PTA 150 Day 9 10 CVA
advertisement

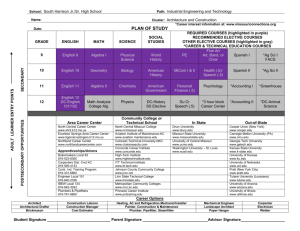
Concorde Career College Physical Therapist Assistant PTA 150: Fundamentals of Treatment II Day 9 & 10 CVA Concorde Career College Objectives Describe the pathophysiology of a CVA Describe physical and neurological impairments associated with CVA Describe physical therapy treatment interventions for patients after a CVA Concorde Career College Cerebrovascular Accident (CVA) Sudden loss of neurological function caused by an interruption of the blood flow to the brain O’Sullivan, pg. 705 Concorde Career College CVA Epidemiology The 3rd leading cause of death in the US THE most common cause for disability in US adults Incidence of stroke 1.25 times greater for males than females Compared to whites, African-Americans have 2x the risk of first-ever stroke (higher also with Mexican-Americans, American Indians, and Alaska Natives) Concorde Career College Definitions CVA is used interchangeably with the term “stroke” Neurological deficits must remain for > 24 hours to be classified as a stroke Transient Ischemic Attack (TIA) Temporary interruption of blood flow to brain Symptoms resolve quickly (within 24 hours) Few if any permanent signs or symptoms Precursor to stroke About 14% of persons surviving an initial stroke or TIA will experience another one within a year Concorde Career College Types of Strokes Hemorrhagic Stroke Blood vessels rupture, blood leaks into the brain 1˚ Cerebral Hemorrhage results from ruptured blood vessels weakened by atherosclerosis Results in ↑ ICP and restricts blood flow to the brain Subarachnoid Hemorrhage (SAH) – bleeding b/w arachnoid layer and pia mater • Common cause: aneurysm & AVM Subdural Hemorrhage (SDH) – bleeding b/w dura mater and arachnoid layer • Common cause is trauma Concorde Career College Types of Strokes Ischemic Stroke Most common (~80%) A clot blocks or impairs blood flow to the brain Can result from a Thrombosis • Results from platelet adhesions & aggregation on plaques • Cerebral Thrombosis: Blood clot forms in cerebral artery • Thrombi lead to ischemia = cerebral infarction Can result from an Embolus • Dislodged matter; blood clot, plaque, fat, gas, air, tissue that dislodges in the body and travels to the brain occluding cerebral circulation Concorde Career College Impact Severity and symptoms of stroke depend on Location of ischemic process Size of the ischemic area Nature & function of structures involved Availability of collateral flow • O’Sullivan , page 708 Concorde Career College Anterior Cerebral Artery Syndrome Middle Cerebral Artery Syndrome Posterior Cerebral Artery Syndrome Vertebrobasilar Artery Syndrome Internal Carotid Artery Syndrome Lacunar Syndrome Vascular Syndromes Concorde Career College Concorde Career College Anterior Cerebral Artery (ACA) Supplies medial part of the frontal and parietal lobe, basal ganglia and corpus callosum Concorde Career College ACA Syndrome Contralateral sensory & motor loss with LEs affected more than UEs Urinary incontinence Mental impairment (confusion, amnesia) Apraxia affecting ability to imitate or perform bimanual tasks Abulia (lack of desire to carry out an action), slowness, delayed movements, lack of spontaneous movements Behavioral changes Concorde Career College Medial Cerebral Artery (MCA) Supplies lateral cerebral hemispheres (incl. frontal, parietal and temporal lobes) Concorde Career College MCA Syndrome Contralateral hemiparesis of face and UE mainly Pure motor hemiplegia (lacunar stroke) Contralateral hemisensory loss of face & UE mainly Speech impairment: Broca’s aphasia, Wernicke’s aphasia, global aphasis Perceptual deficits: unilateral neglect, depth perception difficulties, agnosia Apraxia Ataxia of contralateral limbs (sensory ataxia) Contralateral hemianopsia Table 18.2 (O’Sullivan) Concorde Career College Posterior Cerebral Artery (PCA) Supplies occipital lobe, medial and inferior temporal lobe, thalamus & brain Concorde Career College PCA Syndrome Contralateral sensory & motor loss (hemianesthesia) Hemianopsia Visual agnosia, prosopagnosia and cortical blindness Oculomotor nerve palsy Involuntary movement Choreoathetosis, intention tremor, hemiballismus Thalamic pain Pusher syndrome Concorde Career College Hemiballismus - Video http://www.bing.com/videos/search?q=hemiballismus &view=detail&mid=290D280B1B53C5E9CDEB290 D280B1B53C5E9CDEB&first=0&FORM=LKVR Concorde Career College Vertebrobasilar Artery Vertebral artery arises from the subclavian artery, travels into the brain and then merge to form the basilar artery Vertebral artery supplies the cerebellum and medulla Basilar artery supplies the pons, internal ear, and cerebellum Concorde Career College Vertebrobasilar Artery Syndrome Wide variety of symptoms with ipsilateral and contralateral signs Numerous cerebellar and cranial nerve abnormalities Refer to Table 18.4 in O’Sullivan for details Concorde Career College Internal Carotid Artery (ACA) Syndrome Supplies both the MCA and ACA Complete occlusion leads to ↑↑ cerebral edema = coma & possible death Incomplete occlusion = mix of ACA & MCA syndromes Concorde Career College Lacunar Infarct Caused by small vessel disease deep in cerebral white matter Concorde Career College Lacunar Syndrome Contralateral weakness Sensory loss Dystonia/Involuntary movement Choreoathetosis, hemiballismus Ataxia Concorde Career College CVA – Major Risk Factors Primary Secondary Atherosclerosis Obesity HTN Hypercholesteremia Heart disease Physical Inactivity Diabetes ↑ Alcohol consumption Smoking TIA Concorde Career College Stroke Warning Signs TIME IS BRAIN Sudden numbness or weakness of the face, arm or leg, especially on one side of the body Sudden confusion, trouble speaking or understanding Sudden trouble seeing in one or both eyes Sudden trouble walking, dizziness, loss of balance or coordination Sudden, severe headache with no known cause www.StrokeAssociation.org Concorde Career College Imaging - CT Frontal lobe stroke Concorde Career College Imaging - MRI Concorde Career College CVA Medical Management Reestablish cerebral circulation and oxygenation Control blood pressure Maintain sufficient cardiac output Restore/maintain fluid & electrolyte balance Maintain blood glucose levels Control ICP Maintain bladder function (possible use of catheter) Maintain integrity of skin and joints Concorde Career College Pharmacological Management Anticoagulants (heparin, coumadin); to reduce clots and maintain profusion) Antiplatelets (aspirin); used to decrease the risk of recurrent stroke Antihypertensives Concorde Career College Surgical Intervention Endarterectomy – surgical removal of lining and plaque in an artery Used to prevent strokes (not treat them) In the case of hemorrhage – surgery to repair rupture, prevent further bleeding evacuate the clot Resection of unruptured AVM if found and risk is high Concorde Career College Primary Impairments Sensation Impairments ↓ sensory perception & ability to process sensory information • Touch, temperature, position, kinesthetic, pain • ASTEROGNOSIS • The inability to identify an object by touch without visual input Pain Can experience severe headaches, neck or facial pain Central post-stroke (thalamic) pain: constant, severe burning with intermittent sharp pains Concorde Career College Primary Impairments Visual Impairments Eye movements (sluggish, reflexive, ataxic) Hemianopsia: Blindness in half of each eye’s visual field (loss on the nasal side and half on temple side) Visual neglect Difficulties w/ depth perception & spatial relationships Forced gaze deviation Brainstem strokes may result in diplopia, oscillopsia or visual distortions Concorde Career College Primary Impairments Motor Impairments – Stages of Motor Recovery Stage 1 - Flaccidity Stage 2 - Minimal voluntary movement; may see synergies and spasticity develop Stage 3 – Voluntary control the movement synergies; spasticity may ↑ further (Continued) Concorde Career College Primary Impairments Motor Impairments – Stages of Motor Recovery Stage 4 – movement combinations that do not follow the path of synergy are mastered; spasticity ↓ Stage 5 – Difficult movement combinations are learned Stage 6 – disappearance of spasticity, individual joint movements become possible and coordination approaches normal Concorde Career College Primary Impairments Motor Impairments Weakness (paresis) • Occurs in 80-90% of all patients after stroke • Varies depending on location and size of stroke • Can result in complete paralysis/hemiparesis • Typically, more distal muscles exhibit greater weakness • May even see weakness on the “normal” side • Changes in muscle composition 2˚ weakness & disuse • Atrophy, ↓ Fast twitch type II, ↑ slow twitch type I • ↑ effort and fatigability Concorde Career College Primary Impairments Motor Impairments Changes in tone • Flaccidity – present immediately as a result of cerebral shock; usually short-lived but sometimes persists • Spasticity/hypertonicity • Occurs in about 90% of patients after stroke • Posturing of limbs is common with mod → severe spasticity • Spasms (internal or external stimulation) Concorde Career College Posturing Concorde Career College Primary Impairments Motor Impairments Abnormal synergistic movement patterns • Associated with spasticity, may ↓ with recovery • Review Table 18.5 in O’Sullivan Impaired reflex responses (mild to severe) • Vary according to stage of recovery • Hyporeflexia with flaccidity → hyperreflexia with spasticity • ↑ stretch reflex – clonus, clasp-knife, (+) Babinski • ATNR • Associated reactions Concorde Career College Primary Impairments Motor Impairments Impaired coordination responses • Cerebellar strokes = ataxia & weakness • Basal Ganglia involvement = slow movements (bradykinesia) & involuntary movements (choreoathetosis, hemiballismus) Concorde Career College Video - Cerebellar Ataxia http://www.bing.com/videos/search?q=cerebellar+a taxia&view=detail&mid=F8130C8EBA0E3DD338C 5F8130C8EBA0E3DD338C5&first=1&FORM=LKV R3 http://www.bing.com/videos/search?q=cerebellar+a taxia&view=detail&mid=08E8A16F23E5E860EE90 08E8A16F23E5E860EE90&first=21&FORM=LKVR 18 Concorde Career College Primary Impairments Motor Impairments Altered motor programming • Motor praxis • Ideational apraxia • Ideomotor apraxia Diminished muscle performance for ADL • Strength, Power, Endurance Concorde Career College Primary Impairments Postural Control & Balance Impairments May experience difficulty with balance 2˚ to an external force or during self-initiated exercises • Corrective responses to perturbations are often inadequate = fall Asymmetry typically noted in posture • Typically see falls to the same side as weakness Pusher Syndrome • Active pushing of the uninvolved side offsets muscle control of the involved side (falls, leaning) Concorde Career College Primary Impairments Speech and Language Impairments Aphasia – an acquired communication disorder caused by brain damage and is characterized by an impairment of language comprehension, formulation and use. (O’Sullivan, pg. 722) Concorde Career College Primary Impairments Speech and Language Impairments Receptive Aphasia • aka. Wernicke’s/Sensory/Fluent Aphasia • Auditory and reading comprehension impaired • Speech is functional Expressive Aphasia • aka. Broca’s/Nonfluent Aphasia • Difficulty finding words to express ideas Global Aphasia • Receptive and Expressive Concorde Career College Primary Impairments Speech and Language Impairments Dysarthria • Nasal quality of speech, slurred words Dysphonia • Difficulty producing sounds Dysphagia • Difficulty in swallowing Concorde Career College Primary Impairments Altered Perception Body scheme – relationship of body parts to one another as well as the body’s relationship to the environment Body image – visual and mental image of one’s body may be altered following a stroke • Includes the individual’s feelings about this image Concorde Career College Primary Impairments Examples of body scheme/image impairments: Unilateral Neglect • Visual recognition or attention on involved side • Limb neglect or attention on involved side Anosognosia – denial, neglect or unawareness of one’s paralysis Somatoagnosia – lack of awareness of one’s body structure and its relationship to the environment Right-left discrimination Finger agnosia Concorde Career College Primary Impairments Altered Perception Agnosia - inability to recognize incoming information despite intact sensory capabilities (O’Sullivan, pg 723) • Visual object agnosia • Auditory agnosia • Tactile agnosia (astereoagnosia) Spatial relationship – difficulty determining the relationship between the body and 2 or more objects in the environment Concorde Career College Primary Impairments Cognitive Impairments ↓ alertness ↓ attention Altered orientation Diminished memory Impaired executive function Concorde Career College Primary Impairments Cognitive Impairments – Vocabulary Confabulation Perseveration Multi-infarct dementia Delirium Concorde Career College Primary Impairments Alterations in Affect Pseudobulbar Affect • A.k.a. emotional dysregulation syndrome or emotional lability • Emotional outbursts (crying, laughing) Apathy Euphoria ↑ irritability or frustration Social inappropriateness Depression Concorde Career College Primary Impairments Bladder and Bowel Function Common during acute phase Often implement a toileting schedule Urinary retention controlled with catheterization Can often lead to embarrassment, isolation or depression Concorde Career College Primary Impairments Hemispheric Behavioral Differences Left Hemispheric Damage • Difficulties in communication • Difficulty with processing information • Cautious, anxious, disorganized • Often very aware of impairments Right Hemispheric Damage • Difficulty in spatial-perceptual tasks • Difficulty with grasping overall idea of task or activity • Quick, impulsive • Overestimate their abilities, poor judgment Concorde Career College General Characteristics of CVA Right Hemisphere CVA Left side weakness or paralysis Hemianopsia Decreased awareness and judgment Memory deficits Inattention and less reasoning Emotional labile Impulsive behaviors Concorde Career College Characteristics of CVA Left Hemisphere CVA Right side weakness Aphasia Motor Apraxia Dysphagia Hemianopsia Concorde Career College Complications & 2˚ Impairments Musculoskeletal Loss of ROM & Contractures Edema & pain Disuse atrophy & weakness Osteoporosis • Fall risk Concorde Career College Complications & 2˚ Impairments Neurological Seizures Hydrocephalus – an excessive accumulation of CSF within the cranial cavity Cardiovascular Thrombophlebitis/DVT Impaired Cardiac Function • Impaired cardiac output, decompensation, rhythm disorders • Can restrict exercise/activity tolerance Concorde Career College Complications & 2˚ Impairments Pulmonary Decreased lung volume Decreased pulmonary perfusion & vital capacity Altered chest wall excursion Greater energy expenditure Aspiration Integumentary Skin breakdown and decubitis ulcer • Pressure, friction, shearing Concorde Career College Rehabilitation after Stroke The Role of the PT & PTA Concorde Career College Acute Phase Lo-intensity therapy can begin once stabilized medically. Early mobilization Minimize deconditioning Functional reorganization is promoted Learned nonuse is minimized Reinforce a positive outlook Decreased incidence of depression, apathy and mental deterioration Early presentation of rehabilitation plan Monitor for potential medical emergencies! Average hospital stay is about 7 days Concorde Career College Post-Acute Phase Triage Inpatient rehabilitation, TCU, SNF What other services may be involved with the patient at this time? Progression to home care, outpatient PT Assisting with return to work, recreation, social activities Concorde Career College PT Examination Patient history Joint Integrity & Levels of Mobility Voluntary Movement patterns Strength Postural control & balance Ambulation & Functional mobility Functional status Consciousness Communication Cognitive, emotional and behavioral states Cranial Nerve Integrity Sensory Integrity Perception Tone/Reflexes Concorde Career College Gait after a Stroke The PTA Assessment Concorde Career College VIDEO http://www.youtube.com/watch?v=YMzVywpbNes& feature=related Concorde Career College Gait after Stroke Important to look at movements occurring at the ankle, foot, knee, hip, pelvis, trunk and UEs. Observe the different planes of motion Quantitative measures include distance, time, cadence, velocity, and stride times What type of AD may be necessary? May consider videotaping Concorde Career College Trunk/Pelvis Stance Phase Forward trunk 2˚ • Weak hip extension • Flexion contracture Swing Phase ↓ forward pelvic rotation 2˚ • Weak abdominal mm Leaning towards the stronger side to clear the weaker side foot from the floor OR Backward leaning of trunk • Both may be due to weak hip flexors Concorde Career College Hip Substitutions as a result of inadequate hip flexion: Hip hiking • Weak abdominal mm and inadequate knee flexion may also contribute to this Circumduction • ↑ extensor tone, ↑ PF tone or foot drop as well as inadequate knee flexion may also contribute to this External rotation/adduction May see the opposite, exaggerated hip flexion • Flexor synergy Concorde Career College Knee Stance Phase Excessive knee flexion 2˚ • • • • Flaccid or weak LE, especially hip & knee extensors Poor PPC Flexion contracture Ankle DF range past neutral Hyperextension of knee 2˚ • ↑ extensor tone of LE • Quadricep spasticity • Weakness of gluteus maximus, hamstrings and quads • PF contracture past 90˚ • Impaired PPC Concorde Career College Knee Swing Phase ↓ Knee flexion 2 ˚ • ↑ LE extensor tone, spastic quadriceps • Inadequate hip flexion and poor foot clearance • Circumduction or hiking pattern often seen as a result Exaggerated, delayed knee flexion 2˚ • Strong flexor synergy Inadequate knee extension at initial stance 2˚ • Spastic hamstrings • Sustained total flexor pattern • Weak knee extensors Ankle/Foot Stance Phase Equinus gait – heel does not touch down • Spastic or contracture of gastrocnemius Varus foot – weight is on the lateral side of the foot • Spastic tibialis anterior, posterior tibialis, toe flexors, soleus Unequal step length • Hammer toes can cause pain with WB and prevent a full step forward with opposite leg • Increased flexor tone in toe muscles • Lack of DF ROM on affected side Concorde Career College Ankle/Foot Swing Phase Persistent equinus or varus or a combination of the 2 (equinovarus) • Weak dorsiflexors may contribute to this in addition to spastic muscles Exaggerated DF 2˚ strong flexor synergy pattern Concorde Career College Intervention Concorde Career College Strategies to Improve Sensory Function Encourage use of the affected side!! Training should focus on functional tasks Examples: Stroking skin with various fabrics Drawing shapes, letters onto the skin of affected side Approximation Inflatable pressure splints Patient and family/caregivers must be educated on impairments as well as safety measures to protect the involved limbs Concorde Career College Strategies to Improve Sensory Function With unilateral neglect, incorporate strategies that encourage awareness and use of the body on the involved side Visual scanning Cueing (visual, verbal or motor cues) Imagery Visual focus on the affected arm or leg during activity Bilateral tasks Tactile input given by the therapist to the involved limb Patient may require reorientation Concorde Career College Strategies to Improve Flexibility and Joint Integrity Early ROM daily UE PROM of shoulder important for reaching and overhead movements • Careful attention to mobilize the scapula on the thoracic wall, maintain upward rotation and protraction Maintain full elbow extension, wrist and finger ROM Self UE ROM may include arm cradling, table-top polishing, supine AAROM with intact UE clasping the affected UE Concorde Career College Strategies to Improve Flexibility and Joint Integrity Effective UE positioning is important Lap tray or arm trough 5˚ shoulder ABD & FLEX, neutral rotation, 90˚elbow FLEX & slightly forward, forearm pronated, functional hand position Concorde Career College Strategies to Improve Flexibility and Joint Integrity Volar resting (pan) splint Functional 20-30˚ wrist extension 40-45˚ MP flexion 10-20˚ IP flexion Thumb opposition Concorde Career College Strategies to Improve Flexibility & Joint Integrity LE ROM Often see limited ankle DF • Incorporate weight bearing encouraging DF by performing forward weight shifts or using adaptive equipment (tilt board, foot rocker) Pay careful attention to hip flexor and knee flexion contraction with prolonged sitting in wheelchair ROM in opposition to spasticity (if present) should also be performed daily Concorde Career College Strategies to Improve Strength <3/5 Strength Therapist assisted exercise Powder board Sling suspension Aquatic Exercise 3/5 Strength Gravity resisted exercises >3/5 Strength Free weights Bands Machines Concorde Career College Strategies to Improve Strength Important to combine strengthening and function Wearing ankle weights while performing step ups or stair climbing Reaching exercises while wearing wrist weights • Secondary postural stabilization occurs with this type of exercise Resisted walking with Theraband taut at waist level Sit to stand with resistance given at shoulders by therapist Concorde Career College Strategies to Improve Strength Safe Exercise Prescription Exercise is contraindicated with HTN & recent stroke With HTN – avoid high-intensity & isometric exercises • Concentric & eccentric exercises are less stressful for the cardiovascular system • Sitting exercises less risk for increasing blood pressure as compared to supine exercises Proper warm-up & cool down are important, better to begin with LE exercises first Concorde Career College Strategies to Improve Strength Need to carefully monitor: BP HR Rate of Perceived Exertion (RPE) Breathing (avoid breath holding & Valsalva) Patient needs to be educated to monitor HR and RPE as well as warning signs to stop exercises Concorde Career College Strategies to Manage Spasticity Early mobilization Prolonged stretching Examples: Rhythmic rotation Slow rocking movements over limb in an elongated, weight bearing position PNF upper trunk patterns can ↓ trunk tone Activation of the antagonist muscles using slow & controlled movements May need to use facilitation techniques Concorde Career College Strategies to Manage Spasticity Modalities to reduce spasticity Cold (ice wraps, ice packs) Estim to the antagonist Vibration May incorporate air splints Can use soothing verbal commands/relaxation techniques or imagery Concorde Career College Strategies to Improve Initial Movement Initially focus on normal postural alignment as well as control and functional use of extremities Strategies should address dissociation and selective (out-of-synergy) movement patterns Reinforce slow, controlled, “normal” movements May progress postures to optimize movements Example: shoulder flexion in supine, sitting and then standing Assistance may initially be provided but then progress to active, independent movements Concorde Career College Strategies to Improve Initial Movement Control When addressing function, consider practicing eccentric contractions before concentric Eccentric contraction are more efficient Can gradually progress to a variety of activities that use all 3 types of contractions Concorde Career College Strategies to Improve Motor Learning Strategy Development Critical tasks, goals and outcomes are identified Begin practice, may practice components of the task before practice of the whole task Important to move towards whole task to allow for transfer of learning Practicing with less affected side first may also assist with transfer effects Clear, simple verbal instruction should be given Patient needs to be active in problem solving • i.e., Can the patient identify components performed incorrectly Concorde Career College Strategies to Improve Motor Learning Feedback Can be extrinsic or intrinsic During early motor learning, more likely to use extrinsic feedback • Mirrors, verbal cues or manual cueing from therapist Patient’s attention should be geared towards recognizing intrinsic and developed more as therapy progresses • Patient should “feel the movement” Important to avoid bombardment of feedback and limit immediate feedback Concorde Career College Strategies to Improve Motor Learning Practice, Practice and more Practice May initially be limited by endurance Need to encourage variable practice in order to progress Ensure the environment is conducive to learning • Eventually can progress to a more open, real-life environment Motivation is important • Patient should be involved in goal setting • Treatment session should be positive • Therapist needs to be a support system, encouraging Concorde Career College Strategies to Improve Postural Control & Functional Mobility Rolling Practice rolling to both sides Rolling to affected side more difficult Clasp hands together to assist with momentum and use of the affected UE Can bend the LE’s to assist with pushing over Sidelying on affected side promotes WB of the affected UE Concorde Career College Strategies to Improve Postural Control & Functional Mobility Sit to Supine/Supine to Sit Important to practice towards both sides Will likely be easier to perform from non-involved side Therapist may initially facilitate/assist movements Concorde Career College Strategies to Improve Postural Control & Functional Mobility Sitting Initially looking for symmetrical posture with proper spinal alignment Early sitting may involve therapist cueing (tactile &/or verbal) May use UE’s initially to maintain sitting posture Progress to no UE support, weight shifting, truncal motions, PNF patterns, reaching/dynamic activities, perturbations, scooting Progression may then include these same activities while sitting on a ball Concorde Career College Strategies to Improve Postural Control & Functional Mobility Bridging Develops hip and trunk extensor control as well as LE selective control & early LE WB Can progress from performing the exercise, holding the position and then performing dynamic activities within the posture Concorde Career College Strategies to Improve Postural Control & Functional Mobility Sit to Stand (STS) Focus on symmetrical WB, coordination & timing (Demonstration of proper sit to stand) Strategies to initiate STS: • Clasp hands or reaching forward with UE’s • Place pt hands on ball while therapist stabilizes ball but then move ball forward to promote anterior weight shift • Raise the mat height • Place stronger foot slightly behind the weaker Concorde Career College Strategies to Improve Postural Control & Functional Mobility Sit Down Transfers Strategies to promote controlled sit down include: • Partial wall squats • Varying mat height • Lateral pelvic shifts to involved side and alternate sit/stand Concorde Career College Strategies to Improve Postural Control & Functional Mobility Standing, Modified Plantigrade Standing with affected UE extended and in weightbearing position, LE also extended Assists with development of postural and extremity control Very stable position Can progress from static standing to movement and reaching activities Concorde Career College Strategies to Improve Postural Control & Functional Mobility Standing Initially standing can occur in parallel bars or at bedside with assist Progression can include: • 2 hand support → 1 hand support → free standing • Static standing → weight shift → dynamic (reaching, stepping) → perturbations/rhythmic stabilization Focus on proper alignment and symmetry Concorde Career College Strategies to Improve Postural Control & Functional Mobility Transfers Need to practice transfers to both sides Important to support the weaker knee Vary surfaces and surface heights May progress from squat-pivot to stand-pivot Concorde Career College Strategies to Improve Postural Control & Functional Mobility Pusher Syndrome Focus is on the vertical Can use mirrors, the wall, a ball, or even the therapist to assist with active, appropriate shifting rather than pushing Ask the patient, “Which way are you leaning?”; “Which direction should you move to be vertical?” Concorde Career College Strategies to Improve UE Function UE as a Postural Support Extended UE weightbearing promotes proximal stabilization and counteracts flexion synergy, hypertonus Approximation can stimulate shoulder girdle stabilization and elbow extensors Can perform in sitting, modified plantigrade, standing and quadruped Progress from holding the position to more dynamic activities Concorde Career College Strategies to Improve UE Function Reaching Can begin with positions which eliminate gravity • Sidelying, tabletop assist, “dusting” with washcloth, reaching down to touch the floor • May also need therapist assist Progress to anti-gravity activites Combine with balance & functional activities Vary height/distance to reach, weight of object grasped, time to complete the task Avoid substitution Concorde Career College Strategies to Improve UE Function Manipulation & Dexterity Initial tasks usually involve more gross grasp and release Can begin by using affected hand to stabilize while performing a task with stronger hand Progress to bilateral activities, emphasize function/ADLs Include reaching activities Build-ups for items such as forks, toothbrush, pens can improve independence and efficiency Concorde Career College Strategies to Improve UE Function Enhanced Training Activities Bilateral arm training w/ rhythmic auditory cueing (BATRAC) http://www.youtube.com/watch?v=dy2qzvDa-Fc Concorde Career College Strategies to Improve UE Function Enhanced Training Activities Constrain-Induced Movement Therapy (CIMT) Electromyographic Feeback (EMG-BFB) Neuromuscular Electrical Stimulation (NMES) Concorde Career College Strategies to Improve UE Function Management of Shoulder Pain Common complication post stroke In the case of flaccidity, arm needs support at all times Proper arm support is essential Scapula/shoulder protracted, arm forward in slight ABD and neutral ROT ↓ subluxation – NMES, supportive devices ↓ Pain, normalize tone – gentle stretching & mobilization, cryotherapy, EMG BFB, relaxation training Adhesive capsulitis treated with mobilization, PROM and ultrasound Avoid trauma or traction injuries with functional mobility Concorde Career College Strategies to Improve UE Function Supportive Devices Slings Pros and Cons Concorde Career College Strategies to Improve UE Function Supportive Devices (Gillen) Consider using slings only with initial transfer and gait training Determine whether a sling that places the arm in flexion is really necessary, if so consider wearing only for short periods of time Selection of a sling is on an individual basis Consider alternatives: NMES, taping, hand in pocket/belt, lap tray Concorde Career College Strategies to Improve LE Function Necessary to prepare for appropriate gait Helpful to start with improving pelvic control Can practice forward pelvic rotation in sidelying, supine, hooklying, kneeling, sitting on ball, standing Break synergistic patterns Example: hip extension is paired with knee flexion to allow toe-off during terminal stance/pre-swing Activities to promote this include: bridging, supine hip extension with knee flexed and heel pressing into the floor or standing and repeatedly practicing this phase of walking Concorde Career College Strategies to Improve LE Function Avoiding hyperextension of the knee Activities to promote this control include: controlled heel slides in supine and sitting, partial wall squats, controlled flexion and extension of knee on leg press, terminal knee extension exercises with Theraband in standing Concorde Career College Strategies to Improve LE Function Important to progress activities by modifying postures Example: Supine → Sitting → Kneeling → Standing And… emphasize reduction of synergistic patterns Concorde Career College Strategies to Improve Balance Important to select appropriate exercises, challenging to the patient but does not compromise safety Must first achieve postural alignment and static stability in upright postures Can then progress to exploring limits of stability Weight shifting Encouraging symmetrical weight bearing Encouraging weight bearing to more affected side Concorde Career College Strategies to Improve Balance Examples: Vary the BOS Vary the support surface Vary sensory inputs Vary UE position/support Vary UE movement Vary LE movement Vary trunk movements Incorporate dynamic functional activities Incorporate dual tasks Change the environment Concorde Career College Strategies to Improve Balance Strategies Ankle • Small A/P weight shifting or small perturbations • Standing on rocker board, foam roller, dynadisc Hip • Larger A/P weight shifts or perturbations • Tandem stance promote medial-lateral strategies • Standing on floor or foam roller Stepping • Displacement of COM in all directions • Therapist can apply a band around waist • Step ups Concorde Career College Strategies to Improve Balance Need full attention from patient (and therapist!) Provide well-timed feedback Minimize hand support Encourage active problem-solving Safety education must be included Concorde Career College Strategies to Improve Locomotion Gait training Initially parallel bars & assistive devices can be used • Pros & Cons Important to progress patient to least restrictive device or no device as able Want to encourage even, longer step length and increased time • May use rhythmic auditory cues OR • Markers on the floor with tape Concorde Career College Strategies to Improve Locomotion Look at each phase of gait Stance Phase • Initial weight acceptance • Midstance control • Forward weight advancement Swing Phase • Knee and foot control for toe clearance • Foot placement UE posturing Concorde Career College Strategies to Improve Locomotion Vary the environment Community walking, hiking trails, hills Practice walking in all directions Forward, backward, sideways Practice cross-stepping Include stairs, curbs, step-over-step Include timing activities Crossing the street, using escalators, elevators and automatic doors Concorde Career College Strategies to Improve Locomotion Practice dual-task activities Talking, bouncing a ball, carrying a tray Incorporate balance activities Tandem walking, walking on foam/gravel/grass Treadmills, cycle ergometers These tools may assist with improving time and reciprocity of the LEs Concorde Career College Strategies to Improve Locomotion Body weight support systems Limb load monitors NMES to improve ankle DF Concorde Career College Strategies to Improve Locomotion Orthotics AFO Knee Controls Concorde Career College Strategies to Improve Locomotion Wheelchairs Appropriate position Types: • Hemi-height wheelchair (Seat to floor height is 17.5”) • One arm drive chair • Power wheelchair Training activities • Proper use, maintenance and safety • Methods of propulsion • Level and varied surfaces • Transfers Concorde Career College Strategies to Improve Aerobic Function Initial Phase: functional activities are sufficient Post-Acute Phase: may progress to treadmill, stationary bicycle Carefully monitor VS & symptoms of exertional intolerance, impending stroke or heart attack Choose method based on patient’s interest Suggested frequency is 3X/week for 20-60 minutes May be daily at lower intensities Recommend starting with intermittent training and progressing to continuous 30 minutes of exercise Concorde Career College Questions Concorde Career College