural teeth than their older counterparts and are expected to retain much of this dentition as they age. Thus, treatment needs associated with maintaining oral health in this cohort will likely increase in severity and complexity, particularly for those who are more medically frail. EXPECTATIONS & REALITIES: SUPPORT AND CHALLENGES FOR STROKE SURVIVORS LIVING AT HOME Jared Clark, Memorial University of Newfoundland The challenges of living with stroke carry on long after leaving the hospital. Stroke survivors often depend on a myriad of supports to help them live independently, and the availability of these services varies widely. The demographic and geographic realities of Newfoundland & Labrador, as well as many other parts of Canada, make it difficult to provide continuing care and support for many stroke survivors living at home. Participants were aged fifty years or more, had recently experienced a first-time stroke, received some level of inpatient physical rehabilitation and were preparing to return home following discharge at the time of enrollment. In order to ensure that informed consent and full participation in the study were not problematic, individuals with notable cognitive or language impairment (as judged by treating therapists) were excluded at the time of referral. Participants were purposely recruited from both rural and urban communities in eastern Newfoundland. Semi-structured interviews with participants (and occasionally a family member/caregiver) were used to explore the themes of supports and challenges while living at home. An initial interview was carried out prior to discharge in order to examine the participants’ expectations and perceptions of how the transition back to life at home might be, while a second (follow-up) interview 6-12 months later examined the realities of living at home after stroke. A thematic analysis was carried out using interview transcripts, with particular focus on rural/urban divides, the roles of formal and/or informal supports, community-based services and potential gaps and barriers to independent living. AGING WITH HIV IN CANADA AND THE UK: A SCOPING REVIEW OF HIV POLICY APPROACHES Jacqueline Gahagan, Dalhousie University; Alexandra Hill-Mann, Dalhousie University; Eric Ross, Acadia University; Denver Lewellen, Dalhousie University Despite the advent of antiretroviral therapies in the mid-1990s, people living with HIV (PHA) continue to face complex and interrelated co-morbidities. As the numbers of PHAs living into older adulthood continue to increase, many present with unique health and social needs Nova Scotia Centre on Aging Page 28 often seen among older, non-HIV infected individuals. However, current health policy mechanisms may act as barriers to care across the lifespan. The purpose of this study was to explore policies on HIV and rehabilitation services in Canada and the UK. An iterative, policy-scoping review of Canadian policies and related reports on rehabilitation (N=58) was conducted. A separate, modified policy-scoping review was conducted for similar documents in the UK (N=21). This literature was then evaluated by at least 2 reviewers using a coding scheme developed by the research team, employing frameworks of healthy aging and several determinants of health. Novel policy approaches were identified. The results of the scoping review indicate that few policies regarding rehabilitation services specifically referenced HIV, indicating a lack of policy awareness of the reclassification of HIV as a chronic illness. When HIV was referenced, it was generally discussed in terms incongruent with parallel policy discussions related to other chronic illnesses in aging populations such as cancer and diabetes. Our research suggests that HIV-specific considerations are required in order to ensure inclusive policy-making that is appropriate across the lifespan for PHAs. These considerations may also serve to reduce barriers to accessing rehabilitation programs and services for PHAs in terms of living healthy into older adulthood. Aging and Movement AGE-RELATED CHANGES IN THE NEUROMUSCULAR CONTROL OF TRUNK MUSCLES TO A DYNAMIC LIFTING TASK Adam Quirk, Dalhousie University; Cheryl Hubley-Lozey, Dalhousie University Healthy aging is associated with structural changes in the musculoskeletal and neuromuscular system, but also functional changes such as increased attention to voluntary movement. This over-planning of voluntary movements, combined with structural changes of the neural and musculoskeletal tissues around a joint, may result in altered motor patterns. If these age-related patterns are not successful in controlling excessive joint motion, an increased risk of falls, and/or musculoskeletal injuries may ensue. 12 older adults and 51 younger adults performed a dynamic lifting task (right to left) with instructions to minimize trunk motion. Trunk muscle response was measured using surface electromyography recorded at 12 bilateral trunk muscle sites (6 abdominal and 6 back). A principal component analysis model was used to characterise muscle amplitudes and waveforms, allowing for statistical analysis between muscles and groups. While motion between these two groups was similar, older adults utilized different muscle activation patterns relative to younger adults including: 1) higher amplitudes for both the abdominal and back muscles; 2) a shift from lateral abdominal activity to the lateral back muscles; 3) less increase in the activity of medial back extensors in response to the increased flexion moment. These results suggest that older adults utilize a strategy with higher ongoing muscle activity throughout the task, and fewer specific adjustments to the continually changing external moments. This increased muscle activity would result in increased lumbar compression, which may play a role in an age-related increased risk of developing low back pain. AGING AND THE BRAIN: IS REDUCED FUNCTION OF MEDIAL-FRONTAL CORTEX RESPONSIBLE FOR MOVEMENT DEFICITS IN THE ELDERLY? Olav Krigolson, Dalhousie University; Cameron Hassall, Dalhousie University Nova Scotia Centre on Aging Page 29 By the year 2015 it is speculated that over 30% of traffic fatalities will be caused by elderly drivers (McGee & Tuokko, 2003). Indeed, the number of movement errors that we commit on a day-to-day basis increases as we age. Obviously, there are a number of factors that contribute to this age related increase in movement errors – decreased musculature, changes in timing and coordination, and changes in the peripheral nervous system, for instance. However, another explanation that has yet to be explored is whether or not decreases in the functional efficacy of error evaluation systems within the brain contribute to the increased incidence of movement errors that are associated with aging. Here, we tested this hypothesis by having both young (age: 19-30) and older (age: 65-75) participants perform a computer based driving task while we recorded-event-related brain potentials (ERPs). In line with previous findings (Krigolson & Holroyd, 2006), we found that driving “errors” made by younger participants elicited a feedback error-related negativity (fERN), a change in the ERP associated with error evaluation within medial-frontal cortex. Interestingly, we found that for older participants, the fERN elicited by driving errors was reduced. Importantly, these data suggest that one of the contributing factors to the increased incidence of movement errors observed in the elderly may be a reduced ability to evaluate movement within the brain. We believe that this result could pave the way for future research and potential interventions to improve our ability to move as we get older. Getting Aging on the Agenda THE ELDERLY BODY AS TEXT AND ARGUMENT Yvonne Stephens, Kent State University In sociological and linguistic studies of elderly populations, scholars have explored how discourse can socially construct categories such as “old” (Coupland et al., 1991, 2009). The idea of old age may exist more in language than it does in physical reality. Yet scholars now are noting that social constructivism can go so far as to erase the body, whose lived experience can have physical realities including pain and fatigue that are hard to ignore (Siebers, 2008; Oberg, 1996; Twigg, 2004). These scholars make the call to bring the body back into the conversation to develop a fuller understanding of how both language and bodily reality compose the lived experience of individuals of a certain age. Taking up this call, I argue that language can be used to get at lived, bodily experience. Using qualitative research methods (Corbin & Strauss, 2008), I study individuals who take yoga classes at two senior centers in the Midwestern United States. I conduct focus groups and interviews with 12 people ages 60 to 80 and analyze their talk to understand the ways they perceive the body. In my presentation, I will discuss my study’s findings, which show that not only do participants use discourse to construct arguments about the aging body, but they also use the body as a text to persuade others. I make suggestions for how we can use the knowledge obtained from this study to better understand senior center clientele and to improve communication between senior-care professionals and their clients. Nova Scotia Centre on Aging Page 30 USING PARTICIPATORY ACTION RESEARCH (PAR) TO RESPOND TO AN INVITATION FROM EAST PRINCE SENIORS’ TO COLLABORATE TO ASSESS ONE PART OF THEIR SOCIAL ENGAGEMENT MODEL Judy-Lynn Richards, University of Prince Edward Island; Gloria McInnis-Perry, University of Prince Edward Island; Janet McIntyre, University of Prince Edward Island The purpose of this submission is to share with Atlantic researchers on aging our methodological experiences from exciting participatory action research (PAR) with seniors from the East Prince Seniors’ Initiative (EPSI). A PAR model promotes 1) research with, rather than on, participants and 2) action for social change (Hennink et al 2011;McIntyre 2008), each of which fits with EPSI’s social engagement model. EPSI specifically uses a social engagement model to endorse collaboration with stakeholders (community seniors, business, Government) to bring about the wellness, life-long learning and productivity of seniors to promote their sense of belonging and community membership through active participation in community activities (Baker et al 2009). To assess their model, EPSI stakeholders asked UPEI researchers to study the outcomes of one part of their model, the Walk for Wellness (WfW) program, which encourages seniors to engage in a healthy lifestyle (with access to senior/expert education sessions) for successful aging. Methodologically, we collaborated on how to measure the health outcomes and to document their social engagement experiences, dispensing with researcher-driven decisions/guidelines for seniors’ involvement. While our analyses are not yet complete, the lessons learned, thus far, include more respectful ways to engage in various tasks (decision making, outreach strategies, measurement) and relationship building (autonomy, independence, trust) within PAR. These lessons will allow us and our Atlantic colleagues to understand various components of successful aging, social engagement, health and health promotion (Sanchez 2008;Lindström & Eriksson 2005). BUILDING AN EVIDENCE-BASED FRAMEWORK FOR A NEWFOUNDLAND AND LABRADOR CENTRE ON AGING Leslie Cake, Memorial University; Carla Wells, Western Health; Kelli O’Brien, Western Health; Gail Wideman, Memorial University; M. Ploughman, Memorial University; S. Buehler, Memorial University; Linda Bowering, NL Seniors Resource Center Population aging is unprecedented, pervasive, enduring and has profound implications for societies worldwide. In many countries, aging research and policy development have been facilitated by the creation of Centres on Aging. CIHR currently lists 21 Canadian research centres and organizations investigating aging. Despite having one of the highest proportions of older adults in Canada, Newfoundland and Labrador (NL) is the only province without a research centre for aging. In 2009, the authors formed a province-wide, interdisciplinary and multi-sector (including academics and community) research team to develop an evidencebased framework for the development of a NL Centre on Aging. We identified a purposive sample of 10 Canadian research Centres on Aging (including the NS Centre) which varied in terms of geographic region, size, and research foci. In 2010, we visited the 10 Centres and conducted structured interviews with 38 key personnel including directors, research affiliates, and community representatives. The purposes of the site visits and interviews were to determine the evolution and current activities of the Centres visited and to use this Nova Scotia Centre on Aging Page 31 information to inform the establishment and operation of a NL Centre on Aging. Information was gathered related to the establishment, research, outreach activities, partners, staffing, funding, and management and governance structures of each Centre. Interviewees were also asked to describe lessons learned and to offer advice related to the above categories of information. The conference presentation will summarize and discuss the information gathered and recommendations for the establishment of a NL Centre on Aging 10:15-10:45 am Poster Presentations Session D Continuum of Care THE SENIOR LIFECYCLE PROJECT Robin Campbell, Acadia University; Glyn Bissix, Acadia University; Shilpa Dogra, Acadia University This research contributes to the extensive seniors exercise and health programming research literature by providing a community-based and active transportation perspective. The Senior Lifecycle Project, situated in Kentville, Nova Scotia, identifies where seniors live, what their living and lifestyle conditions are like, what opportunities are available in their neighborhoods and the Town for more active living, and importantly, what barriers exist. In essence the purpose of this research is to identify what physical, social and psychological barriers and opportunities exist to promote more active lifestyles and how these challenges differ over the calendar year, particularly in winter. Using a community development framework this project focuses on four key concerns of the senior population: health and wellbeing, financial security, transportation, and supportive communities. Methodologies used include focus groups with health professionals and seniors; motion detection data using the Body Media Sense Wear Pro 3 armband; and GIS mapping systems. This research considers how communities can effectively increase its emphasis from healthcare (sickness management) to health promotion. Please note that the research is still in the data collection stage, and results are expected by the time of the conference. THE IN-HOME FAMILY CAREGIVER’S EXPERIENCE OF KNOWLEDGE TRANSLATION Lynn Jansen, University of Saskatchewan; Carol McWilliams, University of Western Ontario; Dorothy Forbes, University of Alberta; Cheryl Forchuk, University of Western Ontario Research affords little insight into our understanding of family caregivers’ experience of knowledge translation (KT) related to urinary incontinence (UI) management for eldercare. Although UI can be managed conservatively within the home, it is a principal cause of the collapse of informal eldercare arrangements and care recipient admission to long-term care. Unpaid caregivers provide healthcare for 98% of older adult family members receiving homecare. Not only are both care recipient and caregiver health ultimately undermined by the strain of unsuccessful UI management, but also UI results in annualized in-home Canadian expenditures of $2.6 billion. The purpose of this study was to explore in-home family caregivers’ UI KT experience amongst interdisciplinary homecare providers. An interpretive phenomenological approach was used, foundational to a phase-two grounded theory study. Four caregivers who provide UI care to older adults were purposively selected from a rural homecare setting in Saskatchewan, Canada. Immersion and crystallization Nova Scotia Centre on Aging Page 32 methods were used to analyze in-depth interviews. KT was experienced as a process of working together/not working together within the contexts of homecare and personal attributes that facilitated or impeded KT. Insights suggest that social interaction, particularly within working relationships, is an important part of caregivers’ way of learning UI care and contrasts with traditional didactic professional transfer of information. This interpretive study enables the evolution of programmatic research, building knowledge in a previously unexplored topic area. Ultimately, research findings may inform in-home KT interventions, optimize the health of older people and their caregivers, and minimize UI costs and longterm care admissions. CHANGES IN THE USE OF GOVERNMENT-SUBSIDIZED HOME CARE BY OLDER CANADIANS WHO NEED ASSISTANCE Anne Binette Charbonneau, Université de Montréal; Janice Keefe, Mount Saint Vincent University; Jacques Légaré, Université de Montréal; Sam Vezina, Mount Saint Vincent University This research examines the evolution of government-subsidized home care utilization by Canadians 65 years old and older between 1996/97 and 2009. Previous research has observed a shift in subsidized home care towards acute home care at the expense of chronic home care services (Glenda Hawkins, 2005; Kathryn Wilkins, 2006). We investigate the patterns and predictors of home care usage by analyzing data from the 1996/97 National Population Health Survey (NPHS), the 2005 Canadian Community Health Survey (CCHS) and the Home Care Services module for Ontario of the 2009 CCHS. First, the population distribution by type of assistance (nursing care, personal care, housework, meal preparation, shopping, and other services) is presented. Next, a logistic regression is used to identify the predictors of home care utilization based on the Andersen and Newman’s Behavioral Model. Three points in time (survey years) are studied to determine how proportions and predictors evolved over time. The trend towards a greater use of nursing care and a change in home care users’ profiles observed in previous studies (early 2000’s) has been holding true in more recent years. For example, in Canada between 1996/97 and 2005, government –subsidized nursing care increased from 40% to 44% while housework decreased from 52% to 42%. Given the increased number of older Canadian expected to need assistance, our results demonstrate how our public system is adapting to increased demand. More attention to these trends is needed to better prepare to meet future care needs of older people. SERVICES AND PROGRAMS FOR OLDER RURAL WOMEN EXPERIENCING INTIMATE PARTNER VIOLENCE IN THE MARITIME PROVINCES Lori Weeks, University of Prince Edward Island; Colleen MacQuarrie, University of Prince Edward Island; Lorraine Begletym, University of Prince Edward Island; Kristal LeBlanc, Beausejour Family Crisis Resource Centre In this research, we focused on understanding the influence of both locality and age on the supports that women receive that can facilitate ending a relationship in which they experienced intimate partner violence. Rural women are different from their urban counterparts, partially because of the isolation of their communities. We currently know little Nova Scotia Centre on Aging Page 33 about these women and how existing programs and services influence their lives, and we need to gain further knowledge on how they understand their experiences, where they go for support, and the response and effectiveness of that support. The questions that guided this study are: 1) What initiatives currently exist in rural areas of the Maritime provinces to support older women who have experienced intimate partner violence? 2) How could these current initiatives be improved? We will present data from an environmental scan of policies, programs and services and 6 key informants interviews with representatives of public and nonprofit organizations in the Maritime provinces. In this presentation, we will summarize the results of our environmental scan highlighting the availability of programs and services in the public and non-profit sectors, with a specific emphasis on identified gaps for older women living in rural places. Results from the key informants will include an analysis of their evaluation of current programs and services and recommendations for change. It is clear that gaps in programs and services currently exist, and a great deal of work remains in order to meet the needs of older abused rural women in the Maritime provinces. SIBLING RELATIONSHIPS ACROSS THE LIFE-COURSE: BABY BOOMERS CARING FOR AN OLDER BROTHER OR SISTER Holly Smith, Mount Saint Vincent University; Janice Keefe, Mount Saint Vincent University Concern about who will care for the increasing aging population is becoming a major issue in Canada. Between 1946 and 1964, almost 10 million baby boomers were born in Canada and they began to turn 65 in 2011. With so many children born within a short timeframe, many of the boomers grew up with multiple siblings, each having a different relationship and a unique bond. This abundance of siblings may prove very valuable in the care demands of the future. Using tenets of social exchange and the life course perspective, this research will investigate the experiences of boomers who are the primary caregiver of a sibling who is aged 65 with a physical or mental acquired health condition and living in the community. Semi-structured qualitative interviews, guided by the constructivist paradigm, will be used to explore how sibling relations developed over the life-course and have affected the expectations and experiences of baby boomers as caregivers to their siblings in later life. Grounded Theory Methods will be used in an attempt to construct the stories of the participants in order to inform the area of sibling relationships of care in the later years. Coding techniques, including open, axial, and selective coding, aim to derive the most accurate story possible from each of the interviews. The results will highlight diversity within caregiving relationships and help to inform policies and practice that attempt to support older people with health care needs to remain in the community. ASSESSING THE IMPACT OF INCREASED DEMAND FOR CHRONIC CARE AND DECREASED SUPPLY OF CAREGIVERS: WE NEED A PLAN FOR THE FUTURE Samuel Vezina, Mount Saint Vincent University; Janice Keefe, Mount Saint Vincent University; Jacques Legare, Université de Montréal; Yann Decarie, INRS Canadians in need of ADL or IADL assistance for a long-term health problem or disability receive assistance from the formal network (government-subsidized and private sources), informal network (family, friends, neighbours) or both. Population aging and policy Nova Scotia Centre on Aging Page 34 emphasizing care at home point to an increase in demand for home care services. This research uses Statistics Canada’s LifePaths microsimulation model to project the number of older Canadians needing assistance and the amount of assistance needed from support networks between 2006 and 2031. Logistic regression parameters for characteristics associated with disability (2000/01 Canadian Community Health Survey) and the use of support networks (2002 General Social Survey) of Canadians 65 and older living in private households were applied in LifePaths to project future demand. Derived projections were developed to project the amount of weekly hours expected to be provided by each network. The population needing assistance will double between 2006 and 2031 (from 1.18 to 2.37 million). While this will mean an increase in demand for both formal and informal supports, the proportion having to rely exclusively on the formal network is projected to increase from 28% to 33%. Total weekly hours of assistance are projected to increase from 15.1 million to 29.3 million between 2006 and 2031, with formal hours showing the greatest increase (136%). Canada must prepare for an increase in the absolute number of human resources (formal and informal) that will be needed to provide care and governments must recognize that a greater proportion of assistance will be from formal sources. RETIREMENT DECISIONS AND OUTCOMES AMONG WOMEN CAREGIVERS WHO RETIRED TO GIVE CARE IN RURAL NOVA SCOTIA Jennifer Byrne, Mount Saint Vincent University; Áine Humble, Mount Saint Vincent University More research is needed on single women’s experiences of caregiving and how it relates to their retirement decisions and experiences. Furthermore, how moving to a rural area affects one’s experiences has not been explored sufficiently. Framed by the life course theoretical framework and socialist feminist theory, this qualitative study focused on single middle-aged women’s experiences of retiring to rural areas to give care to an older family member or friend, exploring both the decision to retire and the implications of the retirement decision. As part of a larger study on retirement and caregiving, six Nova Scotian women participated in semi-structured interviews. Participants were between 48 to 66 years old, had been retired between 6 months to just under 6 years, and had retired to care for aging parents (5) or a friend (1) between the ages of 77 to 88. Qualitative description (Sandelowski, 2000) guided the analysis. Key themes were: (a) caring from a distance incurred various costs, (b) family members were released from responsibilities, (c) the decision to retire was constrained rather than freely chosen, and (d) the loss of employment was felt personally, socially, and economically. Women who had lived and worked in rural areas as adults, rather than moving from an urban to a rural area, were particularly negatively affected financially. Understanding more about this process is important in the development of relevant government, institutional, and workplace policies. Policy suggestions for workplace, home care, and income security are discussed. THE AGE FRIENDLY WORKPLACE IN THE NON PROFIT SECTOR Veronica McNeil, Community Links ; Anna Wartacz, Community Links Nova Scotia has the oldest population in Canada. An ageing population is an ageing workforce. The labour force in Canada and in Nova Scotia will experience workers retiring at an unprecedented number, starting in 2012. Attracting and retaining older workers is a key Nova Scotia Centre on Aging Page 35 strategy recognized by the labour sector, including the non-profit sector. This sector is at particular disadvantage compared to other because it tends to have lower wages and fewer benefits available as an inducement to workers. Therefore, this project was designed to examine how to attract older workers to the non-profit sector in Nova Scotia, perhaps as a second career, and how to be age friendly workplaces in order to increase the sector’s capacity to retain older worker. During the course of the research 257 participants were engaged through on-line surveys, focus groups and a provincial forum. The resulting report presents a “Snapshot” of age friendly workplace practices and contains considerations for the non-profit sector organizations, the sector as a whole and for government in what needs to occur to support older workers to remain working to try something new as they consider retirement options. CAPTURING THE DYNAMICS OF A WORK DAY IN LONG-TERM CARE FACILITIES Jennifer Wong, Saint Mary's University; Kevin Kelloway, Saint Mary's University The long-term care sector in Canada is undergoing fundamental transformations. Yet, our understanding of how workplace demands affect caregivers’ health has not changed. Past research conducted has been mostly self-reports, which are susceptible to recall bias and fail to capture the complexity of a workday. The objective of this study is to facilitate a greater understanding of the stressors in long-term care work settings and their consequences using an ecological momentary sampling. This sampling method captures experiences in real-time, allowing us to ‘map’ reactions back to the antecedents. To supplement psychological measures of health, ambulatory blood pressure (ABP) monitors will assess caregiver’s physiological functioning. Moreover, the mediated role of emotion between stressors and health outcomes will be explored. A diary study accompanied by ABP measurements will be conducted with long-term care employees. Caregivers will wear the ABP monitors programmed to take hourly readings for a full day. After each reading they will fill out a diary entry consisting of items assessing workplace stressors, the emotions and recovery experiences associated with it. Data will be analyzed using multi-level modeling. The current study will contribute to the knowledge of the demands faced by caregivers and their health outcomes by using a unique combination of methodologies. A DAY IN THE LIFE… LEARNING ABOUT NURSING HOME RESIDENT QUALITY OF LIFE THROUGH PARTICIPANT OBSERVATION Robin Stadnyk, Dalhousie University; Thea Brown, Mount Saint Vincent University; Marie Warner, Dalhousie University; Grace Warner, Dalhousie University This poster shares preliminary results of case study research examining resident quality of life in relation to 3 different models of nursing home care in Nova Scotia. The purpose of this poster is to explore the role of participant observation in case study research. The theoretical framework driving the research, developed from a review of literature on models of care, links aspects of models of care to 5 components of quality of life: relationships, activities, autonomy, affect and home-likeness of the facility. Six qualitative case studies are being conducted, 2 each in 3 nursing homes representing 3 different models of care. Each case study includes resident, staff, and family member interviews, activity monitoring, and Nova Scotia Centre on Aging Page 36 participant observation. The participant observation comprises of up to 4 hours of observation of the resident's day to day life in a 10 hour period. Three different observations of each resident will conducted over an 8 month period. Residents are of diverse ages and functional/ cognitive status. This poster reports on the first 2 data collection periods, and describes 1) the process of data collection and analysis; 2) the experiences of the participant observer and 3) the contributions of the participant observations to the findings of the case studies regarding resident quality of life in relation to models of care. Implications for the future studies involving participant observation in nursing homes will also be discussed. ASSESSING THE PHYSICAL ENVIRONMENT OF ADULT DAY PROGRAMS FOR PERSONS WITH DEMENTIA Thea Brown, Mount Saint Vincent University; Janice Keefe, Mount Saint Vincent University This research assesses physical environments of adult day programs in Nova Scotia in terms of their appropriateness for persons with dementia. Researchers have found that when physical environments are well designed, they can significantly compensate for decreased cognitive ability and can impact the behavior and wellbeing of people with dementia. The Personal Environment Fit Model (Lawton & Nahemow, 1973) is used in this study as it recognizes that behavior and affect are outcomes of a person’s level of competence interacting with an environment’s level of press. This presentation will report the reliability and validity tests of an adult day program physical environment assessment tool (ADPPEAT) designed by the author and will assess the extent to which adult day program environments in Nova Scotia implement the key physical environment design principles. All adult day programs (N=32) are included in the cross-sectional design. A sub-sample of four centres are re-assessed for reliability purposes. Descriptive information will be presented on characteristics of the programs: type and number of clientele, hours of operation, services offered, funding sources and information on support networks. The Nova Scotia government recently increased its support of adult day programs and their participants. The results of this research will demonstrate how these services are supporting the needs of the dementia population; the relative importance of the design in creating a dementia friendly physical environment in community based services and provides a baseline for future research. Such evidence will help to inform future decisions around adult day care policy. (DE)CONSTRUCTING PERSONHOOD: A CRITICAL REVIEW OF THE LITERATURE ON PERSONCENTRED DEMENTIA CARE Katie Aubrecht, University of Toronto and Nova Scotia Centre on Aging Current research on dementia privileges a biomedical perspective which views dementia in terms of impairment, disorder, deficiency and dysfunction. Left unexamined, a biomedical perspective can work to negate the meaning and value of a life lived with dementia, perpetuate ageism and ableism, and rationalize such dehumanizing practices as neglect, segregation, and physical and chemical restraint. Person-centred models of care increasingly recognized as offering an alternative perspective that can protect and advance the dignity and autonomy of ‘persons with dementia’. Person-centred care promotes a social perspective that encourages reflexive understanding of social categories and definitions of Nova Scotia Centre on Aging Page 37 situations, as well as economic, political and cultural contexts [1, 2]. Although understanding the social construction of dementia is central to person-centred dementia care [3], assumptions concerning impairment are often left unexamined. In this presentation I share the results of a comprehensive review and textual analysis of literature on personcentred dementia care conducted in 2011-2012. Drawing on critical disability studies theory, I consider how dementia continues to be treated as a biomedical problem, albeit one which resides in individuals who deserve to be recognized as persons. I consider how definitions of personhood in textual representations of dementia care do not only provide access to the current treatment and interpretation of dementia, but also what it means to be a ‘person’ and a have a voice within contemporary neoliberal contexts. This presentation concludes with a reflection of the promise of research that brings critical disability studies and aging and caregiving studies into conversation. References: [1] Bartlett, R. & O’Connor, D. (2007). From personhood to citizenship: Broadening the lens for dementia. Journal of Aging Studies, 21, 107-118. [2] O’Connor, D., Phinney, A., Smith, A., Small, J., Purves, B., Perry, J., Beattie, L. (2007). Personhood in dementia care: Developing a research agenda for broadening the vision. Dementia, 6(1), 121-142. [3] Kitwood T. (1997). Dementia reconsidered: The person comes first. Open University Press, Buckingham. 12:15-2:00 pm Keynote Speaker: Susan Kirkland, Dalhousie University AGING INTO THE FUTURE: GROWING OLD WITH THE CANADIAN LONGITUDINAL STUDY ON AGING Over the next twenty years, the Canadian Longitudinal Study on Aging (CLSA) will generate a wealth of information that will contribute to the advancement of the science of aging and policy development in a changing world. The CLSA will collect information from 50,000 men and women on the biological, clinical, psychological, social, and economic aspects of their lives in order to understand how, individually and in combination, they influence the maintenance of health and well-being, and the development of disease and disability as people age. The CLSA will be one of the most comprehensive studies of its kind undertaken to date. Its large sample, multidisciplinary focus, and longitudinal design will provide research opportunities unprecedented in Canada and internationally. In 2009 the CLSA partnered with Statistics Canada to develop the Canadian Community Health Survey (CCHS) in Healthy Aging and launch the CLSA. Recruitment of the Tracking cohort began in 2010 with funding from the Canadian Institutes of Health Research. In 2011, with funding from the Canada Foundation for Innovation, the infrastructure for eleven Data Collection Sites across Canada was established to conduct health assessments in the Comprehensive cohort. In 2012, recruitment of the Comprehensive cohort began. The objectives of this presentation are to: 1) Provide an update on CLSA progress and milestones achieved; 2) Give a detailed account of the data collection procedures within the CLSA that will allow researchers to appreciate its scope and potential as a platform for the study of aging; 3) Describe the process for future data access by the research community. Nova Scotia Centre on Aging Page 38