Infectious Disease - Clinical Departments
advertisement

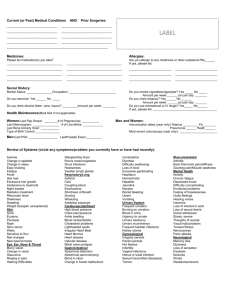
Infectious Disease A 65-year-old woman is evaluated for a 1-day history of fever, headache, and altered mental status. Medical history includes type 2 diabetes mellitus and hypertension treated with glipizide and hydrochlorothiazide. She has no allergies. On physical examination, the patient appears confused. Temperature is 38.9 °C (102.0 °F), blood pressure is 104/66 mm Hg, pulse rate is 100/min, and respiration rate is 20/min. Her neck is supple, and she has no rashes. Laboratory studies indicate a leukocyte count of 19,000/µL (19 × 109/L) with 30% band forms and a platelet count of 90,000/µL (90 × 109/L). A non-contrast– enhanced CT scan of the head is normal. Cerebrospinal fluid (CSF) analysis shows a leukocyte count of 1300/µL (1300 × 106/L) with 98% neutrophils, glucose concentration of 20 mg/dL (1.1 mmol/L) (plasma glucose, 120 mg/dL [6.7 mmol/L]), and protein level of 200 mg/dL (2000 mg/L). CSF Gram stain results are negative. After providing adjunctive dexamethasone, which of the following empiric antimicrobial regimens should be initiated in this patient? 1. 2. 3. 4. 5. Ceftriaxone Penicillin G Vancomycin, ampicillin and ceftriaxone Vancomycin plus ceftriaxone 0% 0% Vancomycin plus trimethoprim- sulfamethoxazole 1 2 0% 3 0% 0% 4 5 Meningitis • Most common bacterial causes: – – – – – S. pneumonia (61%) Neisseria meningitidis GBS Haemophilus influenza Listeria monocytogenes Meningitis Diagnosis Meningitis Treatment • Repeat LP if pt not improving at 48hrs on appropriate abx • Dex given with or just before first dose abx Brain Abscess Subdural Empyema Epidural Abscess • Most commonly from contiguous spread (middle ear, mastoid cells, paranasal sinus) • Symptoms: severe ipsilateral headache • Diagnosis: MRI more sensitive than CT • Treatment: emergent surgery and empiric abx • • • • Most commonly from otorhinologic infections (paranasal sinus) Symptoms: meningeal signs and focal neurologic deficit Diagnosis: MRI more sensitive than CT Treatment: emergent surgery and empiric abx • • • • Most commonly from hematogenous spread Symptoms: fever, spinal pain, neurologic deficits Diagnosis: MRI can better visualize spinal cord and epidural space Treatment: surgical decompression, abscess drainage and long term abx Viral CNS Infections Herpes Simplex: • Symptoms: Fever, headache, behavior abnormalities, seizures • Diagnosis: • MRI: Edema and hemorrhage of temporal lobe • LP: HSV PCR (false- negative when hemoglobin in CSF; repeat testing if strong suspicion) • Treatment: Acyclovir West Nile virus: • Symptoms: Tremors, myoclonus, parkinsonism, flaccid paralysis • Diagnosis: • MRI: mixed intensity (hypodense lesions on T1, hyperintense on T2) • LP: IgM antibodies • Treatment: None An 18-year-old woman undergoes evaluation in the emergency department for increasing muscle pain in the left biceps area, nausea, light-headedness, and fever of 3 days’ duration. She was recently diagnosed with varicella virus infection. She admits to having vigorously scratched a lesion in that area and in other areas several days earlier. Vaccinations except for the varicella vaccine are up-to-date. Her only medication has been ibuprofen as needed. On physical examination, temperature is 38.7 °C (101.8 °F), blood pressure is 85/55 mm Hg, pulse rate is 120/min, and respiration rate is 20/min. Skin examination reveals healing varicella lesions. The left biceps area is notable for tenderness, warmth, and “woody” induration to palpation. Hemoglobin 11.0, WBC 20,000; Platelet 75,000; Creatinine 2.0; AST 95; ALT 100 Urinalysis is normal. MRI shows evidence of superficial fascial necrosis between the skin and the biceps muscle. The patient had a single dose of vancomycin and piperacillin-tazobactam before undergoing emergency surgical debridement. Gram stain of the surgically obtained tissue and fluid reveals only gram-positive cocci in short chains. Which of the following treatment regimens should be given now? 1. 2. 3. 4. Intravenous immune globulin Metronidazole and ciprofloxacin 0% Penicillin and clindamycin 1 Vancomycin plus cefepime and metronidazole 0% 2 0% 3 0% 4 Skin and Soft Tissue Infections Infection Treatment Notes Cellulitis Dicloxacillin, Cephalexin S. Aureus, GABHS CA- MRSA TMP-SMX, Tetracycline, Clinda Purulent drainage, abscess Animal Bite Wounds Amoxicillin/Clavulanate Perform tetanus, rabies assessment Human Bite Wounds Amoxicillin/Clavulanate Perform tetanus assessment A 21-year-old man is evaluated in August for a 2-day history of fever, diffuse myalgia, and a mild frontal headache. Recent travel history includes a 2-month hike on the Appalachian Trail completed 10 days prior to presentation. On physical examination, the patient is not ill appearing. Vital signs are normal except for a temperature of 37.9 °C (100.2 °F). Skin examination findings of the lower extremity are shown . A 21-day course of oral doxycycline is initiated, and after100% 2 days, the rash resolves and the patient is asymptomatic. One week after completing therapy, the patient undergoes follow-up evaluation for generalized malaise, diffuse aching, and a mild sore throat. The rash and the fever have not returned. Physical examination is normal. WBC 7600, Hemoglobin 16.4, ESR 14, AST 34, Serologic test for Borrelia Positive Which of the following is the most appropriate next step in treatment? 1. 2. 3. 4. 5. IV ceftriaxone for 4 weeks Oral amoxicillin for 4 weeks Oral atavoquone for 4 weeks 0% Oral azithromycin for 4 weeks 1 therapy 2 No additional antibiotic or antimicrobial 0% 3 0% 0% 4 5 Tick Borne Illnesses • Lyme Disease (Borrelia burgdorferi) – Vector: Ixodes scapularis (deer tick) – Reservoirs: deer, mice – Infection occurs after ticks have fed for at least 36 hours – Treatment: doxycycline Early: Erythema Migrans at 5-14d Serologic Tests are negative Early Disseminated: neurologic and cardiac Late: rheum, neuro or cutaneous at months- years Tick Borne Illnesses • Babesiosis (Babesia microti) – – – – – • Ehrichiosis (Ehrlichia chaffeensis)– – – – – • Vector: Ixodes scapularis (deer tick) Reservoirs: rodents, cattle Symptoms: nonspecific febrile illness Diagnosis: peripheral smear Treatment: quinine + clinda or atovaquone + azithro Vector: Lone star tick Reservoirs: deer, dogs, goats Symptoms: fever, headache and myalgias Diagnosis: peripheral smear Treatment: doxycycline Anaplasmosis (Anaplasma phagocytophilum) – – – – – Vector: Ixodes scapularis (deer tick) Reservoirs: deer, rodents Symptoms: fever, headache and myalgias Diagnosis: peripheral smear Treatment: doxycycline Tick Borne Illnesses • Rocky Mountain Spotted Fever (Rickettsia rickettsii) – Vector: dog and wood ticks – Reservoir: Humans – Symptoms: fever, headache and myalgias; rash at wrist/ankles and centripetally spread – Treatment: doxycyline A 32-year-old female physician is beginning a postgraduate fellowship at a university hospital and must undergo tuberculin skin testing. This is the first time she will have undergone such testing. She is healthy. She grew up in Africa and completed medical school and residency training in London. She received the bacille Calmette-Guérin (BCG) vaccine as 100% a child. Tuberculin skin testing results indicate a 16-mm area of induration at the tuberculin skin testing site. Physical examination is normal. Which of the following is the most appropriate next step in the management of this patient? 1. 2. 3. 4. Chest radiograph Isoniazid, rifampin, pyrazinamide, and ethambutol Repeat tuberculin skin testing in 2 weeks No additional therapy or evaluation 0% 1 2 0% 3 0% 4 Tuberculosis • A history of BCG vaccine should NOT influence interpretation TST. • Treatment: – Active: Rifampin, Isoniazid, pyrazinamide, ethambutol x 2months, then rifampin & Isoniazid x 7 months – Latent: Isoniazid x 9months A 31-year-old man is evaluated for a 12-day history of low-grade fever, pleuritic chest pain, and a nonproductive cough. Two weeks ago, the patient traveled to Phoenix, Arizona, for 3 days to play in a golf tournament. He lives in central Pennsylvania. Medical history is noncontributory, and he takes no medications. On physical examination, temperature is 37.7 °C (100.0 °F). The remaining vital signs are normal. Chest examination reveals occasional bibasilar crackles. 100% The leukocyte count is 7400/µL (7.4 × 109/L) with 52% neutrophils, 32% lymphocytes, 10% monocytes, and 6% eosinophils. Chest radiographs show bilateral small, scattered infiltrates and bilateral pleural effusions. Thoracentesis is performed and yields 300 mL of amber-colored turbid fluid with a leukocyte count of 1200/µL (1.2 × 109/L) with 88% lymphocytes and 12% neutrophils. Gram stain and acid-fast bacilli stain show no organisms. Which of the following is the most likely cause of this patient’s illness? 1. 2. 3. 4. 5. Blastomyces dermatitidis Coccidioides immitis Cryptococcus neoformans Fusarium oxysporum Histoplama capsulatum 0% 1 0% 2 3 0% 0% 4 5 Fungi Infections Fungus Symptom Diagnosis Treatment Cryptococcosis Pulm and CNS Antigen, PCR Fluconazole, Itraconazole, Ampho B Histoplasmosis Pulm Urine Antigen Itraconazole (moderate), Ampho B (severe) Bird, Bat droppings; Great River Vallies Blastomycosis Pulm and Skin Tissue path Itraconazole (moderate), Ampho B (severe) Southeastern US & around Great Lakes & Ohio, MS River Culture, Antibodies Ampho B, Itraconazole, Ketoconazole, Fluconazole Arizona, Cali, New Mexico Coccidioidomyc Pulm osis Notes A 25-year-old man is evaluated in the emergency department for a 3-day history of scrotal pain without fever. Medical history is unremarkable, and he takes no medications. The patient is frequently sexually active with women and never has sex with men. On physical examination, vital signs, including temperature, are normal. Genitourinary examination discloses a purulent urethral discharge and right100% sided scrotal swelling and tenderness, especially superior to the right testis. Duplex Doppler ultrasonography of the scrotum shows normal-sized testes and a swollen right epididymis with normal blood flow. Which of the following is the most appropriate treatment? 1. 2. 3. 4. Ampicillin and gentamicin Azithromycin Ceftriaxone and doxycyline Ofloxacin 0% 1 0% 2 3 0% 4 Azithro or Doxy Ceftriaxone Penicillin G Acyclovir A 29-year-old woman is evaluated in the emergency department for blurred vision, diplopia, slurred speech, nasal regurgitation of fluids, and bilateral upper extremity weakness. The vision disturbances developed yesterday, and the slurred speech and upper extremity weakness began earlier today. Two other patients with similar symptoms are also being evaluated in the emergency department. On physical examination, the patient is alert, awake, and fully oriented. Speech is fluid but slurred. Temperature is 37.0 °C (98.6 °F), blood pressure is 90/60 mm Hg, pulse 100% rate is 50/min, and respiration rate is 12/min. The pupils are dilated, and extraocular movements show bilateral deficits in cranial nerve IV. She cannot abduct her arms against resistance. Complete blood count and routine blood chemistry studies are normal. CT scan of the head is normal. Lumbar puncture is performed; cerebrospinal fluid examination is unremarkable. Which of the following is the most likely diagnosis? 1. 2. 3. 4. Botulism Guillain-Barre syndrome Myasthenia gravis 0% Poliomyelitis 1 0% 2 3 0% 4 Disease Incubation Anthrax 1-60d Smallpox S/Sx Treatment Bioterrorism Ppx Inhalation: Cipro or Doxy febrile flu illness Cutaneous: necrotic lesion Cipro 7-17d High fevers and dense rash Supportive Vaccine if exposed in last 7d Plague (Yersinia) 1-6d Fulminating pneumonia and sepsis Streptomycin, Cipro or doxy Cipro or doxy Botulism 1-8d Descending flaccid paralysis Antibotulinum IG Antitoxin Tularemia 3-5d Febrile, flu-like illness Streptomycin, Cipro or doxy Cipro or doxy A 35-year-old man seeks disease-prevention advice prior to taking a 6-week African safari trip to Tanzania and Kenya, where he will spend time camping in tents. He is generally healthy and takes no medications. All of his basic immunizations are up-to-date. Immunizations for hepatitis A, typhoid, and yellow fever are recommended; prescriptions for traveler’s diarrhea treatment and malaria prophylaxis are provided; risks of travel-related automobile injury100% are discussed; and information about careful contact with dogs is provided. In addition to the steps taken above, which of the following is the most appropriate advice to provide to this patient for his upcoming travel? 1. 2. 3. 4. 5. Avoid carbonated water (soda) Avoid locally made hot tea Sleep under bed netting Use citronella-based insect repellents 0% 0% 0% Wear a facemask on the airplane 1 2 3 4 0% 5 Travel Medicine • Malaria: cyclic fevers, splenomegaly, GI sx – – – – Screened areas from dusk to dawn Sleeping with bed netting (permethrin treated) Insect repellants Chemoprophylaxis with chloroquine when in endemic areas • Typhoid fever: fever and constitutional sx – Treat with fluoroquinolone, 3rd cephalosporin • Traveler’s diarrhea: – Avoid unpeeled fresh fruits and vegetables – Avoid ice from local water – Add sodium hypochlorite or tinture of iodine to water and waiting 30min to consume water – Chemoprophylaxis for high-risk settings with TMP-SMX, doxy, Fluoroquinolones – Can treat severe cases with FQ, azithro but mild cases resolve in 3-5d • Dengue Virus Infection: fever, myalgia, retro-orbital pain; dengue shock syndrome and hemorrhagic fever occur in second infections – Insect repellents – Use of screens during day (no bed netting bc Aedes mosquito active during day only) • Hepatitis A – Vaccinated 2-4 weeks before traveling to an endemic area HIV Opportunistic Infection Infection Symptoms/Diseas e Treatment CD4 Ppx CMV Disseminated or End organ (GI, retina, CNS) Ganciclovir < 50 MAC Disseminated Macrolide and Ethambutol < 50 Cryptococcus Meningitis Ampho B and Fluconazole < 100 Toxoplasmosis CNS Sulfadiazine + Pyrimethamine < 100 TMX-SMP PJP Pulmonary TMX-SMP + steroids < 200 TMX-SMP Azithromy cin HIV Treatment • Goal of therapy to lower HIV RNA viral load to <50 copies • Guidelines recommend initiating HARRT – CD4 < 350 – patient with an AIDS defining illness – HIV nephropathy – Hep B co-infection – Pregnant patients HIV Treatment HIV HAART Complications Metabolic • Lipohypertrophy of abdomen • Lipoatrophy of face, extremities Cardiovascular • Increased risk of CV events; aggressively modify risk factors Immune Reconstitution Inflammatory Syndrome • Clinical deterioration despite immunologic and viral control • Unmasking: in pts with an occult infection • Paradoxical: in pts with previously successfully treated infections Repeated Infections • Congenital IgA Deficiency: multiple sinopulmonary bacterial infections; multiple GI infections (Giardia) • Common Variable Immunodeficiency: repeated episodes of bronchitis and sinusitis, repeated pneumonias, GI infections (Giardia) • Terminal Complement (C5-C9): recurrent Neisseria infections – Check CH50 levels