3.MOLECULAR DIAGNOSIS COURSE - e
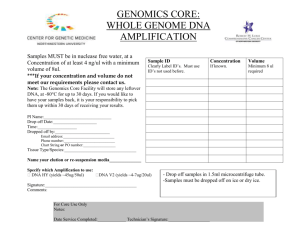
advertisement

1.1 Nucleic acids in human cells There are about 6 billion bases in the human genome, of which 2-5 % code for genes. The majority of the remaining DNA has no known function, and is often referred to as “jund” DNA on the assumption that it is indeed functionless. There are estimated to be in theregion of 35.000 to 70 000 genes in human DNA. The vast majority of hu man DNA is found in the cell nucleus, and this is where most of the information on human genetic disease in this course will be concentrated. However, there is also an important source of DNA in the mitochondria, which are found in the cytoplasm. These organelles have a different arrangement of genes compared to the nucleus and the mitochondrial genome contains only 37 genes. Owing to a high mutaion rate in mitochondrial DNA and the fact that the mitochondrial genome is densely packed with coding sequences, this DNA is more important than might be expected in human genetic disease. Human nuclear DNA is complexed with proteins in the form of Chromosomes. During most of the cell cycle these structures are dispersed in the nucleus but during cell division they condense and can be seen under the microscope with the correct preparative techniques. Normal human cells contain 22 pairs of chromosomes (called autosomes), one of each pair inherited from each parent, plus 2 sex chromosomes which are known as X and Y. Females are XX and males XY. Figure 1.3 shows a diagram of the human chromosome complement, which are numbered in size order from 1 to 22. The chromosomes represented in Figure 1.3 would have been treated with a stain called Giemsa, to give the light and dark pattern known as G banding. Light bands are much more gene rich than the dark bands. Figure 1.3 also shows that chromosomes have 2 arms, with a constriction where they meet called the centromere. The short arm is the p arm (from the French petit), the long one is the q arm (because q comes after p). The centromere is essential for segregation of duplicated chromosomes when they have divided at mitosis. The end of each chromosome arm is called a telomere, and this contains large numbers of repeated lengths of noncoding DNA. These are very variable in number between different individuals, and this variation is one component that is used to produce a “DNA fingerprint”. Most genes are interrupted by noncoding regions as summarized in Figure 1.4. RNA is copied from DNA, and initially this RNA contains both coding and noncoding regions (Figure 1.4). The stretches of RNA which code for amino acids are called exons, and the intervening sequences introns. There are 2 bases at the beginning and end of every intron that are invariant; these are GT at one end and AT at the other. This intron/exon boundary is known as a splice junction, because during processing to produce the final mRNA the intron sequences are spliced out at these points (Figure 1.4). The production of a messenger RNA molecule from DNA is known as transcription (Figure 1.4), and in part this process is controlled by particular sequences of bases upstream of the coding region. These are indicated as ‘promoter’ regions in Figure 1.4. There is an ‘initiation’ codon, AUG, in mRNA, where translation into protein begins in the cytoplasm. Upstream of this site, a specially modified nucleotide, 7-methyl guanosine (termed a ‘cap’) is added immendiately after transcription, and most mRNAs have a series of adenosine molecules added at their 3’ end, the so-called ‘poly(A) tail’. These are the processes referred to as capping and polyadenylation in Figure 1.4. RNA is normally single-stranded and there are three types of RNA molecule in a eukaryotic cell. The most important in terms of genetic disease is mRNA, which carries the coding sequence that the cell recognizes to translate into protein. This translation involves the other two RNA species; ribosomal RNA (rRNA) and transfer RNA (tRNA). The former is a component of ribosomes, where the mRNA is translated into protein, while the tRNA carries the amino acids to the ribosomes, and ensures that the correct amino acid is added as each triplet base code. 1.2 Nucleic acid structure in micro organisms 1.2.1 Viruses Viruses are genetic elements enclosed in a protective coat that allows them to move from one cell to another. Viruses may be subdivided by genome type, into those with: • Double stranded (ds) DNA genomes (including the Adenoviridae), which are amongst the largest of viral genomes; • Single stranded (ss) DNA genomes, typically smal, such as parvovirus. • ds RNA /RNA genomes, (e.g., reovirus); • ssRNA genomes, which can be subdivided into those that funcion as mRNA (positive sense), • and those that are compplementary to the mRNA produced from them (negative sense). • Viruses with RNA genomes that use a DNA intermediate (a provirus) to produce the RNA genome (Retroviridae); • Viruses with DNA genomes that use an RNA intermediate stage to produce a DNA genome (Hepadnaviridae). The replication of RNA viral genomes occurs through the formation of complementary strands, a process that is catalyzed by RNA polymerase enzymes known as replicases. As mentioned above, there are so called negative strand RNA viruses (e.g., influenza) and positive strand viruses (such as polio). The difference is that in the former case the infecting viral RNA does not code for protein; it is only the complementary strand and there must be a preformed replicase present to produce infectious strands. In the case of positive strand viruses the viral strand is coding and can act as a messenger RNA in the cell. Some viruses can replicate in the cytoplasm, or can incorporate into the host cell DNA. The RNA viruses that do this are called retroviruses, such as HIV, where part of the genome codes for an enzyme not present in higher cells; reverse transcriptase. This produces DNA from RNA, and in this way the viral RNA genome can be integrated into that of the cell. 1.2.2 Bacteria Like higher organisms, bacterial genomes are composed of DNA, from which messenger RNA molecules are produced. There are no mitochondria and hence no mitochondrial DNA. However, there are DNA molecules within bacterial cells which can self-replicate. They are called plasmids, and have a small circular chromosome. Plasmid DNA does not usually encode genes with essential functions for the bacteria, they carry resistance genes for antibiotics. There are often multiple copies in each bacterium, and their division occurs independently of the bacterial chromosome. E. coli, one of the best studied bacteria has a circular chromosome of 4.700.000 bases. Unlike human cells, bacterial DNA is not enclosed in a nucleus, but it is centrally located within the organism. About 90% of the bacterial DNA codes for messenger RNAs, compared to about 5-10% in humans. In bacteria, many genes with related functions, such as members of particular metabolic pathways, are clustered together in what are calles ‘operons’. These clusters are transcribed as single messenger RNA molecules. There are no introns in bacterial ge nes, so the process of transcription from DNA to RNA is much simpler with no splicing necessary to remove noncoding regions. Almost all E. coli genes occur as single copies, with the exception of those that code for ribosomal RNA, which in most strains of E. Coli have seven copies. Genetic elements called transposons exist in bacterial DNA (as they do in eukaryotic DNA). These are DNA sequences that code for enzymes which can cause a new copy of the transposon to be inserted into another site of the chromosome. 2.6 Some pitfalls in nucleic acid diagnosis This is especially true of PCR where the sensitivity of the technique can be a real problem .Great care has to be taken, as it is the PCR product, rather than DNA from other individuals, that is the most likely cause of contamination. To minimize the problem, solutions for PCR are prepared in one room, sample is added in another, and the PCR is carried out in another. PCR products are never allowed into the other areas. Some laboratories have different colored lab coats for those people in each room, and different colored pipettes, so it is immediately obvious if anyone or anything is in the wrong place. This may seem excessive, but there are many papers in the literature where positive viral results have proved to be due to contamination. Mutations in the primer sites in PCR can produce anomalous results, especially if they are at the most 3’ position. In this case the primer will almost certainly not amplify, and this can give the appearance of a deletion for this region, whereas it is simply a point mutation. 2.7 Future diagnostic research The use of robotics is certain to increase in the next few years as DNA testing becomes more common. The area where technology will have the greatest impact will be the use of silicon chips . In this method, short oligonucleotides (about 15 bases long) are attached to a silicon chip, and this is used as a hybridization target for an individual’s DNA. Infectious diseases I- viruses 4.1 Introduction Molecular probes have the advantages over conventional methods of speed, specificity and sensitivity.In addition they may be the only applicable techniques as many microorganisms are fastidious and cannot be easily grown . This is particularly pertinent to the study of viruses which, as obligate intracellular parasites, require mammalian cells for their culture. Apart from detection, molecular methods are now becoming standard technologies for establishing viral load, particularly with regard to monitoring treatment, and resistance to antiviral therapy. Table 4.1 shows a comparison of molecular probes with more conventional methods. Viruses are obligate intracellular pararites. They possess either RNA or DNA. From the viewpoint of probe technologies it is useful to know the type of target nucleic acid . In theory it should be possible to diagnose virus infections rapidly by electron microscopy and culture. In practice, the former is insensitive, requiring about 106 virions to be present in a sample, and the latter slow and not always possible. Molecular probes, and gene amplification, overcome these problems and have become routine procedures in the diagnostic setting. 4.2 Sample collection and preparation Nucleic acid from DNA viruses can be processed in a manner not dissimilar to that used for DNA from eukaryotic and bacterial sources. RNA is, however, more labile and specimens containing viral RNA need to be handled rigorously. Containers should be both sterile and treated with diethylpyrocarbonate to minimize RNAse activity. Collection should be undertaken with gloves as RNAse activity is high in sweat and other bodily fluids. The use of RNAse inhibitors may also be required if viral load is low. Extraction of RNA as template requires rigorously controlled conditions and most often employs a guanidiumisothiocyanate (GI ) extraction step. 4.3 Detection of virus 4.3.1 PCR methods For DNA viruses this is straightforward, for RNA viruses an additional reverse transcription step is required either by a separate RT enzyme or a DNA polymerase, such as Thermus thermophilus DNA polymerase, which has RT activity. Human papillomaviruses (HPV) cannot be routinely grown in cell culture and serological assays, are of poor sensitivity and crossreactivity of antigens. These viruses are recognized by their genotype of which more than 120 are now recognized. Certain types of HPV, such as 16 and 18, are strongly associated with the risk of cervical cancer. Other types may be more common but are not oncogenic. PCR studies have shown that up to half of Papanicolaou smear-negative cervical specimens carry HPV, including type 16, suggesting that this is a more sensitive test for determining the risk of subsequent cervical cancer. PCR also allows genotyping with the use of type-specific primers. Other viruses that cannot be grown routinely are shown in Table 4.3. Some viruses can be routinely grown in cell culture but grow so slowly as to be clinically unhelpful. An example of this is the cytomegalovirus (CMV). Standard cell culture techniques can take up to 3 weeks for positive isolation although this can be speeded up by immunofluorescent or enzymatic detection of early antigens in 24-48 hours. Both simple probe and amplification methods have been applied to the detection of CMV. Positive results may occur because of latent virus which is common in adults. In one study in which primers were used that hybridized to regions of the MIE gene (the ‘major immediate early’ antigen gene, an expressed nonstructural product), all 44 culture-positive neonates were PCR positive in their urine but none of the 27 culture-negative neonates were. The most problematic specimen type is blood as the virus is lymphotropic and latent virus can be detected in white cells. Unless there is bleeding into the meninges, however, CSF would not normally be expected to harbor latent virus and its use on CSF of AIDS patients with neurological disorders has shown PCR to be able to detect almost all cases with disease even though cell culture was more commonly negative. With viruses expected to be present in low concentrations, nested PCR is often used and adds to specifity; the increased sensitivity also, however, makes the risk of false positives due to contamination. With specimens which may have a number of different viruses or even mixed infections, multiplex PCR methods have been developed. Specimens such as CSF and respiratory secretions are ideal samples for the use of multiplex PCR as the clinical features are unlikely to identify the causative virus. Another use of multiplex PCR is to type viruses. There are, for example, four serotypes of dengue virus which can cause an illness ranging from simple fever to hemorrhagic fever. It is useful to be able to type this virus as it is recognized that infection with one serotype, following prior infection with another is a risk factor for the serious hemorrhagic fever manifestation. Other Amplification Techniques Following the heels of PCR, a number of alternative in-vitro amplification techniques have been developed, of which some are now available commercially. Examples of these alternative techniques include ligase chain reaction (LCR), nucleic acid sequence based amplification/isothermal amplification (NASBA), and branched DNA probes. Of these techniques, LCR, NASBA and branched DNA are now available commercially in an automated or semi-automated format. A NASBA assay is available for the quantification of HIV-RNA (Organon), and an LCR assay is available for the detection of chlamydia (Abbott). Branched DNA assays are available for the detection of quantification of HIV-RNA, HBV-DNA, and HCVRNA (Chiron). With the exception of the branched DNA probe, all these techniques involve exponential amplification of either the target nuclei acid or the probe. Therefore, they are all as susceptible to contamination as PCR. The branched DNA system is really an intermediate between classical hybridization techniques and the newer in-vitro amplification techniques. It is not as sensitive as those techniques which involve exponential amplification but is considerably more sensitive than the classical hybridization techniques. Below is a brief summary of the features of the different amplification methods available tion method, such as PCR ,LCR can be highly sensitive and is useful for the detection of point mutations. So LCR is useful for the detection of mutations which are frequent in HIV . It depends on the ability of a thermostable DNA ligase to seal nicked double stranded DNA. A method of DNA amplification similar to PCR. LCR differs from PCR because it amplifies the probe molecule rather than producing amplicon through polymerization of nucleotides. Two probes are used per each DNA strand and are ligated together to form a single probe. LCR uses both a DNA polymerase enzyme and a DNA ligase enzyme to drive the reaction. Like PCR, LCR requires a thermal cycler to drive the rxn and each cycle results in a doubling of the target nucleic acid molecule. LCR can have greater specificity than PCR. NASBA amplification pathway. Target ssRNA (in this case, Noroviral genome) binds to Primer 1. An RNA/DNA hybrid is formed by the action of reverse transcriptase. RNaseH then degrades the RNA component of the hybrid and reverse transcriptase using Primer 2 makes a cDNA of the target region. Because Primer 1 contains a T7 RNA polymerase promoter, many copies of the target RNA are made. NASBA reagents are available from Biomerieux under the product name Nuclisens http://www.biomerieux-usa.com/clinical/nucleicacid/index.htm Molecular Beacon probe in the unbound hairpin conformation (upper figure) and in the bound, fluorescent conformation. Amplification of the target sequence can be monitored by fluorescence measurements made every minute. quence. bDNA quantitative assays are commercially available for HBV,HCV and HIV. 4.3.3Molecular epidemiology Viruses evolve through mutation and recombination events at a rate much faster than living organisms; this is greater in those with an RNA genome. As genetic variation is a precursor of antigenic variation, subtler differences can best be detected by genome analysis. Two methods have been commonly employed, PCR-RE (restriction enzymes ) and PCR-single-strand-conformation polymorphism (PCR-SSCP) analysis. The former is also termed PCR-restriction fragment length polymorphism (PCR-RFLP) analysis and is restriction enzyme digestion of PCR amplicons.PCR-SSCP employs a nondenaturing polyacrylamide gel to compare melted single strands of amplicons. In theory a strand with a single base mutation will migrate differently from the non-mutant type. In practice this degree of resolution requires meticulous technique. 4.4 Quantitative viral estimation Quantification of viral load is becoming increasingly important as a means of monitoring antiviral therapy of viruses such as HIV and hepatitis C. It is also used, in HIV infection, as a means for deciding when to start therapy. PCR, nucleic acid sequence-based amplification (NASBA) and branched chain DNA (bDNA) amplification methods have all been applied to quantification of viral load in the clinical setting. Quantitative competitive PCR includes a target sequence mimic which contains a template (control sequence) which is amplified as efficiently as the actual target. Thus a comparison of, for example, HIV-1 target amplification with that of the control allows for a value to be extrapolated. There are a number of different methods that allow differentiation between the two sets of amplicons. The insertion of a restriction site, the inclusion of internal deletions or insertions, or replacement of a portion of the sought sequence by a novel sequence in the control are all used. The last is used in the commercially available system from Roche. This can be enhanced by the use of ‘real-time’ PCR to 50 copies ml-1. NASBA is an isothermal RNA amplification system which has a similar lower limit of detection to PCR. It is available commercially with a linear dynamic range of 102 -107 copies ml-1 when applied to HIV-1 quantification. This is a transcription-based amplification system (TAS), which utilizes 3 enzyme activities: RT, RNAse H and T7 RNA polymerase. An oligonucleotide probe primer is bound to target RNA and the RT makes a DNA copy. RNAse H removes the RNA portion of the RNA-DNA hybrid and allows a second probe primer to anneal downstream. RT then acts as a DNA-dependent DNA polymerase to extend from one probe binding site to the other. One probe primer has a T7 promoter site incorporated so that this enzyme can then produce a further RNA copy to allow the process to start again. Typically a 108 - 109 amplification can be achieved. bDNA amplification does not require an internal control template to be quantifiable. It is a signal amplification method that uses branched chain DNA probes that can then act as substrates for further hybridization reactions if the template is present initially. The technology is licensed by Chiron and has a linear range for HIV-1 of 104 –106 copies ml-1. 4.5 Measurement of antiviral resistance Genotypic determination of viral resistance relies on identification of mutations that confer this state. Thus, it is known that mutations in the UL97 phosphotransferase gene and the UL54 DNA polymerase genes of cytomegalovirus confer resistance to the antiviral drugs, ganciclovir and/or foscarnet. For some viruses, such as HIV which mutates frequently like most other RNA viruses, a battery of probes could be used to look for the common mutations that confer resistance in the RT and protease genes. 4.6 Detection of novel agents of disease The identification of a virus, or any other micro-organism, from patients with a disease is, of course, not sufficient grounds to establish cause and effect. Although not conclusive, the finding of nucleic acid within a diseased cell, but not a normall cell, provides convincing evidence of aetiology. In-situ hybridization enable this. As with other probe methods, in-situ PCR is becoming the advancement of choice. In-situ PCR can be direct or indirect. Indirect methods involve adding standard PCR reagents to the fixed cells and then post-amplification of the products are detected by standard in-situ hybridization. Direct in-situ PCR involves the use of a labeled dNTP in the PCR reaction so that it can detected: a biotin-or digoxigenin dUTP detected by labeled avidin or antidigoxigenin are common examples. VIROLOGICAL METHODS 1. Virus Isolation Viruses are obligate intracellular parasites that require living cells in order to replicate. Cultured cells, eggs and laboratory animals may be used for virus isolation. Although embryonated eggs and laboratory animals are very useful for the isolation of certain viruses, cell cultures are the sole system for virus isolation in most laboratories. The development of methods for cultivating animal cells has been essential to the progress of animal virology. To prepare cell cultures, tissue fragments are first dissociated, usually with the aid of trypsin or collagenase. The cell suspension is then placed in a flat-bottomed glass or plastic container (petri dish, a flask, a bottle, test tube) together with a suitable liquid medium. e.g. Eagle's, and an animal serum. After a variable lag, the cells will attach and spread on the bottom of the container and then start dividing, giving rise to a primary culture. Attachment to a solid support is essential for the growth of normal cells. Primary and Secondary Cultures Primary cultures are maintained by changing the fluid 2 or 3 times a week. When the cultures become too crowded, the cells are detached from the vessel wall by either trypsin or EDTA, and portions are used to initiate secondary cultures. In both primary and secondary cultures, the cells retain some of the characteristics of the tissue from which they are derived. Cell Strains and Cell Lines Cells from primary cultures can often be transferred serially a number of times. The cells may then continue to multiply at a constant rate over many successive transfers. Eventually, after a number of transfers, the cells undergo culture senescence and cannot be transferred any longer. For human diploid cell cultures, the growth rate declines after about 50 duplications. During the multiplication of the cell strain, some cells become altered in that they acquire a different morphology, grow faster, and become able to start a cell culture from a smaller number of cells. These cells are immortalized and have an unlimited life-span. Cell Cultures Cell cultures are separated into 3 types:1. Primary cells - prepared directly from animal or human tissues and can be subcultured only once or twice e.g. primary monkey kidney 2. Semi-continuous diploid cells - which are derived from e.g. human fetal tissue and can be subcultured 20 to 50 times e.g. human diploid fibroblasts such as MRC-5 3. Continuous cells - derived from tumours of human or animal tissue e.g. Vero, Hep2 • Cell cultures vary greatly in their susceptibility to different viruses. It is of utmost importance that the most sensitive cell cultures are used for a particular suspected virus. Specimens for cell culture should be transported to the laboratory as soon as possible upon being taken. Swabs should be put in a vial containing virus transport medium. Bodily fluids and tissues should be placed in a sterile container. • Upon receipt, the specimen is inoculated into several different types of cell culture depending on the nature of the specimen and the clinical presentation. The maintenance media should be changed after 1 hour or if that is not practicable, the next morning. The inoculated tubes should be incubated at 3537oC in a rotating drum. Rotation is optimal for the isolation of viruses and result in an earlier appearance of the CPE for many viruses. If stationary tubes are used, it is critical that the culture tubes be positioned so that the cell monolayer is bathed in nutrient medium. • The inoculated tubes should be read at least every other day for the presence of cytopathic effect. Certain specimens, such as urine and faeces, may be toxic to cell cultures that may produce a CPE-like effect. If toxic effects are extensive, it may be necessary to passage the inoculated cells. Cell cultures that are contaminated by bacteria should either be put up again or passed through a bacterial filter. Cell cultures should be kept for at least one to two weeks (longer in the case of CMV). •Cell cultures should be refed with fresh maintenance medium at regular intervals or if required should the culture medium become too acidic or alkaline. When CPE is seen, it may be advisable to passage infected culture fluid into a fresh culture of the same cell type. For cell-associated viruses such as CMV and VZV, it is necessary to trypsinize and passage intact infected cells. Other viruses such as adenovirus can be subcultured after freezing and thawing infected cells. Cytopathic effects of enterovirus 71, HSV, and CMV in cell culture: note the ballooning of cells. Cytopathic effects of mumps and measles viruses in cell culture: note the formation of syncytia. Influenza and parainfluenza viruses do not ordinarily induce CPE, however they possess haemagglutinins and thus the ability to absorb guinea pig RBCs as they bud from the cell. This phenomenon is known as haemadsorption. Commonly employed cell cultures include primary monkey kidney, LLC-MK2 and MDCK cells. The cell cultures are incubated with a suspension of guinea pig RBCs at 4oC or RT for 30 minutes. The unabsorbed RBCs are then removed and the cell sheet observed microscopically for the presence of haemadsorption. Presumptive identification of virus isolates can usually be made on the basis of the type of CPE, haemadsorption, and selective cell culture susceptibility. For final identification, immunofluorescence, neutralization, haemadsorption inhibition, electron microscopy, or molecular tests are normally carried out. Rapid Culture Techniques e.g. DEAFF test .One of the most significant contributions to rapid diagnosis has been the application of centrifugation cultures to viral diagnosis. The cell culture is stained by monoclonal antibodies for the presence of specific viral antigens 24-48 hours later. The best known example of this technique is the DEAFF test used for the early diagnosis of CMV infection. In the DEAFF test, the specimen is inoculated onto human embroyonic fibroblasts and then spun at a low speed. After a period of 24-48 hours, the cells are then stained by monoclonal antibodies against CMV early antigen. Therefore a rapid diagnosis of CMV infection can be made without having to wait 1-3 weeks for the CPE to appear Haemadsorption of red blood cells onto the surface of a cell sheet infected by mumps virus. Also note the presence of syncytia Susceptible Cell Lines 1.Herpes Simplex HEL),human amnion 2.VZV 3.CMV 4.Adenovirus 5.Poliovirus 6.Coxsackie B 7.Echo 8.Influenza A 9.Influenza B 10.Parainfluenza 11.Mumps 12.RSV 13.Rhinovirus 14.Measles 15.Rubella Vero Hep-2, human diploid (HEK and human diploid (HEL, HEK) human diploid fibroblasts Hep2, HeLa, MK, BGM, LLC-MK2, human diploid,Vero, Hep-2, Rhadomyosarcoma MK, BGM, LLC-MK2, vero, hep-2 MK, BGM, LLC-MK2, human diploid, Rd MK, LLC-MK2, MDCK MK, LLC-MK2, MDCK MK, LLC-MK2 MK, LLC-MK2, HEK, Vero Hep-2, Vero human diploid MK, Vero Vero, RK13 2. Electron Microscopy Virus diagnosis by electron microscopy relies on the detection and identification of viruses on the basis of their characteristic morphology. A major advantage of virus diagnosis by EM is the ability to visualize the virus. Speed is another advantage of EM as the specimen can be processed within minutes of receipt and thus EM can be used as a rapid diagnostic method. On the other hand, the main disadvantage of EM is its inability to examine multiple specimens coincidentally. Secondly, there must be a minimum number of virus particles present (around 106 virus particles per ml for detection) Some viruses may give a non-distinct morphological appearance which may make detection very difficult. Finally, EM is a very expensive service to provide and requires highly skilled personnel. EM has found a particular niche in the detection of fastidious gastroenteritis viruses such as rota, adeno, astro, Norwalk, and Caliciviruses. In addition EM may be used to confirm the results of virus isolation by cell culture such as for parainfluenza viruses. There are two types of EM methods;- direct or immunoelectron microscopy (IEM). With direct methods, negative staining is normally used which requires little special equipment, in contrast to thin sectioning techniques. The specimens may be used directly or the virus particles may be concentrated before negative staining. Immunoelectron microscopy is a means of increasing the sensitivity and specificity of EM and is particularly useful in the following situations;1.The number of virus particles present is small. 2.Many different viruses have different morphology e.g. herpesviruses and picornaviruses. IEM may identify the virus There are 2 types of IEM, simple IEM, where the specimen is incubated with specific antibody before staining in the hope that the antibody will agglutinate the specimen, and solid phase IEM (SPIEM), where the copy grid is coated with specific antibody which is used to capture virus particles from the specimen. Electronmicrographs of viruses commonly found in stool specimens from patients suffering from gastroenteritis. From left to right: rotavirus, adenovirus, astroviruses, Norwalk-like viruses. ELISA ELISA was developed in 1970 and became rapidly accepted. A wide variety of assay principles can be used in ELISA techniques. Currently the most important ones are; 1.Competitive methods 2.Sandwich methods 3.Antibody capture methods Competitive methods One component of the immune reaction is insolubilized and the other one labeled with an enzyme. The analyte can then be quantified by its ability to prevent the formation of the complex between the insolublized and the labelled reagent. Advantages of this approach are that only one incubation step is necessary and that the "prozone effect" at high analyte concentrations cannot occur. Disadvantages are that the concentration range in which the analyte can be quantified without sample dilution is rather narrow and that the antigen or antibody therefore cannot be distinguished in a one step assay Sandwich method The method in which the same component of the immune reaction (e.g. the antibody) is used in the insolubilized and the enzyme in the labelled form. Indirect Method 1.The method in which one component (usually the antigen) is used in an insolubilized form to bind the analyte from the sample (the antibody),which is subsequently determined by addition of labelled second antibody against the same class of antibody as the analyte antibody . Modification of the test in so that antibodies of a specific class such as IgM, can be detected in the sample. Also RF ( rheumatoid factor ) is known to be a potentially interfering factor. Antibody capture methods These methods used to detect antibodies of specific immunoglobulin subclasses, by first reacting the sample with e.g. insolubilized anti-IgM,and subsequently with either enzyme labelled antigen or with antigen followed by enzyme linked antibody. Neither antibodies from other immunoglobulin subclasses nor rheumatoid factor interfere significantly in such assays. They are widely used for the diagnosis of acute infections by IgM detection. These assays may be used for detecting IgG and IgA. Direct Competitive ELISA: operate on the basis of competition between the horseradish peroxidase (HRP) enzyme conjugate and the analyte in the sample for a limited number of specific binding sites on the precoated microplate Competitive or Blocking ELISA In a competitive ELISA, a patient serum and an Ag-specific conjugate (pink) are co-incubated with a captured Ag. The amount of colour developed is inversely proportional to the amount of Ag-specific patient Ig present. Careful standardisation is required to interpret the results In a blocking ELISA, the patient serum is added first, incubated and the excess washed off. Next an Ag-specific conjugate is added and the results interpreted as above. Titres here may be lower if the conjugate is of a high enough titer to displace patient Ab. In a variation of this format, a conjugated Ag is used the competitor. Types of ELISA Direct ELISA Direct ELISA is the most basic of ELISA configurations. It is used to detect an Ag (red triangle; virus/bacteria/fungus, recombinant peptide/protein, or another Ab) after it has been attached to the solid phase (eg. a membrane or Types of ELISA polystyrene microwell or dipstick). Direct ELISA An Ab (green), conjugated with a label (yellow star; eg. HRPO, AP, FITC) is then incubated with the captured antigen. After washing off excess conjugate and incubating with a substrate and chromogen, the presence of an expected colour indicates a specific Ab-Ag interaction. The conjugate could be a commercial prepartion specific for the Ag of interest, or an in-house conjugated monoclonal or polyclonal Ab, or even patient serum. Indirect Once again an Ag is adsorped onto a solid phase. The first, or primary Ab (green) is incubated with the Ag, then the excess is washed off. A second or secondary Ab (blue), the conjugate, is then incubated with the samples. The excess is again removed by washing. For colour to develop, a primary Ab that is specific for the Ag must have been present in the sample (eg. human serum, CSF or saliva or the supernatant from a hybridoma culture). This indiactes a positive reaction. It is important, during assay optimisation, to ensure that the secondary Ab does not bind non-specifically to the Ag preparation or impurities within it, nor to the solid phase. Capture ELISAs Antigen Capture In this, more specific approach, a capturing Ab (orange) is adsorped onto the solid phase. The capture antibody may be the reagent to be tested (eg. the titre of a patients immune response to a known Ag). However, the Ab may be a standard reagent and the antigen the unknown(as when a patients serum is being investigated for the presence of a microbial infection). The same stringent optimisation is required as for Indirect ELISA. This will ensure that the Ab do not cross-react in the absence of Ag, or non-specifically bind to the solid phase. It is also important, when detecting the Ag, to use Ab from different animal species to prevent same-species Ab binding. Antibody Capture In this approach, a capturing Ab (orange) is adsorped onto the solid phase. The Ab is designed to capture a class of human Ab (green; eg. IgG, IgA or IgM). Next the sample is applied, containing the Ab under investigation. After washing, an Ag (red) specific for the Ab is added and finally an antiAg conjugate (blue) provides the signal. Assay Characteristics The use of monoclonal antibodies has lead to many improvements in ELISA systems. 1.Higher sensitivity ;- either by selection of antibodies with a extremely high affinity, which makes very low concentrations of analyte more readily detectable. 2.Higher specificity ;- by avoiding the presence of any antibody in the assay system with specific reactivity against non-analyte epitopes, and by selecting combinations of monoclonal antibodies which may further increase specificity. The enzyme label ; -Most of the assays employ horse-radish peroxidase, alkaline phosphatase, or B-Dgalactosidase. Methods are available to detect horse radish peroxidase by means of chemilumininescence. - TMB is gradually replacing mutagenic substrates such as OPD, leading to increased sensitivity and safety. Microplate ELISA: coloured wells indicate reactivity. The darker the colour, the higher the reactivity Immunofluorescense Immunofluorescence (IF) is widely used for the rapid diagnosis of virus infections by the detection of virus antigen in clinical specimens, as well as the detection of virus-specific IgG or IgA or IgM antibody. The technique makes use of a fluorescein- labelled antibody to stain specimens containing specific virus antigens, so that the stained cells fluoresces . In the case of direct IF, the specimen is probed directly with a specific labelled antibody against a particular virus antigen. In the case of indirect IF, the specimen is first probed with a non-labelled specific antibody, followed by a labelled antibody against the first antibody. Direct or indirect IF can be used for the detection of virus antigen, whereas indirect IF is virtually always used for the detection of antibody. Indirect IF possess the advantage of an extra amplification step for the signal, however, it requires an extra step in comparison to direct IF. Detection of viral antigens Nasopharyngeal aspirates are the best specimens to use and is usually collected from babies less than 12 months old. A number of respiratory viruses can be detected by direct or indirect IF, including RSV, influenza A and B, adenoviruses and parainfluenza viruses. However, the sensitivities vary greatly between different viruses. The method is most useful in the case of RSV ,is also widely used for the detection of HSV infections, from vesicle lesions and for VZV. A typical indirect IF procedure for the detection of viral antigens is as follows; -cells from the clinical specimen are immobilized onto individual wells on a slide. Specific polyclonal or monoclonal sera is then added to each well and the slide is incubated at 37oC for 30 to 60 minutes. The slide is then washed 3 times for 5 minutes each with PBS and fluorescein labelled antibody against the first antibody is added. -The slide is further incubated at 37oC for 30 to 60 minutes and washed again. The slide is then prepared for microscopy. Specific monoclonal or polyclonal sera raised against the viral antigen can be used. Monoclonal sera offer the advantage of increased sensitivity and specificity. However, one must be certain that it can detect all the different strains of the virus. Positive immunofluorescense tests of HSV antigen from epithelial cell and CMV pp65 antigen from peripheral blood neutrophils. Right: Positive immunofluorescense test of rabies virus antigen (CDC) Detection of viral antibodies IF is probably the simplest serological assay to set up. It simply requires virally infected cells that express viral antigens and a fluorescein-labelled antiserum against human immunoglobulin. IF can be used to detect IgG, IgM and IgA. IF is extensively used for the diagnosis of EBV infections . 8. Neutralization Neutralization of a virus is defined as the loss of infectivity through reaction of the virus with specific antibody. Virus and serum are mixed under appropriate condition and then inoculated into cell culture. The presence of unneutralized virus may be detected by reactions such as CPE. The loss of infectivity is bought about by interference by the bound Ab with any one of the steps leading to the release of the viral genome into the host cells. Stable neutralization - with time, Ag-Ab complexes usually become more stable (several hours) . Such neutralization is generally produced by Ab molecules that establish contact with 2 antigenic sites on different monomers of a virion, greatly increasing the stability of the complexes. An example of stable neutralization is the neutralization of polioviruses, whereby, the attachment of the antibody to the viral capsid stabilizes the capsid and inhibits the uncoating and release of viral nucleic acid. Viral evolution must tend to select for mutations that change the antigenic determinants involved in neutralization. In contrast, other antigenic sites would tend to remain unchanged because mutations affecting them would not be selected for and could even be detrimental. Because of its high immunological specificity, the neutralization test is often the standard against which the specificity of the other serological techniques is evaluated. Before the neutralization test is carried out, the components that are to be used must be standardized. To identify a virus isolate, a known pretitred antiserum is used. Conversely, to measure the antibody response of an individual to a virus, a known pretitred virus is used. To titrate a known virus, serial tenfold dilutions of the isolate is prepared and inoculated into a susceptible host system such as cell culture . The virus endpoint titre is the reciprocal of the highest dilution of virus that infects 50% of the host system eg. 50% of cell cultures develop CPE. This endpoint dilution contains one 50% tissue culture infecting dose (TCID50) or one 50% lethal dose (LD50) of virus per unit volume. The concentration of virus generally used in the neutralization test is 100 TCID50 or 100 LD50 per unit volume. The antiserum is titrated in the neutralization test against its homologus virus. Serial twofold dilutions of serum is prepared and mixed with an equal volume containing 100TCID50 of virus. The virus and serum mixtures are incubated for 1 hour at 37oC. The time and temperature for incubation varies with different viruses. The mixtures are then inoculated into a susceptible host system. The endpoint titration contains one antibody unit and is the reciprocal of the highest dilution of the antiserum protecting against the virus. Generally 20-100 antibody units of antiserum is used in the neutralization tests Serology Following exposure, the first antibody to appear is IgM, which is followed by a much higher titre of IgG. In cases of reinfection, the level of specific IgM either remain the same or rises slightly. But IgG shoots up rapidly and far more earlier than in a primary infection. Many different types of serological tests are available. With some assays such as EIA , one can look specifically for IgM or IgG, whereas with other assays such as CFT and HAI, one can only detect total antibody, which comprises mainly IgG. Newer techniques such as EIAs offer better sensitivity, specificity and reproducibility than classical techniques such as CFT and HAI. The sensitivity and specificity of the assays depend greatly on the antigen used. Assays that use recombinant protein or synthetic peptide antigens tend to be more specific than those using whole or disrupted virus particles. Criteria for diagnosing Primary Infection 1.A significant rise in titre of IgG/total antibody between acute and convalescent sera - however, a significant rise is very difficult to define and depends greatly on the assay used. In the case of CFT and HAI, it is normally taken as a four-fold or greater increase in titre. The main problem is that diagnosis is usually retrospective because by the time the convalescent serum is taken, the patient had probably recovered. 1. Presence of IgM - EIA and IF are used for the detection of IgM. This offers a rapid means of diagnosis. 2. However, there are many problems with IgM assays, such as interference by rheumatoid factor, re-infection by the virus, and unexplained persistence of IgM years after the primary infection. 3. Seroconversion - this is defined as changing from a previously antibody negative state to a positive state e.g. seroconversion against HIV following a needle-stick injury, or against rubella following contact with a known case. 4. A single high titre of IgG (or total antibody) - this is a very unreliable means of serological diagnosis since the cut-off is very difficult to define. Serological events following primary infection and reinfection. Note that in reinfection, IgM may be absent or only present transiently at a low level. Criteria for diagnosing re-infection/reactivation It is often very difficult to differentiate re-infection/re-activation from a primary infection. Under most circumstances, it is not important to differentiate between a primary infection and re-infection. However, it is very important under certain situations, such as rubella infection in the first trimester of pregnancy: primary infection is associated with a high risk of fetal damage whereas reinfection is not. In general, a sharp large rise in antibody titres is found in re-infection whereas IgM is usually low or absent in cases of reinfection/re-activation. Limitations of serological diagnosis How useful a serological result is depends on the individual virus. 1.For viruses such as rubella and hepatitis A, the onset of clinical symptoms coincide with the development of antibodies. The detection of IgM or rising titres of IgG in the serum of the patient would indicate active disease. 2.However, many viruses often produce clinical disease before the appearance of antibodies such as diarrhoeal viruses. So in this case, any serological diagnosis would be retrospective and therefore will not be so useful. 3.There are also viruses which produce clinical disease months or years after seroconversion e.g. HIV and rabies. In the case of these viruses, the mere presence of antibody is sufficient to make a definitive diagnosis. There are a number of problems associated with serology: 1.long length of time required for diagnosis for paired acute and convalescent sera 2.mild local infections such as HSV genitalis may not produce a detectable humoral immune response 3.Extensive antigenic cross-reactivity between related viruses e.g. HSV and VZV, may lead to false positive results 4.immunocompromised patients often give a reduced or absent humoral immune response. Antibody in the CSF In a healthy person, there should be little or no antibodies in the CSF. Where there is a viral meningitis or encephalitis, antibodies may be produced against the virus by lymphocytes in the CSF. The finding of antibodies in the CSF is said to be significant when ratio between the titre of antibody in the serum and that in the CSF is less than 50-80. But this does depend on an intact blood-brain barrier. The problem is that in many cases of meningitis and encephalitis, the blood-brain barrier is damaged, so that antibodies in the serum can actually leak across into the CSF. This also happens where the lumbar puncture was traumatic in which case the spinal fluid would be bloodstained. So really, one should really check the integrity of the blood-brain barrier before making a definite diagnosis. One way to check the integrity of the blood brain barrier is to use a surrogate antibody that most individuals would have, such as measles virus, since most people would have been vaccinated. If the blood-brain barrier is intact, there should be little or no measles antibodies in the CSF. Human infectious diseases II bacteria, fungi, and protozoa 5.1 Introduction It is estimated that up to 95% of bacteria present in a sample are noncultivable. Cheaper cultural methods will, no doubt, be used as a standard but there are four areas where nucleic acid based diagnosis will be the method of choice: • The identification and characterization of fastidious organisms; •Rapid typing of isolates for epidemiological and other purposes; •Rapid determination of antimicrobial resistance; • Identification of organisms in a noncultivable state Bacteria are responsible for the majority of currently treatable infectious diseases and because of this an accurate rapid diagnosis and determination of susceptibility to antibiotics is important. In addition, typing is important for epidemiology and, ultimately, control of these organisms. 5.2 Specimen collection and preparation Material collected may range from the sterile, relatively acellular, environment of cerebrospinal fluid to the highly complex milieu of food. The more complex the environment, the more likely that there will be substances that interfere with hybridization or inhibit amplification. Thus, specimens need to be collected in a manner likely to stabilize nucleic acids for transport to the laboratory . Apart from the special circumstance when differentiation between viable and nonviable bacteria is required, DNA is the target and RNAase inhibition is not usually required. Obviously procedures should be as sterile as possible to prevent the addition of exogenous micro-organisms. Further purification before probing or PCR may not be required when bacterial load is likely to be high such as with acute meningitis. If significant nonbacterial contamination is likely, then additional steps to ‘purify’ the bacterial DNA may be required. Proteinase K digestion, alkaline lysis are commnonly used. 5.3 Identification The bacterial genome consists of a circular chromosome. In addition there may be extra-chromosomal elements on plasmids. Methods have been developed which facilitate the detection of chromosomal, plasmid or total DNA in a wide range of bacteria. In addition the advent of more advanced genotypic methods, such as PCR, has enabled the detection of previously undiscovered pathogens. Indeed molecular methods have been important in the understanding of pathogenesis. The use of probes to 16S ribosomal RNA sequences is peculiar to bacterial diagnostics enabling both detection and phylogenetic analysis. CULTURE AND IDENTIFICATION OF INFECTIOUS AGENTS Bacterial identification in the diagnostic laboratory versus taxonomy Isolation and identification of bacteria from patients aids treatment since infectious diseases caused by different bacteria have a variety of clinical courses and consequences. Susceptibility testing of isolates (i.e. establishing the minimal inhibitory concentration or MIC) can help in selection of antibiotics for therapy. When patients are suspected of having a bacterial infection, it is usual to isolate visible colonies of the organism in pure culture (on agar plates), and then speciate the organism. The identification is based on taxonomic principles applied to the clinical microbiological situation. In the diagnostic laboratory, many samples must be characterized each day and results obtained as quickly as possible. Classical methods for speciation of bacteria are based on morphological and metabolic characteristics. There are numerous different tests for each of the many target pathogens. Additionally, molecular biology techniques (for characterization of specific genes or gene segments) are now commonplace in the clinical laboratory. Taxonomic terms (classification) Family: a group of related genera. Genus: a group of related species. Species: a group of related strains. Type: sets of strain within a species (e.g. biotypes, serotypes). Strain: a single isolate of a particular species. The most commonly used term is the species name (e.g. Streptococcus pyogenes - abbreviation S.pyogenes). There are always two parts to the species name, one defining the genus in this case "Streptococcus" and the other the species (in this case "pyogenes"). The genus name is always capitalized but the species name is not. Both species and genus are underlined or in italics. Steps in diagnostic isolation and identification of bacteria Step 1. Samples of body fluids (e.g. blood, urine, cerebrospinal fluid) are streaked on culture plates and isolated colonies of bacteria appear after incubation for one to several days . Each colony consists of millions of bacterial cells. Observation of these colonies for size, texture, color, and (if grown on blood agar) hemolysis reactions, is highly important as a first step in bacterial identification. Whether the organism requires oxygen for growth is another important differentiating characteristic. Step 2. Colonies are Gram stained and individual bacterial cells observed under the microscope. Step 3. The bacteria are speciated using these isolated colonies. This often requires an additional 24 hours of growth. THE GRAM STAIN A colony is dried on a slide and treated as follows : Step 1. Staining with crystal violet. Step 2. Fixation with iodine stabilizes crystal violet staining. All bacteria remain purple or blue. Step 3. Extraction with alcohol or other solvent. Decolorizes some bacteria (Gram negative) and not others (Gram positive). Step 4. Counterstaining with safranin. Gram positive bacteria are already stained with crystal violet and remain purple. Gram negative bacteria are stained pink. Taxonomic characterization of bacteria There is considerable diversity even within a species. Comparisons are primarily based on chemical or molecular analysis. Chemical and Molecular Approaches: •Cell wall composition. •Membrane lipid signatures. •Electrophoretic comparison of proteins. •Nucleic acid hybridisation. •Gene sequence comparisons. Molecular analysis It would be ideal to compare sequences of entire bacterial chromosomal DNA, but this is currently not feasible. Millions of nucleotides have to be sequenced for each strain. In the past several years, sequencing of the entire genomes of one representative (i.e. a strain) of a few bacterial species has been achieved. In each case, this has involved massive amounts of work by large research groups dedicated to the task of sequencing. Alternatively, genomic similarity has been historically assessed by the content of guanine (G) plus cytosine (C), usually expressed as a percentage (% GC). This has been replaced by two alternatives hybridization and sequencing (most commonly of the gene coding for 16S rRNA). DNA-DNA homology is employed to compare the genetic relatedness of bacterial strains/species. If the DNA from two bacterial strains display a high degree of homology , the strains are considered to be members of the same species. DNA from different bacterial species (unless closely related) display no homology. In the last few years, sequencing of 16S ribosomal RNA molecules (16S rRNA) has become the "gold standard" in bacterial taxonomy. The molecule is approximately sixteen hundred nucleotides in length. The sequence of 16S rRNA provides a measure of genomic similarity above the level of the species allowing comparisons of relatedness across the entire bacterial kingdom. Closely related bacterial species often have identical rRNA sequences. Bacterial DNA sequences can be amplified directly from human body fluids (the polymerase chain reaction, PCR). For example, great success has been achieved in rapid diagnosis of tuberculosis. Serologic identification of an antibody response (in patient's serum) to the infecting agent can only be successful several weeks after an infection has occurred. Genotypic Identification Differences in the DNA base sequences between different organisms can be determined quantitatively, such that a phylogenetic tree can be constructed to illustrate probable evolutionary relatedness between the organisms. The nucleotide base sequence of the gene which codes for 16S ribosomal RNA is becoming an important standard for the definition of bacterial species. Comparisons of the sequence between different species suggest the degree to which they are related to each other; a relatively greater or lesser difference between two species suggests a relatively earlier or later time in which they shared a common ancestor. A comparison between species of gram-negative bacteria is illustrated.When the sequences are aligned such that similarities and differences can be readily seen . Gaps and insertions of nucleic acid bases (the result of "frame-shift" mutations occuring over eons of time as the organisms diverge from common ancestors) which affect long stretches of DNA have to be taken into account for a proper alignment. The organisms are as follows: •Neisseria sicca . •Pseudomonas fluorescens. •Three enteric-like organisms: Vibrio cholerae, Photobacterium phosphoreum and Plesiomonas shigelloides. •Three relatively obscure enterics: our new organism (shown by initials "AH" ), Budvicia aquatica and Edwardsiella tarda. •Escherichia coli – the archetypal enteric – with two closelyrelated species, Shigella dysenteriae and Escherichia hermannii. "AH" (our new organism) gataactactggaaacggtagctaataccgcataacgtcgcaagaccaaa gcgggggaccttagggcctcgcgccatcagatgaacccagatgggattag ctagtaggtggggtaatggctcacctaggcgacgatccctaactggtctg agaggatgaccagtcacactgggactgagacacggcccagactcctacgg gaggcagcagtggggaatattgcacaatgggcgcaagcctgatgcagcca tgccgcgtgtgtgaagaaggccttcgggttgtaaagcactttcagtgagg aggaaggcgttgcagttaatagctgtagcgattgacgttactcacagaag aagcaccggctaactccgtgccagcagccgcggtaatacggagggtgcaa gcgttaatcggaattactgggcgtaaagcgcacgcaggcggtttgttaag tcagatgtgaaatccccgggctcaacctgggaactgcatttgaaactggc aggctagagtctcgtagaggggggtagaattccaggtgtagcggtgaaat gcgtagagatctggaggaataccggtggcgaaggcggccccctggacgaa gactgacgctcaggtgcga.agcgtggggagcaaacaggattagataccc tggtagtccacgctgtaaacgatgtcgatttggaggttgtgcccttgagg cgtggcttccggagctaacgcgttaaatcgaccgcctggggagtacggcc gcaaggttaaaactcaaatgaattgacgggggcccgcacaagcggtggag catgtggtttaattcgatgcaacgcgaagaaccttacctactcttgacat ccagagaaggttccagagatgggactgtgccttcgggagctctgagacag gtgctgcatggctgtcgtcagctcgtgttgtgaaatgttgggttaagtcc cgcaacgagcgcaacccttatcctttgttgccagc.acttcgggtgggaa ctcaagggagactgccggtgataaaccggaggaaggtggggatgacgtca agtcatcatggcccttacgagtagggctacacacgtgctacaatggcgca tacaaagagaagcgaacttgcgagagtaagcggacctcataaagtgcgtc gtagtccggattggagtctgcaactcgactccatgaagtcggaatcgcta gtaatcgtagatcagaatgctacggtgaatacgtccccgggccttgtaca caccgccc When a 1308-base stretch of that part of the chromosome which codes for 16S ribosomal RNA was lined up and analyzed to find the extent to which four of the above organisms differed from each other, the percent difference between any two organisms was determined, and the results are summarized as follows: PF PF AH 14.8* AH BA 14.5 3.2 BA ET 14.9 4.3 5.0 ET * An example: The same bases appear in the same sequence, position by position, for each of the two organisms except for 14.8% of the time. With the percent differences used to denote probable evolutionary distances between the organisms, a phylogenetic tree was roughed out to illustrate the relationships. The distances between any two organisms, when read along the horizontal lines, corresponds closely to the percent differences. (The bar at the bottom signifies approximately 1% base difference.) Databases of various gene sequences are found on the web. Genbank's database was used as the source of the above sequences. And rather than having to line up the sequences and determine the differences manually, a set of programs to analyze sequence data and plot trees are available. Numerical taxonomy, the use of computers. The similarity matrix and conversion to dendrogram • •Sequence determinations and construction of gene probes. •Phylogenetic trees from complete sequences. •Prokaryote phylogeny and comparison with conventional classification: Phylogeny rRNA genes are found in all bacteria and mutate at a slow rate. The use of rRNA probes for DNA fingerprinting has been termed ribotyping: labeled probes are generally derived from E. coli 23S, 16S, and 5S rRNA sequences. Current developments use gene amplification. Primers to conserved regions are used to PCR amplify regions that are then identified using genus-specific and species-specific probes. With the proper design of primers it is possible to amplify all genes of a range of bacteria, so-called universal primers. Such primers have been designed to detect a broad range of bacteria, with subsequnt genus and species identification using probes to intervening variable sequences (Figure 5.1). The use of 16S rRNA gene probes has enabled the identification of noncultivable bacteria and, indeed, suggests that only a fraction of the total bacterial species have been identified by cultural methods. Ribotyping It uses so-called universal probes targeted at specific conserved domains of ribosomal RNA coding sequences, allowing characterization with only limited sequence information. Depending on the protocols used, the resultant band patterns can be compared with known species and strains of organisms to determine genetic and evolutionary relationships. Basis of Methodology Strategies can vary widely depending on the sequences selected, the level of information required, and the target organism. Here are some of the key advantages that differentiate this method of DNA typing: 1. The genes for rRNA appear in several different copies at different loci within the genome having different flanking restriction site locations. 2.There is variability among the rRNA genes (16S and 23S). 3.There is variability in the spacer region between 16S and 23S rRNA genes. Related Strategies The amplified fragments are subsequently cut with one or more restriction enzymes and separated by native polyacrylamide gel electrophoresis. The band patterns are compared . This method is also called amplified ribosomal DNA restriction analysis (ARDRA). Direct sequencing of 16S RNA is also commonly employed for similar species and subspecies identification purposes, because it is fairly direct and uncomplicated. Direct sequencing of 16S ribosomal RNA, however, has the disadvantage of the highly conserved nature of the 16S sequence. Thus useful polymorphism in the 16S region is frequently absent at the subspecies level. RAPD Random amplification of polymorphic DNA (RAPD) is a very general method for obtaining a molecular fingerprint of a strain or species. It is a convenient and sensitive method that is finding increasing application in such fields as epidemiology, molecular genetics, microbial ecology, molecular evolution, and taxonomy. Low-stringency PCR amplification of genomic DNA using a single short primer (10–15 bases) of arbitrary sequence is used to generate a set of fragments that is characteristic of the species or strain from which the DNA was prepared. Each fragment in the set results from the fortuitous hybridization of a pair of primers on opposite DNA strands in the appropriate orientation, and separated by such a distance allowing efficient PCR (<1,500 bp). Following electrophoresis and staining, the number of bands in common between a known and an unknown DNA sample can be used for visual estimation of the molecular relatedness of two individuals. By performing similar experiments with different primers and many strains, quantitative data can be derived which can then be used to prepare dendrograms for taxonomic studies. A particular band can also be considered to be a Mendelian "trait" of an organism and can be used as a molecular marker to study the segregation of other traits of economic or clinical significance. In food production and clinical settings, RAPD has been found to be a particularly quick and sensitive alternative to standard bacteriological methods for strain identification, which may take days to perform. The principal advantage of RAPD is that, unlike most other methods of strain identification, it requires no prior knowledge of the organism under investigation. A primer of arbitrary sequence and low-stringency PCR conditions is all that is required to generate information. Of course, some effort is necessary to optimize the amount of information obtained in an experiment, since a particular primer and set of PCR conditions may result in too few or too many bands to be particularly useful. The method is sufficiently simple and rapid, however, that such optimization can be performed in a short time. Because RAPD depends on the identification of common bands between two samples based on their size, the spatial resolution of the electrophoresis method employed contributes significantly to the method's accuracy. The thin polyacrylamide gels however, offer significantly improved resolution over agarose gels for the size range of fragments generated in RAPD. Silver staining is generally recognized to offer greater sensitivity than ethidium bromide. A more serious problem, related to the sensitivity of the method, is reproducibility. Amplification under low-stringency conditions is very sensitive to such factors as quality and quantity of the DNA, primer and magnesium concentration, quality of the polymerase, non accurate quantification of small amounts of DNA, each of which can lead to loss of reproducibility. Digitized RAPD patterns and dendrogram of 18 Acinetobacter genomic species (1 to 18) and 13 clinical Acinetobacter isolates (19* to 31*) obtained after separate PCRs with six different primers. For each strain, all six RAPD patterns have been combined into one single lane (1 to 6). The dendrogram was constructed with Gelcompar cluster analysis by UPGMA. Percentages of similarity and molecular weights are shown above the dendrogram. VNTR/ STR Tandemly repeated sequences are powerful tools for genotyping and linkage analysis. The sequences that are the core of the repeated units represent a relatively wide diversity of size (2–80 bp), sequence, and genome distribution. They are extremely valuable as genetic markers because of their highly polymorphic and abundant presence in the genomes of higher organisms. Tandemly repeated sequences can be broadly categorized into two groups: — VNTRs and STRs based primarily on the size range of the core sequence that is repeated. VNTRs represent repeated sequences that can typically range in length from 10 to 80 bps and are highly polymorphic as to the number of repeats at a given locus. They occur fairly frequently in the genome, but there are relatively few different types. Occurring every few kilobases on average, they are not evenly dispersed throughout the genome, tending to cluster toward the telomeric ends of chromosomes A working VNTR fragment size range is 50 to 1,500 base pairs. These sequences are typically identified using a strategy similar to that of RFLP analysis, where genomic DNA is digested with an endonuclease and separated by electrophoresis. The gels are then analyzed by southern blotting, using sequence-specific probes to the repeated core sequence. Short tandem repeat (STR) sequences, or microsatellites, consist of much shorter (2–10 bp) core sequences whose allelic variants are tandemly repeated as many as hundreds of times at different genetic loci. They are typically more evenly dispersed throughout the genome as compared with the larger VNTRs, and they represent ideal tools as genetic markers because of their rich diversity, wide distribution, and polymorphism. Common repeats used for typing and linkage analysis are "CA" or "ACTT" sequences. Specifically designed as amplification-based detection methods, STR and microsatellite-based DNA typing offer some practical advantages over typing methods based on larger repeat sequences. For example, PCR amplification using primers targeted to a specific STR sequence typically generates 50-to-500-bp-sized fragments without compromising allelic diversity. This allows for easier sizing of a wider range of alleles on a single electrophoretic separation, as compared with larger tandem repeat sequences that typically produce an order-ofmagnitude greater range in fragment size diversity. In addition, the smaller average size of STR and microsatellite alleles allows the technique to exhibit a greater tolerance for crude or partially degraded genomic DNA samples, because the need for longer intact sequence domains is reduced. Variable Number of Tandem Repeat (VNTR) loci are chromosomal regions in which a short DNA sequence motif (such as GC or AGCT) is repeated a variable number of times at a single location (tandem repeat). In this example, Locus A is a tandem repeat of the motif GC: there are four alleles, with two, three, four, or five repeats (A2, A3, A4, and A5, respectively). Locus B is a tandem repeat of the motif AGCT: there are only two alleles, with two or three repeats (B2 and B3, respectively). The example shows a DNA fingerprint that examines both loci simultaneously. Individual #1 is heterozygous at Locus A (A2 / A5) and homozygous at Locus 2 (B2 / B2: note that this genotype gives a single band phenotype in the fingerprint). Individual #2 is heterozygous at both loci: (A4 / A3 and B3 / B2) respectively). The two individuals are distinguishable at either locus.` Locus QUB-11a was amplified by PCR and the products were resolved by agarose gel electrophoresis. Length polymorphisms correspond to multiples of a 69 bp tandem repeat unit. Lanes: 1, PCR negative control; Ma, 100 bp DNA ladder (Promega); 2, M. tuberculosis H37Rv (allele 2); 3, M. bovis AF2122/97 (allele 9); 4, M. bovis 028 (allele 10); 5, M. bovis 029 (allele 10); 6, M. bovis 030 (allele 10); Mb, 100 bp DNA ladder; 7, M. bovis 031 (allele 10); 8, M. bovis 032 (allele 10); 9, M. bovis 033 (allele 9); 10, M. bovis 034 (allele 10); 11, M. bovis 035 (allele 9); Ma, 100 bp DNA ladder; 12, M. bovis 036 (allele 5). 5.3.1 Mycobacteria Slow-growing or fastidious bacteria are particularly appropriate targets for molecular diagnostics . The prime example of the former is Mycobacterium tuberculosis. Traditional methods of diagnosis, as with other bacterial pathogens, have relied on microscopy and culture. Culture on specialized media, such as Lowenstein-Jensen, takes several weeks. Neither method is, however, as fast as PCR-based methods. In the main, PCR-based methods for M. tuberculosis utilize probes to either rRNA or to a repetitive DNA sequence, IS6110. Utilization of the IS6110 target has an inherent advantage, in that, although both M. tuberculosis and the related M. bovis BacilleCalmette-Guerin strain are detected, the differences in copy number of the target sequences within the two organisms results in differing patterns of amplification products. 5.3.2 Other bacteria Many bacteria can exist in both a pathogenic and nonpathogenic state. In this scenario, genotypic methods can be used to detect virulence determinants. An example of this would be the use of toxin gene-specific probes to detect toxigenic strains of Clostridium difficile, a cause of a particular type of diarrhea associated with the use of antibiotics, termed antibiotic-associated colitis . Not all virulence determinants will be chromosomally mediated but probes are equally suited to detect toxin genes on plasmids. Escherichia coli is a Gram-negative bactetium which constitutes much of the bacterial flora of the normal human gastrointestinal tract. Certain strains however carry plasmids that code for toxins that cause diarrhea. 5.3.3 Genotypic vs phenotypic It is now recognised that specific virulence genes are only expressed in the host and not under laboratory conditions.The main drawback of most probe methods that are described in the literature is that they do not differentiate between ‘live’ and ‘dead’ bacteria. The most common approach to resolve this is to detect mRNA by RT-PCR. False positives due to contamination with minute quantities of DNA can be minimized by DNAase digestion of template. 5.4 Commercial systems Most methods are based on PCR for which the world-wide patents are held by Hofmann La Roche, and accrue a royalty payment. These systems (Amplicor®) are semi-automated, based on a PCR-ELISA methodology. Such systems do not require precultivation of organisms. A commercial typing system, Enviro-Amp® for Legionella species in the environment is also available. This kit uses a set of biotinylated primers to conserved regions of 5S rDNA sequences, then species-specific primers which anneal to the Mip gene of Legionella pneumophilia. Identification of amplicons is by hybridization to membrane bound capture probes and subsequent detection by incubation with streptavidin/horse radish peroxidase conjugate in the presence of the substrate, 33΄,55΄ tetramethylbenzidine (TMB). A colorless to blue color change indicates a positive reaction. LCR methods have been developed by Abbott laboratories and have become a commonly used methodology in, for example, the detection of Chlamydia trachomatis in urine. Transcription-mediated amplification (TMA) systems are also available. They can use both RNA and ssDNA targets. 5.5 Typing of isolates 5.5.1 Epidemiology Epidemiological typing of isolates is useful for tracking an outbreak of infection prospectively and for finding a source retrospectively as the aim is to abort the spread of infectious disease. In identification, there are a number of targets for probes: • Chromosomal DNA • Plasmid DNA • Repetitive DNA 5.5.2 Chromosomal DNA Chromosomal DNA is extracted from, ideally, a pure bacterial culture and digested with frequent-cutting restriction enzymes. Subsequent electrophoresis of the fragments results in an RFLP pattern. This technique is not as easily applied to bacteria as it is for some viruses because the much larger genome produces a large number of restriction fragments, some of which may be difficult to resolve on a gel. Instead of using standard gel elecrtophoresis, PFGE has also been used as it results in smaller number of bands and an easier to interpret fingerprint. Gene amplification techniques are now more commonly employed for the typing of microbial isolates. The first described was arbitrarily-primed PCR (AP-PCR) in which an arbitrary primer is used to detect amplification length polymorphisms . This has now been adapted as the RAPD (Random Amplified Polymorphic DNA) method. A short single primer oligonucleotide, is used so that binding is of low specificity to a large number of loci in the target DNA. These primers are typically of random sequence and greater than 60% G:C base ratio. After PCR amplification, complex banding patterns can be visualized in polyacrylamide gels. In theory it is possible to obtain a specific fingerprint for an organism but there are some practical difficulties. The use of short primers necessitates low annealing temperatures. Ramp rates and primer concentrations are crucial to reproducibility. The target DNA may also be polymorphic, and a single point mutation can lead to a different banding pattern. For large genomes, the banding pattern may be also very complex and be difficult to interpret. 5.5.3 Plasmid DNA The plasmids usually characterized are those that confer antimicrobial resistance, termed R (for resistance) factors. These have been shown to be useful epidemiological markers of the spread of nosocomial infection within hospital settings. 5.5.4 Repetitive DNA Repetitive DNA is common in bacterial genomes. The identification of the differing frequency of repetitive sequences at differing positions within the chromosomal DNA allow a ‘fingerprint’ to be established. Rep-PCR involves the PCR amplification of regions of the genome between repetitive elements. Differing sizes of product occur as a result of distance variations between the repeat sequences. The repetitive sequences that code for tRNA are conserved and may have variable intervening genome lengths. With judicious use of primer probes to tRNA gene it is then possible to produce DNA fingerprints with multiple bands or single bands of differing size which can be separated by migration rate on agarose gel electrophoresis. It has been possible to type streptococcal and staphylococcal species by this method. 5.6 Antimicrobial resistance Conventional determination of antimicrobial resistance consists of culture and identification of the organism and determination of growth in the presence of antibiotic as separate procedures. Gene probes can be used to determine the presence of genetic sequences coding for resistance which is plasmid or chromosomally-mediated; if the latter it may be possible to combine detection of the organism and determination of antibiotic resistance simultaneously. A number of genes responsible for antibiotic resistance have now been identified (Table 5.3). One of the best characterized is the mecA gene of Staphylococcus aureus. This gene encodes a penicillinbinding protein and is present in the majority of methicillin-resistant isolates of S. aureus ( MRSA ) but absent in those that are susceptible. In one study, in which the mecA gene was detected using PCR, 42 of 46 isolates of S. aureus and S. epidermidis that were mecA-positive were also methicillin resistant . Such detection enables appropriate infection control measures and antibiotic therapy, if required, to be instituted more rapidly than by conventional methods. 5.8 Fungi The majority of the common fungal causes of human diseases can be rapidly diagnosed by Gram stain. This is cheap and sensitive and would remain the method of choice for candidoses and dermatophyte infections. Molecular probes will, however, have a limited role in diagnostic mycology. Life-threatening infections due to fungi are becoming more prevalent because of acquired immunosuppression due to AIDS and transplantation procedures. Rapid diagnosis of disseminated candidiasis and invasive aspergillosis could be improved by molecular methods. Currently diagnosis depends on culture and/or serology. Both of these are insensitive, slow or both. The use of antigen detection tests speeds up the process but has less than 100% sensitivity or specificity, neither exceeding 70% in practice. Any of the probe technologies that have been described for viruses and bacteria could be applied to the detection of fungi. There are some problems which have particular relevance to the application of such methods to the mycological diagnosis. • The first is that with the serious acute infections, blood is often the most appropriate sample. Blood contains a number of inhibitors of PCR, such as hemoglobin. • Secondly, fungal cell walls are hardy structures and resist release of nucleic acid targets. • The third aspect to be considered in the interpretation of molecular assays is that fungi are very common environmental contaminants and indeed may be present in specimens without probable clinical significance. 5.9 Protozoa The diagnosis of protozoal infection is conventionally made by microscopy or serology. When parasite load is high, microscopy is an adequate methodology for the diagnosis of acute infection. The most frequent protozoal infection world-wide is malaria which is caused by one of four Plasmodium species. Probes, when allied to amplification, have advantages over conventional microscopy when low-level parasitemia occurs and when it is useful to identify drug-resistant mutants. In the vast majority of situations, microscopy will remain the method of choice. Probes to rRNA genes can be genus-or species-specific. They can also be employed to detect mixed infections which are not infrequent. Oligonucleotide rRNA probes are able to detect down to 10-50 parasites in blood spots. PCR detection enables even greater sensitivity. Probes have also been described which detect a 21 bp repetitive sequence, and a number of parasite specific genes. PCR assays have been developed that probe for specific mutations in the dihydrofolate reductase gene that confer resistance to the antifolate drugs (such as proguanil and pyrimethamine). These assays seem to be clinically useful . Techniques such as RAPD-PCR can also be applied to understand the epidemiology of these organisms. Protozoa have hypervariable minisatellite tandem repeat sequences which can be exploited by mini-satellite variant repeat PCR (MVR-PCR) for epidemiological purposes. 5.10 Future prospects The next major advance will be the incorporation of DNA chip technology into routine diagnostics. Probes are bound to a solid phase for detection of unknown, ‘interrogated’, DNA. The use of a solid phase to bind probes is not novel, being used in commercial PCR systems, but DNA chips involve a very large array of probes of known sequence on a solid surface, ‘the chip’.