Heart Anatomy
advertisement

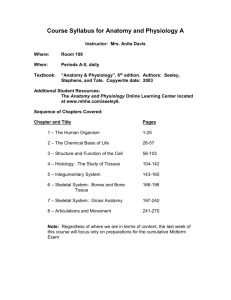
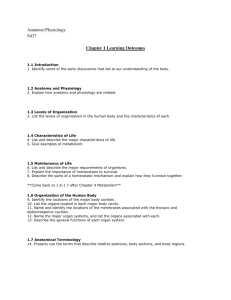
Anatomy & physiology of the heart Heart Anatomy Size, Location, and Orientation Enclosed in the mediastinum Base (posteriorsuperior portion) and Apex (inferioranterior portion) Heart Anatomy Coverings Pericardium protects the heart anchors the heart to surrounding structures such as the diaphragm and the great vessels prevents overfilling of the heart with blood Heart Anatomy Coverings pericardial cavity contains a film of serous fluid pericarditis: inflammation of the pericardium which may lead to adhesions between the layers or the buildup of fluid in the pericardial cavity (cardiac tamponade) Heart Anatomy Heart Wall Epicardium Myocardium bulk of the heart consisting mainly of cardiac muscle Heart Anatomy Heart Wall Endocardium simple squamous epithelium and a thin CT layer that lines the heart chambers and valves and is continuous with the endothelial lining of the blood vessels Heart Anatomy Chambers Atria Features small, thin-walled chambers Functions receiving chambers for blood returning to the heart from the circulation push the blood into the adjacent ventricles. Heart Anatomy Chambers Atria Receive blood from right side Superior and Inferior Vena Cava Coronary Sinus (draining the myocardium) left side Pulmonary Veins Heart Anatomy Chambers Ventricles Features make up most of the mass of the heart the walls of the left ventricle are 3X thicker than those of the right Heart Anatomy Chambers Ventricles Functions discharging chambers of the heart propel blood to Pulmonary Trunk (right ventricle), Aorta (left ventricle) Heart Anatomy Pathway of Blood Through the Heart Pulmonary Circuit functions strictly as gas exchange the right side of the heart is the pulmonary circuit pump this is a short, low-pressure circuit Heart Anatomy Pathway of Blood Through the Heart Systemic Circuit o functions as both gas and nutrient exchange o the left side of the heart is the systemic circuit pump o this is a long, high-resistance pathway through the entire body Heart Anatomy Heart Valves These enforce the one-way flow of blood through the heart The valves open and close in response to differences in blood pressure on their two sides Heart Anatomy Heart Valves Atrioventricular Valves the valves close when the ventricular pressure increases and forces blood against the valve flaps Tricuspid (right side) Bicuspid (Mitral) (left side) Heart Anatomy Heart Valves Semilunar Valves located between the ventricles and the large arteries these open when the pressure produced by the contracting ventricle exceeds that in the artery and close when the arterial pressure exceeds the pressure produced by the relaxing ventricle Pulmonary (right side) Aortic (left side) Coronary Circulation Coronary Arteries the coronary arteries arise from the base of the aorta and actively deliver blood only when the heart is relaxed the heart is 0.5% of body weight and receives 5% of the body's blood supply (most to the left ventricle) Coronary Circulation Coronary Arteries left main coronary artery left anterior descending artery: serves the interventricular septum and anterior walls of both ventricles circumflex artery: serves the left atrium and posterior wall of the left ventricle Coronary Circulation Coronary Arteries Right main coronary artery posterior descending artery: serves the posterior walls of both ventricles marginal artery: lateral wall of the right side of the heart Cardiac Veins follow arteries and join at the Coronary Sinus which empties blood into the right atrium Heart Physiology Electrical Events Intrinsic Conduction System of the Heart the ability of cardiac muscle to depolarize and contract is intrinsic (no nervous stimulation is required) nerve impulses can alter the basic rhythm of heart activity set by intrinsic factors Heart Physiology Electrical Events Action Potential Generated by Autorhythmic Cells Sequence of Excitation o Sinoatrial Node o Atrioventricular Node o Atrioventricular Bundle (bundle of His) o Bundle Branches o Purkinje Fibers Heart Physiology Electrical Events Extrinsic Innervation of the Heart fibers of autonomic nervous system accelerate or inhibit the basic rate of heartbeat set by the intrinsic conduction system Heart Physiology Electrical Events Electrocardiography electrical currents generated and transmitted through the heart spread throughout the body and can be monitored the graphic recording of electrical changes during heart activity is called an electrocardiogram (ECG or EKG) Heart Physiology Electrical Events Electrocardiography the ECG consists of series of three waves o P Wave: atrial depolarization starting at the SA node o QRS Complex: ventricular depolarization Heart Physiology Electrical Events Electrocardiography o P-R (P-Q) interval: time from the beginning of atrial excitation to the beginning of ventricular excitation and includes the contraction of the atria and the passage of the depolarization wave through the rest of the conduction system Heart Physiology Electrical Events Electrocardiography o T Wave: ventricular repolarization o Q-T interval: time from the beginning of the ventricular depolarization through their repolarization and includes the contraction of the ventricles Heart Physiology Mechanical Events: The Cardiac Cycle Terms Systole: contraction period of heart activity Diastole: relaxation period of heart activity Heart Physiology Mechanical Events: The Cardiac Cycle Cardiac Cycle o pressure in the heart is low and the blood is returning passively (70% of ventricle filling occurs) o atria depolarize (P wave) and contract and force the remaining 30% of the blood into the ventricles o the atria relax and remain in diastole through the rest of the cycle Heart Physiology Mechanical Events: The Cardiac Cycle o the ventricles depolarize (QRS complex) o ventricles begin their contraction o ventricular pressure rises rapidly and the AV valves close o as ventricular pressure rises above arterial pressure the semilunar valves open and the ventricles empty during the ventricular ejection phase Heart Physiology Mechanical Events: The Cardiac Cycle o ventricular systole ends with the repolarization of the ventricles (T wave) o ventricles relax and ventricular pressure drops o semilunar valves close o the atria have been filling with blood since ventricular systole and when the atrial pressure exceeds the ventricular pressure the AV valves open ventricular filling begins again Heart Physiology Cardiac Output General cardiac output is the amount of blood pumped out by each ventricle in 1 minute and is the product of heart rate (HR) and stroke volume (SV) stroke volume is the volume of blood pumped out by one ventricle with each beat and is the difference between end diastolic volume (EDV) and the end systolic volume (ESV) Heart Physiology Cardiac Output Regulation of Stroke Volume Preload: Degree of Stretch affected by the EDV and operates intrinsically Frank Starling Law of the Heart: The greater the degree of stretch of cardiac muscle fibers the greater the force of contraction and the greater the stoke volume Heart Physiology Cardiac Output resting cardiac fibers are normally shorter than the optimal length and stretching them (increasing EDV) produces dramatic increases in contractile force anything that increases the volume or speed of venous return (slow heart rate or exercise) increases EDV which increases the force of contraction which increases stroke volume Heart Physiology Cardiac Output Contractility affects the ESV and are extrinsic factors that increase the contractile strength of heart muscle many chemicals enhance contractility (positive inotropic agents) Heart Physiology Cardiac Output Afterload: Back Pressure affects the ESV the pressure exerted on the aortic (80 mm Hg) and pulmonary (20 mm Hg) valves by arterial blood important in people with hypertension where ESV is increased and stroke volume is reduced SA AV