Aintree University Hospital NHS Foundation Trust
advertisement

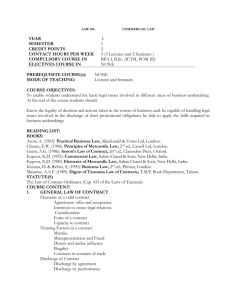
Discharge To Assess Aintree University Hospital 10th September 2015 Angela McAvoy: Therapies CBM Rebecca Mitchell: Senior Physiotherapist Claire Denton: Liverpool Senior Social Worker Biography Angela McAvoy Therapies Clinical Business Manager for Aintree University Hospital. Picture to go here Qualified as an Occupational Therapist form St Loye’s School of Occupational Therapy in 1989. Has worked in a variety of clinical settings including Acute and Community Services, Prosthetic and Wheelchairs Service and AED before moving into her current role leading the Integrated Therapy Service at Aintree which includes Occupational Therapy, Physiotherapy, Dietetics, Speech and Language Therapy, Prosthetic and Wheelchairs, Patient Appliances and North West Assistive Technology Biography Rebecca Mitchell BSc Hons Physiotherapy Manchester Metropolitan University 2009 Physiotherapist for Aintree University Hospital since 2013 Senior Physiotherapist within Aintree@Home team at Aintree University Hospital Specialist interest in falls prevention, frailty and discharge to assess Qualified acupuncturist and pilates teacher Biography Claire Denton Employed by Liverpool City Council in the role of Social Work Team Leader for Aintree University Hospital. Qualified as a Social Worker in 1999, working in an integrated Older People’s team and GP surgery. Following this was seconded to a PCT to support with the implementation of the Older People’s National Service Framework. Claire then joined an integrated disability team as senior practitioner, supporting service users with a learning disability, ASD and those with an acquired brain injury. Claire is also a qualified Social Work practice educator. Discharge to Assess model Aintree’s Trust Vision “To provide world class services for all our patients” Aintree at Home encapsulates the “Discharge to Assess” model and facilitates early and safe discharge through the functional and social care assessment in the service user’s home. By identifying and providing the appropriate social care, in partnership with social care providers, Aintree at Home reduces length of stay, maximises independence and helps prevent unnecessary readmission. “The objective of discharge is not simply to get the person out of hospital, but also to provide seamless support, to ensure a return to their home or care home in the best possible physical, mental and emotional state.” Commission on Dignity in Care for Older People, June 2012. Overview of the service • Aintree at home began as a pilot in December 2012 - discharge to assess approach for therapy. • Feb 2015 stakeholders meeting - social work assessments at home since • A service that adopts a strong multi-disciplinary approach of Occupational Therapists, Physiotherapists, Nurses and Generic Therapy Assistants. • Close working relationships with hospital based social workers and community therapy and social care services, GP’s and district nurses. • Seven days per week 8am-6pm, working with community outreach teams to support bedtime care calls. • Outreach model with a strong ethos of “getting it right for every patient every time” by moving traditional therapy and social work assessments out of the hospital environment and into the home environment. Drivers for Discharge to assess • • Improving Patient Care- ageing population, with increasingly complex health and social care needs Need to develop patient centred care – assessment in the right place at the right time, patient family and carer involvement Positive patient experience • • • • Improving patient flow- Pressures in acute and timely discharge of patients Availability and use of community resources Financial challenges facing NHS/Social Sector Move of resources away from secondary care into primary care • Process • • • • • • • • Stakeholder event organised by Liverpool commissioners Opportunity to do something different Agreement around the table – removed barriers immediately Started process next day Step by step approach – 1 patient at a time –learnt lessons as you go Open forum – invited all Weekly operational review meeting Communication and engagement – ward mangers, patient flow, consultants, board rounds • Visited key wards identified – staff supported by CBM, Clinical Lead • Test phase February to July 15 – next phase formalising project Factors to consider and address • • • • • • Cultural change Historic processes Change in staff/services –opportunities/impact Commissioners involvement Opportunities for engagement and sharing the work Learn from others • Providing equitable services for all – 3 CCG’s/Local Authorities Process for selecting inpatients • Potential for D2A highlighted by ward therapist. • D2A co-ordinator screens patient. • Outcome discussed with allocated social worker. • Co-ordinator contacts referrer and confirms plan/information details. • Paper work completed and section two completed to social worker. • Information given to patient re: D2A process. • Treatment plan agreed with patient. • Communication with the ward and patients family as required. Discharge process for D2A patients • TTO’s collected. • Escorted discharge home • Joint assessment completed at home or social worker to review at home within 48hours • Therapy complete full assessment and provide any equipment required. • Social worker assesses care needs and arranges POC through care agency. • A@H bridge POC until care agency care start, independently or in collaboration with other agency. • Evaluation form completed and statistics gathered. Outcome measures • Capacity Vs Demand- statistics kept and evaluated monthly for length of stay, prevention of re-admissions, changes in care packages, number of patients accepted, number of patients deferred and the reasons for this. • Patient satisfaction forms- completed for each patient and evaluated on a quarterly basis by the clinical audit department. • Blaylock assessments- standardised assessment. • Referrals generated post discharge/ sign posting -recorded to examine if there has been an increase or reduction in the need for community organisations. • Discharge problems identified/ resolved e.g. medication, equipment. Discharge To Assess challenges • Delay in TTO’s and difficulties with medication- nursing role developing supports to resolve issues, developed a local medication administration guideline, established good links with pharmacy and community GP’s. • Delay in transport- applied for funding for additional vehicles including wheelchair accessible vehicles to escort patients home in, currently have one available work car and two vans to deliver essential equipment. • Initial lack of understanding of the discharge to assess process- established working policies and ++ promotion to members of the MDT. • Lack of communication from the ward re: discharge- kept record of difficulties, provided regular feedback and training. • Lack of initial crisis support in community- lack of step up beds/ access to community resources e/g lifelines, key safes etc, capacity of emergency teams to support bed calls, D2A only available to one of our three CCG’s. Challenges in Social Care • Understanding roles of different professionals • Timely and appropriate assessments -risk assessment, not over whelming the patient • Establishing pathway for D2A alongside process for response to Assessment and Discharge Notifications from the trust (not causing further delay, requesting care in a timely manner) • Agreeing criteria for suitable patients (Clarity between A@H and D2A) • Issues of Mental Capacity, consent and Safeguarding issues (terminology, risk-particularly for patients lacking in capacity who may refuse to return to hospital) Results Discharge to Assess Feb-July 2015 NUMBER OF PATIENTS 40 NUMBER OF VISITS for D2A including bridging POC gaps 368 NUMBER OF BED DAYS SAVED 327 POC changes following one initial visit POC reduced = 13 patients POC increased= 1 patient 8 bed days saved on average per patient (total of 21 calls reduced) Summary: Our analysis clearly demonstrates that valuable bed days could be saved if patients were being assessed for packages of care earlier and in their own home. Previously, we developed a package of care based on assessments which took place in the hospital, only to find the reality in the patient’s home required different or additional elements, which would further delay the patient’s discharge. It reduces patient dependence on long term POC by incorporating a re-enabIement approach. Case study one • 58 year old female. PMH: COPD, depression. SH: lived alone in house • Joint SW/ PT Ax at home- on arrival home house had been burgled • Completed Ax and equipment to facilitate stay at daughters property • Gave information and support • Patient and daughter happy with support, no POC needs identified. “ You were excellent, 10 out of 10. Thank you so much for all your help” Case study two • 91 year old female. PMH: Registered blind, OA. SH: lived alone, no family support. • Joint SW/ OT ax at home • Previous POC- patient identified as having increased needs as an inpatient (4calls) • Equipment provided to increase safety • A@Home provided POC 2 calls/day • 7 visits completed, 7 bed days saved • LT POC- 2calls/day Patient feedback Are there any comments on areas we could improve? “None, It was very good care” “I was treated well…… with respect and staff were very attentive” “Excellent, 10 out of 10. Thank you so much for all your help” Plan for future • Increased D2A patients per week- continue to grow as the pilot expands. • Better access to step up beds. • Continue to improve networking with community teams/ collaborative working. • Increased awareness of D2A throughout trust. • Increased family/ patient education at front door/ ward re: assessment at homesome reluctant for discharge from hospital. • Increased SW support from our other two CCG’s. Service Evaluation Since the service was piloted in December 2012 there has been continuous evaluation to ensure we learn through good and bad experiences. We have shared our learning through training and awareness sessions, formal presentations, articles in trade publications and visits to other hospitals to share our model. Aintree at Home has also been presented to undergraduates at the University of Liverpool and at national conferences. Aintree has demonstrated with the growth of the Aintree at Home service that more patients can be supported home from the acute setting sooner with an early supported discharge approach. The model could be easily replicated within other Trusts, potentially easier than Aintree, who are challenged by managing discharge and on going support for our patients from 3 different boroughs, with 3 different social services, equipment providers and community services. We firmly believe that we have a high quality service that will continue to grow and adapt to meet the future needs of the NHS. Thank you Any questions? For further information please contact: Angela McAvoy Aintree University Hospitals Therapy Outpatient Department Lower Lane Liverpool L9 7AL ANGELA.MCAVOY@aintree.nhs.uk