Lecture 5 Post Partum Period 2015 Students
advertisement

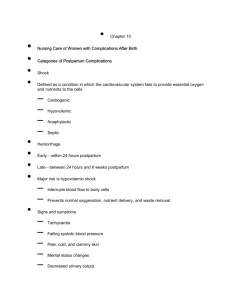
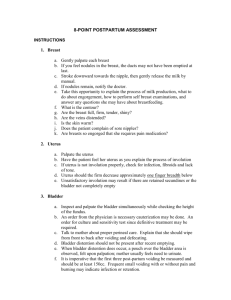
Post Partum Period Chapters 15 & 16 High Risk Chapter 22 Mary L. Dunlap MSN Fall 2015 Post Partum • Begins immediately after child birth through the 6th post partum week • Reproductive track returns to nonpregnant state • Adaptation to the maternal role and modification to the family system Safety for Mother and Infant • Prevent infant abductions • Check ID bands • Educate mother about safety measures Infant ID Bands Security Band Clinical Assessment • Receive report • Review Antepartum and Intrapartum history • Determine educational needs • Consider religious and cultural factors • Assess for language barriers Post Partum Assessment BUBBLE-EE • • • • Breast Uterus Bladder Bowel • • • • Lochia Episiotomy Extremities Emotion Vital signs • • • • Temperature Pulse Blood pressure Respirations Pain Assessment • Determine source/location and pain level • Interventions- based on pain • Document location, type, pain level and intervention • Reassess in 30 min and document pain level Breast Initial assessment • Inspect for size, contour, and asymmetry • Note if nipples are flat, inverted or erect Ongoing assessments • Check for cracks, redness, or fissures • Engorgement • Mastitis Breast Care Lactating Mother • • • • Supportive bra Clean areola & nipples with water Air dry Express colostrum apply to areola & nipple • Change breast pads frequently Breast Care Non-Lactating Mother • • • • Avoid stimulation Wear support bra 24hrs Ice packs or cabbage leaves Mild analgesic for discomfort Assessment of Uterus • After birth midline between umbilicus and the symphysis pubis • Within 1h returns to the umbilicus • Descends 1 cm/day • Consistency- firm/boggy • Height- measured in fingerbreadths • Fundal massage procedure 22.1 p 753 Nursing care • Boggy fundus- massage until firm • Medications- Pitocin, Methergine, Hemabate • Teach new mom to massage her fundus Afterpains • Intermittent uterine contractions due to involution • Primiparous-mild • Multipara- more pronounced • Breastfeeding causes an increase in contractions due to release of oxytocin Nursing Interventions • Patient in a prone position and place a small pillow to support her abdomen • Ambulation • Medicate with a mild analgesic Bladder • Monitor for bladder distention and displacement of uterus • Assess for voiding difficulty • Monitor output • Postpartum Diuresis Nursing care • Encourage frequent voiding every 4-6 hours • Monitor intake and output for 24 hrs • Early ambulation • Void within 4-6 hrs after birth • Catheterize if unable to void Preventing Stress Incontinence • Vaginal delivery causes direct pelvic muscle trauma and disruption of fascial support contributing to the development of urinary stress incontinence. • Prevention strategies: Loss weight, avoid bladder irritates, decrease fluid intake • Kegal exercises Teaching Guidelines 16.3. 502 pg Bowel • • • • Relaxin depresses bowel motility Progesterone ↓ muscle tone Diminished intra-abdominal pressure Incontinence if sphincter lacerated (4th degree) • Spontaneous BM 2nd to 3rd post partum day • Normal bowel pattern 8-14 days Nursing Care • • • • • • Increase fiber in diet 6-8 glasses of water or juice Stool softener- especially 4th degree Laxative Sitz bath for discomfort Medications for hemorrhoids Lochia • • • • Rubra Serosa Alba Documentation Lochia Assessment Scant • 1-2 in • About 10 ml Small • 2-4 in • About 10-25 ml Moderate • 4-6in • About 25-50 mL Heavy • Saturated pad greater than 6 in • About 50-80 mL within 1 hr. Nursing Care • Educate on the stages of lochia • Increase in lochia, foul odor or return to Rubra lochia is not normal • Change Peri pad frequently • Peri care after each voids to decrease risk of infections Episiotomy • 1-2 inch incision in the muscular area between the vagina and the anus • Assess REEDA • Lacerations • Episiotomy care Nursing Care • • • • • Peri care Ice packs Dry heat Topical medications Sitz bath Teaching guidelines 16.1 p. 499 Extremities • Increases the risk of thromboembolic disorders • Risk factors venous stasis, altered coagulation and vascular damage due to birth process increase risk of clot formation Assess for Thrombosis • Homan’s sign • Assess extremities • Monitor for signs of PE Post Partum Assessment • Post Partum Assessment Video Emotional Status • Bonding is a vital component of the attachment process. It helps establish parent infant attachment and a healthy loving relationship. • Bonding takes during the first 30 to 60 min. after birth Emotional Status Bonding process helps to lay the foundation for nurturing care • Touch- skin to skin • Eye contact • Breastfeeding • Engrossment • Factors that interrupt bonding Engrossment Seven Behaviors • Visual awareness • Tactile awareness • Perception NB is perfect • Focus is on NB • Aware of NB’s distinct features • Extreme Elation • Increase sense of self esteem- proud Tactile Awareness Bonding Factors that may interfere with bonding process • Stress over finances • Lack of support • Cultural beliefs • Interruption of process-sick child NICU Transitioning to parenthood • • • • Difficult and challenging Provide emotional support Accurate information Nursing goal create a supportive teaching environment Assuming the mothering role Rubin’s three phases • Taking –in • Taking –hold • Letting-go Taking in Phase Fathers Development Process Three stages • Expectations • Reality • Transition to Mastery Maternal Physiological Adaptations Hematological System • Decrease in blood volume • Elevated WBC • Increased Fibrinogen Hormonal Levels • Estrogen and Progesterone decrease • Anterior pituitary → prolactin for lactation • Expulsion of the placenta- placental lactogen, cortisol, growth hormone, and insulinase levels decrease • “Honeymoon phase”- insulin needs decrease Neurological System • • • • Maternal fatigue Transient neurological changes Headaches Carpel tunnel improvement Integumentary System • Darken pigmentation gradually fades • Hair regrowth returns to normal in 612 months • Striae( stretch marks) fade to silvery lines Immune System Rubella • Administer to nonimmune mothers • Safe for nursing mothers • Avoid pregnancy for 1 month • Flu-type symptoms may occur Immune System • Rho (D) immune globulin • Mother Rh negative, infant Rh positive • Negative coombs’ test • 300 mcg of RhoGam within 72 hrs after delivery • Card issued to mother Reproductive System • Involution of uterus • Healing of placental site • Vaginal changes Menstruation and Ovulation Nonlactatating mother • Menstruation returns in 7-9 wks, can take up to 3mo. • First cycle may be anovulatory Lactating mother • Delayed ovulation and menstruation Musculoskeletal System • Relaxation of pelvic joints, ligaments, and soft tissue • Muscle fatigue and general body aches from labor and delivery of newborn • Rectus abdominis diastasis Postpartal Surgical Patient • Tubal ligation • Cesarean birth Breast Feeding • American Academy of Pediatrics (AAP) recommends infants be breastfed exclusively for first 6 months of life • Breastfeeding should continue for at least 12 months • If infants are weaned before 12 months, they should receive iron-fortified infant formula Breast Feeding • Optimal method of feeding infant • Breast milk- Bacteriologically safe, fresh, readily available • Milk transition: Colostrum, Transitional milk & mature milk • Breastfeeding benefits 18.2 p 583 • Nursing Care Plan 18.1 pg 587 Contraindications to Breastfeeding • Maternal cancer therapy/ radioactive isotopes • Active tuberculosis • HIV • Maternal herpes simplex lesion • Galactosemia in infant • Cytomegalovirus (CMV) • Maternal substance abuse Breast Feeding Keys to successful breast-feeding • Initiate first feeding within first hr. • No supplements • Feed on demand, unrestricted at least 8-12 feeds in 24hrs • Avoid artificial nipples • Mother and newborn to stay together Breastfeeding • • • • Cue signs Latch-on Assess for milk let down Scoring tool table 18.6 p 509 Cue Signs • Rooting Latch on • Open mouth gape • Infant tip of nose, cheeks and chin touching breast THE LATCH SCORING TOOL Parameters 0 Point 1 Point 2 Point L LATCH Sleepy infant No latch achieved Hold nipple in infants mouth to latch & suck Stimulate to suck Latches on rhythmic sucking A: Audible swallow none Few with stimulation Spontaneous and Intermittent T Type of nipple Inverted Flat Protruding C Comfort of nipple Engorged cracked bleeding sever discomfort Filling, reddened, small blisters Mild to mod. discomfort Soft nontender H Positioning Nurse must hold infant to breast Minimal assistance then mother takes over No help needed Breastfeeding Positions • Cradle hold • Foot ball • Side lying Cradle Hold Foot Ball Hold Foot Ball Hold Side Lying Breastfeeding • A newborns stomach is the size of a small marble and can hold 5-7 cc’s. This is matches the amount of colostrum produced • From 7-10 days it increases to the size of a golf ball and can hold 1.5 to 2 oz Breastfeeding • Newborns nurse on average 8-12 times/24hrs • Feed by cue signs about every 1-3 hours • Should have no more than one 4 hr period • Teaching Guidelines 18.4 pg.588 Milk Expression • Manually • Manual or handheld breast pump • Electric breast pump • Hand Express Manual Pump Electric Hand Held • Electric Pump Electric Pump Breast Milk Storage • Room temperature- 4 hrs • Refrigerator- 5-7 days • Deep freezer- 6-7 months Ineffective Breastfeeding • Incorrect latch-on • Inverted nipples • Breast engorgement Special Considerations • Sleepy baby- use gentle stimulate to bring to alert state • Fussy baby- use calming techniques • Slow weight gain- evaluate breastfeeding Formula Feeding • Formula preparation • Periodically check nipple integrity • Bottle preparation Teaching Guidelines 18.5 p. 591 Discharge Teaching • • • • • • Fundus and Lochia Episiotomy care Incision care Signs of PP infection- table 22.3 p 761 Elimination Nutrition Box 16.4 p 504 Discharge Teaching • • • • • • • Exercise- 16.2 p 501 Activity Pain management Sexual activity Contraception Blues Community resources Postpartum Women at Risk Chapter 22 Postpartum Hemorrhage • Blood loss >500 ml of blood after a vaginal birth • 1000 ml of blood after cesarean section • Major hemorrhage >2,500 mL • Transfusion of >5 units • Any amount of bleeding that places mother in hemodynamic jeopardy • Table 22.1 pg 748 Postpartum Hemorrhage • • • • • • • 5 T’s- factors associated with PPH Tone Tissue Trauma Thrombin Traction Table 22.2 pg. 751 Tone / Atony • Altered muscle tone due to overdistention • Prolonged or rapid labor • Infection • Anesthesia Tissue • • • • Retained placental fragments Uterine inversion Clots Subinvolution Trauma • Cervical lacerations • Vaginal lacerations • Hematomas of vulva, vagina or peritoneal areas Trauma Hematoma • Localized collection of blood in connective or soft tissue under the skin( caused by laceration to blood vessel) • Risk factors • Signs and symptoms • Management Thrombin • Disorders of the clotting mechanism • This should be suspected when bleeding persists without an identifiable cause Management of PPH • • • • • • • Frequent VS q 15 min times 1 hr. Fundal massage Administer medications Monitor blood loss for amount Maintain IV Type & cross match Empty bladder Fundal Massaging • Procedure 22.1 pg. 753 Uterotonic Drugs • • • • • Oxytocin (Pitocin) Misoprostol (Cytotec) Dinoprostone (Prostin E2) Methylergonovine maleate (Methergine) Prostaglandin (Hemabate) Drug Guide 22.1 pg.754 Management of PPH • Balloon Tamponade Catheter Post Partum Hemorrhage • PPH Simulation • PPH Noell Thromboembolic Conditions • Thrombosis (blood Clot) can cause inflammation of the blood vessel (Thrombophlebitis) which can cause Thromboembolism (obstruction of blood vessel) Assessment Superficial • Tenderness and pain in extremity • Warm and pinkish red color over thrombus area • Palpable- feels bumpy and hard • Increased pain when ambulating Nursing Care • • • • • NSAIDs for pain Bed rest elevate affected leg Warm compresses Elastic stockings No anticoagulants required Assessment For Deep Vein Thrombosis • • • • • • • Calf swelling Warmth Tenderness Pedal edema Diminished peripheral pulses Color blue Homan’s sign Nursing Care • • • • • • Bed rest Elevate effected leg Continuous moist heat TED hose both legs Analgesics PRN Anticoagulation therapy Thrombosis Patient Education • Anticoagulation Teaching Guidelines 22.1 pg. 758 • Eliminate risk factors • Continue using Compression stockings • Avoid constrictive clothing & prolonged standing • Danger signs Pulmonary Embolism • Abrupt onset: chest pain, dyspnea, diaphoresis, syncope, anxiety • ABC response Postpartum Infections • Temp of 100.4 or higher after the first 24 hrs. for 2 successive days of the first 10 PP days • Temp of 102.2 or greater within first 24 hrs.- sever pelvic sepsis Group A or B streptococcus Postpartum Infections • • • • • • • Endometritis Wound infection UTI Mastitis Septic Pelvic Thrombophlebitis Box 22.1 Risk Factors Table 22.3 pg. 761 signs & symptoms Metritis • Involves the endometrium, decidua and adjacent myometrium of the uterus • Lower abdominal tenderness or pain • Temperature • Foul-smelling lochia Nursing Care • Administer broad spectrum antibiotic • Provide analgesia • Provide emotional support Wound Infection • Sites- Cesarean incision, episiotomy and genital tract laceration • Drainage • Edema • Tenderness • Separation of wound edges Nursing Care • • • • • Aseptic wound management Frequent perineal pad changes Good hand washing Administer antibiotics Analgesics Urinary Tract Infection • • • • • Burning and pain on urination Lower abdominal pain Low grade fever Flank pain Proteinuria, hematuria, bacteriuria, nitrates and WBC Nursing Care • • • • • Frequent emptying of bladder Increase fluid intake Antibiotics Analgesics Peri care Mastitis • Infection of the breast (one sided) • Seen first 2 weeks after delivery • Most common organism staphylococcus aureus • Infected nipple fissure - to ductal system involvement- edema obstructs milk flow in a lobe- mastitis Mastitis Symptoms • Flu like symptoms • Tender, hot, red area on one breast • Breast distention with milk Nursing Management • Empty the breast by increasing the frequency of nursing or pumping • Control infection- Antibiotics • Analgesics • Warm/ice compresses • Assess infants mouth for thrush Postpartum Infection Education • Continue antibiotics • Monitor temperature and notify provider if temp greater then 100.4 • Watch for signs and symptoms of a recurrence • Practice good hand washing • Teaching Guidelines 22.2 pg. 765 Postpartum Affective Disorders • Plummeting levels of estrogen and progesterone after delivery contribute to the mood disorders • Disorders based on their severity: Postpartum blues Postpartum depression Postpartum psychosis Postpartum Blues Transient periods of depression during the first 1 to 2 weeks postpartum • Tearfulness • Sad feeling • Confusion • Insomnia • Feel overwhelmed Nursing Care • • • • • Remind mom that the “Blues” are normal Encourage rest Utilize relaxation techniques Share her feelings with her partner If symptoms do not resolve and progress to depression medical treatment needs to be sought Postpartum Depression • Gradual onset and is evident within first 6 wks. • Cause combination of body, mind, and lifestyle • Symptoms- sleep disturbances, guilt, fatigue, feelings of hopelessness Box 22.2 pg. 771 • Screening tools Postpartum Depression Management same as that for major depression • Antidepressants • Antianxiety • Psychotherapy • Marriage counseling if that is part of the causes Postpartum Psychosis • Emergency psychiatric condition which could put the women at risk for suicide & infanticide • Detect within 3 wks. of giving birth • Symptoms: delusions, hallucinations, agitation, inability to sleep, bizarre irrational behavior Postpartum Psychosis Management • Usually hospitalized for several months • Psychotropic drugs • Individual psychotherapy • Support group therapy