Prostatitis
advertisement

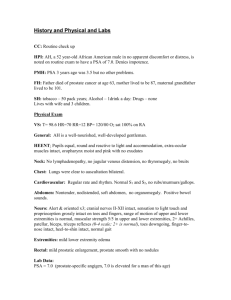
Dr Imran Cheema ST3 19/10/2010 Lower Urinary Tract Symptoms. History taking & use of IPSS. Differential diagnosis of LUTS. Examination and Investigation. Management of BPH. PSA request and counselling. Prostate cancer. Prostatitis and its Management. Obstructive Poor stream, Hesitancy, Terminal Dribbling, Incomplete Bladder Emptying, Overflow Incontinence Irritative Frequency, Nocturia, Urgency, Dysuria Describes difficulty starting and stopping when urinating with a poor stream. Compelled to void again soon after going. Getting up during night average 3x. PMH – Hypertension. What else would you like to know? Assess symptoms & severity. Assess impact on quality of life. Identify other causes of LUTS. Identify complications. Identify co-morbidities that may complicate treatment. 6/12 Hx gradual worsening symptoms. Worries when out & about – always looking for toilet. No dysuria or haematuria. No Hx of incontinence. Thinks is part of ageing! DH – Amlodipine 5mg. Objective measurement to grade symptoms. Useful to quantify severity, help to choose appropriate treatment & monitoring response. Mild = 0-7, Moderate = 8-19, Severe 20-35. Only 20% of GPs use this. Should we be using it more often? Causes of Outflow Obstruction: BPH, Urethral Stricture, Severe Phimosis, Idiopathic Bladder Outlet Obstruction, Bladder Neck or Sphincter Dyssynergia. Inflammatory Conditions: UTI, Bladder Stone, Prostatitis, Interstitial Cystitis. Neoplastic: Bladder or Prostate Cancer. Bladder Storage Disorders: Overactive Bladder Syndrome, Underactive Detrusor. Neurological Conditions: MS, Parkinson’s, CVA Conditions causing Polyuria: Diabetes, Congestive Cardiac Failure. What would you like to do? DRE – anal tone, size of prostate & abnormalities (hard, nodular, irregular, or fixed = carcinoma vs. smooth & regular) Focused neurological examination. Abdominal examination. Distended palpable bladder or other causes e.g. abdominal/pelvic mass PSA – more on this later! Urinalysis: Renal function tests: Exclude UTI, Haematuria, Glucose. All patients presenting with LUTS. If renal impairment needs Renal USS to check for hydronephrosis. Flow rate studies: Can be helpful to confirm diagnosis, objectively measure severity, monitor response to treatment. You diagnose mild BPH with no complications, what treatment option(s) will you discuss? Watchful Waiting: As not severely troubled by symptoms. Advise reducing fluid intake particularly caffeine & alcoholic drinks. Review medications e.g. diuretics Preventing constipation Advise to return if symptoms deteriorate Aims of treatment are: Relieve symptoms. Improve quality of life. Attempt to prevent progression of disease & development of complications. Symptoms worsened. Embarrassing episodes of urge incontinence. Worries about leaving the house. Wants to try medical therapy now. He has heard of using saw palmetto & wants to know if this is ok to try. What can we offer him? Alpha antagonists = 1st line. Work by relaxing smooth muscle in prostate & reduces urinary outflow resistance. Benefits: Act rapidly usually 48hrs, symptomatic relief immediately noticeable. 70% respond to treatment, expected in 3/52. Evidence: Many RCT & systematic review – similar efficacy between drugs & formulations. Choice dependant on tolerability & those with preexisting cardiovascular co-morbidity or comedication. Side effects: Cardiovascular – postural hypotension, dizziness, headaches. GU – failure of ejaculation. CNS – somnolence, dizziness. Compliance better with newer once daily sustained release e.g. Flomax MR, Xatral XL. No effect on prostate volume. Recommendations: Suitable for moderate-severe LUTS, low risk of disease progression. Tamsulosin has best cardiovascular side effect profile = 1st line. Alfuzosin. Reduces production of dihydrotestosterone & arrests prostatic hyperplasia. Two licensed for use in UK. Similar clinical efficacy & safety profile. Warn patients that shrinkage takes time – 6/12 & no noticeable symptom improvement for this period. Side effects: Finasteride (Proscar) Dutasteride (Avodart) ED, loss of libido, ejaculatory disorders, gynaecomastia, breast tenderness. Recent drug alert issue – link to male breast cancer. Recommendations: Suitable for moderate-severe LUTS & obviously enlarged prostate & those more likely to have progressive disease. NB – reduces PSA levels by half – need to adjust when interpreting results for suspected prostate cancer. Risk factors for disease progression Age >70yrs, IPSS >7, Prostate volume >30mls, PSA level >1.4ng/ml, QMax <12ml/s, Post void RV >100mls. For those patients with increased risk of disease progression & symptomatic. Increased side effects. Remember the saw palmetto: Is a plant extract. Others: Pumpkin seeds, stinging nettle root, cactus flower extracts, South African star grass, African plum tree. Currently NOT recommended (be aware of Oxford Handbook of GP). Advise patient: Although some evidence in studies shows benefits LUTS, it has not undergone same scrutiny for efficacy, purity or safety. Presents with painful inability to pass urine. Has tried several times to go without success since last night. No Hx of voiding difficulties. No back pain/sciatica. Has been constipated last few days. PMH – Osteoarthritis. He has a palpable bladder. DRE – large prostate, normal perineal sensation & anal tone. Acute urinary retention. This is urological emergency. Admit for catheterisation. Based on NICE guidelines. Urgent if: Soon: Acute or chronic urinary retention. Renal failure. Any suspicion of neurological dysfunction. Haematuria – see next presentation. Suspected malignant prostate. Recurrent UTI. Routine: Unclear diagnosis. No improvement on initial medical therapy. Presents with wife requesting PSA test. No symptoms. Concerns as advancing age. Has friends in USA of similar age that are screened for prostate cancer annually. Asking if similar NHS screening programme. PMH: Hypertension, low back pain. Back to basics – history & examination. Ask about LUTS, sexual dysfunction, ICE(!) Red flags: Weight loss, bone pain, haematuria. DRE: Hard, irregular prostate, loss of sulcus, palpable seminal vesicle. He is concerned about prostate cancer. Because there is a family Hx. Assessing risk: If one 1st degree relative <70yr: RR 2. Two 1st degree relatives (one of them) <65: RR 4. Three or more relatives: RR 7-10. Risk factors: Increasing age (85% diagnosed >65yrs). Ethnicity: highest rates in black ethnic group (lowest Chinese). Diet: Evidence that high in dairy products & red meat linked to increased risk. There is no prostate screening programme in the UK. Men can request a PSA test. www.cancerscreening.nhs.uk = good website with pt info leaflet. What is prostate cancer? Gland lies beneath bladder Each yr 22,000 men are diagnosed with prostate cancer Rare in men <50yrs Average age of diagnosis is 75yrs Slow growing cancers are more common than fast growing ones –no way of telling between two May not cause symptoms or shorten life What is the PSA test? Blood test. Many causes of raised levels. 2/3 of men with raised PSA do NOT have cancer. May lead to unnecessary anxiety and further investigations when no cancer is present. Can provide reassurance if normal. May miss diagnosis too (false reassurance). Does not distinguish between aggressive and nonaggressive tumours. May detect early stage of cancer when treatments could be beneficial. If raised, examine to check prostate or repeat test in few months. If referral to specialist: Prostate biopsy (TRUS). Complications: uncomfortable, bleeding & infection. 2 out of 3 men who have prostate biopsy will not have prostate cancer. However, biopsies can miss some cancers. Treatment options: Depends on classification (localised to prostate, locally advanced, metastatic). No strong evidence to suggest treatment of localised cancer reduces mortality. Main treatments have significant side effects & no certainty that treatments will be successful. Before PSA men should not have: Active UTI (wait 1/12). DRE (in previous week). Recent ejaculation (previous 48hrs). Vigorous exercise (previous 48hrs). Prostate biopsy (previous 6/12). A good screening test should fulfil WilsonJungner Criteria (1968, WHO). The only criterion met = prostate cancer is important health problem. No good understanding of natural history of condition, no acceptable level of sensitivity or specificity of test, no clear demonstrable benefit of early treatment. No means to detect which ‘early’ cancers become more widespread. More men would be found with prostate cancer than would die or have symptoms from it. Not clear if early treatment enhances life expectancy. No strong evidence that PSA testing reduces mortality from prostate cancer. PSA = 4.5 ng/ml. DRE – hard craggy prostate. What will you do? 2WW referral: DRE: hard irregular prostate typical of prostate cancer. Include PSA result with referral. DRE: normal prostate, but rising/raised age-specific PSA with or without LUTS. Symptoms & high PSA levels. Asymptomatic men with borderline age-specific PSA rpt test after 1-3 mo. If still rising refer. Age-related referral values for total PSA levels recommended by the Prostate Cancer Risk Management Programme. Age 50–59 60–69 70 and over PSA referral value (ng/ml). ≥ 3.0 ≥ 4.0 > 5.0 His Gleason score = 7 What does this mean? Moderate chance of cancer spreading Gleason score characterises prostate cancers on basis of histological findings. Used with T part of TNM staging to stratify risk of risk of progression. Watchful waiting: Low risk patients. Monitoring with annual PSA/rectal examination. Increase in PSA or size of nodule triggers active treatment. Active surveillance: Low or intermediate risk, localised prostate cancer. PSA surveillance & at least one re-biopsy. Treatment of choice if estimated life expectancy of <10yrs. Radical prostatectomy: Intermediate & high risk. Potential for cure, but up to 40% have evidence of incomplete tumour removal. Complications: impotence, incontinence. Radical radiotherapy radiotherapy: & external beam Aims to achieve cure, but persistent cancer found in 30% on biopsy. Short term side effects: bladder & bowel related (dysuria, urgency, frequency, diarrhoea). Long term side effects: impotence, incontinence, diarrhoea & bowel problems, occasional rectal bleeding. Brachytherapy. Hormone therapy: In conjunction with radiotherapy or following surgery. LHRH analogues e.g. Goserelin: given by subcutaneous injection every 4-12 wks. Side effects: Impotence, hot flushes, gynaecomastia, local bruising, infection around injection site. When starting LH initially increases causing ‘flare’ – counteracted by prescribing anti-androgens e.g. flutamide for few days prior to administering LHRH & for first 3/52. Anti-androgens can be used as monotherapy. Bony metastases: 1st line LHRH or bilateral orchidectomy. If hormone refractory. MDT: palliative care as needed. Chemotherapy. Corticosteroids. Spinal MRI. Bisphosphonates. All patients should be offered phosphodiesterase type inhibitors e.g. sildenafil for impotence. 5 yrly flexible sigmoidoscopy to look for bowel cancers following radiotherapy. Hot flushes can be helped with short blasts of progesterones (2wks). PSA should be checked annually in primary care once pt stable for at least 2yrs (discharged from hospital). Presents with Dysuria, Frequency & Urgency symptoms. Feverish. Low back pain. Supra-pubic pain. Perineal pain. Painful to open bowels. PMH: Type 2 Diabetes, Angina. UTI. Acute prostatitis. Urethritis. Cystitis. Pyelonephritis. Acute epididymo-orchitis. Local invasion from prostate, bladder or rectal cancer. Temp 37.8 Abdomen – soft, tender suprapubic, no loin tenderness. Urine dipstick +ve leucocytes & nitrites. DRE – Tender prostate. You diagnose acute prostatitis & discuss with urology for urgent referral. Start antibiotics immediately (whilst waiting MSU results): Ciprofloxacin 500mg BD. Ofloxacin 200mg BD. Treat for 28 days (prevent chronic prostatitis). If neither above tolerated, trimethoprim 200mg BD for 28 days. Quinolones or trimethoprim effective in most of likely pathogens & high concentrations in prostate. If unable to take oral Abx or severely ill – admit. Treat pain: Paracetamol +/- ibuprofen = 1st line. If severe offer codeine. If defecation painful offer stool recommended: lactulose or docusate. softener – Advise to seek medical advice if deteriorates. Reassess in 24-48hrs: Review culture results & ensure appropriate Abx. Refer to urology if not responding adequately to treatment, consider prostate abscess. Potentially serious bacterial infection prostate. Urinary pathogens = culprits commonly: Gram –ve organisms e.g. E.coli, proteus klebsiella, pseudomonas. Enterococci. of sp, Accompanied by UTI, occasionally epididymitis or urethritis. Not sexually transmitted. Can follow urethral instrumentation, trauma, bladder outflow obstruction, dissemination of infection from elsewhere. Admit: Urgent: If acute urinary retention, will need suprapubic catheterisation. Deteriorating symptoms despite appropriate Abx, need to exclude prostatic abscess (transrectal USS or CT). If pre-existing urological condition e.g. BPH, or indwelling catheter. Immuno-compromised or diabetic. Consider referral when recovered – investigation to exclude structural abnormality. 6/12 later he returns with continuing pain in perineum. Also complains of painful ejaculation affecting relationship. Still getting some LUTS – mainly frequency, urgency and poor stream. General aches in pelvis – fluctuates, deep, and sometimes in lower back. Tired, getting him down. Physical examination. Exclude other diagnosis. DRE: diffusely tender prostate. Urine culture. Consider PSA – more on this later. Prostatic massage primary care. not recommended in Characterised by at least 3/12 of pain in perineum or pelvic floor. Often with LUTS. And sexual dysfunction. ED, painful ejaculation, post-coital pelvic discomfort. Can be divided into 2 types. Dysuria, frequency, hesitancy & urgency. Chronic bacterial = 10% Chronic pelvic pain syndrome = 90% Management in primary care not dependent on classification. Assess severity of pain, urinary symptoms & impact on quality of life. Reassurance not cancer & not STI. Trend is for symptoms to improve over months-years. If defecation painful: offer stool softener. Consider trial of paracetamol +/- ibuprofen for 1/12. If Hx of UTI (or episode of acute prostatitis) in last 12 mo consider single course of antibiotic. Quinolones for 28 days, or trimethoprim where not tolerated. Refer cases to urology. Can start Abx whilst awaiting review. Urologist may consider trial of alpha blocker for 3/12. Consider chronic pain specialist referral. BMJ Learning modules: Benign Prostatic Hyperplasia, Prostate cancer risk management. Accessed via www.learning.bmj.com Clinical Knowledge Summaries on BPH, acute & chronic prostatitis. Accessed via www.cks.nhs.uk GP notebook. Accessed via www.gpnotebook.co.uk Oxford Handbook of General Practice 2nd Edition Department of Health. Prostate cancer risk management programme: PSA Testing in Asymptomatic Men. Accessed via www.cancerscreening.nhs.uk Prostate Cancer. InnovAiT, Vol 1, No. 9, pp. 642-650, 2008 GP Update Handbook (login access courtesy of Joanna Blyth) via www.gp-handbook.co.uk Patient UK – leaflets for patients www.patient.co.uk Management of prostatitis. BASHH 2008 guidelines. Accessed via www.bashh.org UK prostate link www.prostate-link.org.uk Prostate cancer charity www.prostate-cancer.org.uk Prostate cancer support association www.prostatecancersupport.co.uk