Pediatric Bipolar Disorder
advertisement

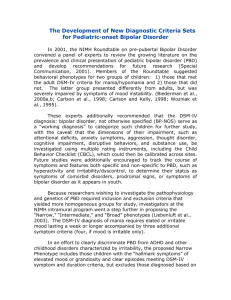
Pediatric Bipolar Disorder Ira Glovinsky, Ph.D. Prevalence Pediatric Bipolar Disorder diagnosis in outpatient clinics increased 40-fold between 1994-2003: 1. A true increase in prevalence; 2. Rectification of previous under-recognition; 3. Changes in conceptualization of the disorder; 4. Inappropriate application of the diagnosis to youth with other illnesses. Should children and adolescents with severe, nonepisodic irritability and symptoms of ADHD be considered to have a developmental presentation of mania? How Pediatric Bipolar Disorder Evolved 1. Aretaeus of Cappadocia (Rome 2nd century)- cyclothymia as a form of mental disease presenting phases of depression alternating with phases of mania…so that mania is like a variety of melancholia. 2. Through the medieval era mania and depression: (a) Continued usually to appear together among diseases of the head; (b) Were grouped together as the two chronic forms of madness; (c) Were described as being without fever; (d) Were presented in adjacent chapters or sections, if not in the same chapter; (e) Mania continued to imply primarily excited psychotic states, and melancholia dejected psychotic states; (f) The basic clinical description changed little. How Pediatric Bipolar Disorder Evolved 3. Jules Baillarger (1809-1890)- la folie à double forme- the existence of a distinct and separate disease with both melancholic and manic phases characterized by regular periods of each. 4. Jean-Pierre Falret (1794-1870)- la folie circulaire- mania changed to melancholia and vice versa, with rational intervals of very short duration. 5. Emil Kraepelin (1921)- “manic-depressive insanity. 6. Theodor Ziehen (early 1900’s) 7. Charles Bradley (1945) 8. John Campbell (1953) 9. E.J. Anthony and P. Scott (1960)- manic-depression is rare in children under 11 years. How Pediatric Bipolar Disorder Evolved 10. Youngerman and Canino (1978)- studied lithium in youth. Response to lithium was poor in those without classic manic-depression. 11. Laufer and Denhoff (1957) described “hyperkinesis” in children. These children were explosive, hyperactive, and distractible, had mood lability and variations in behavior that was more than how we now define ADHD. 12. The “diagnostically homeless.” DSM-III broke off the mood lability symptom from hyperkinesis because it was not felt to be central to ADHD. Children who had mood lability went into the bipolar classification. 13. Using adult bipolar criteria to diagnose children. DSM-IV-TR Criteria for Mania Criteria for a Manic Episode A distinct period of abnormally and persistently elevated, expansive or irritable mood, lasting one week (or any duration of hospitalization is necessary). DSM-IV-TR and ICD-10 Criteria: Focus on Episodes One specifically makes a diagnosis of manic episode in DSM-IV, not mania per se. According to DSM-IV, if one cannot identify distinct episodes, one cannot diagnose mania or hypomania, and by extension, one cannot diagnose bipolar disorder. DSM-IV-TR and ICD-10 Criteria: Focus on Episodes ‘A’ Criteria- a ‘distinct period’ of abnormal mood, lasting the requisite number of days and then returning to a euthymic or subsyndromal state (At least one identifiable period when the mood was different from baseline). ‘B’ Criteria- Concurrent with the change in mood, the patient must have experienced the requisite number of ‘B’ criteria. DSM-IV-TR Criteria for Mania During the mood disturbance, three (or more) of the following symptoms have persisted (four if the mood is only irritable) and have been present to a significant degree: 1. inflated self-esteem and grandiosity; 2. decreased need for sleep (e.g., feels rested after only three hours of sleep); 3. more talkative than usual or pressure to keep talking; 4. flight of ideas or subjective experience that thoughts are racing; 5. distractibility( i.e., attention too easily drawn to unimportant or irrelevant external stimuli; 6. increased goal-directed activity (either socially, at work or school, or sexually) or psychomotor agitation; 7. excessive involvement in pleasurable activities that have a potential for dangerous consequences. DSM-IV-TR Criteria for Mania The symptoms do not meet criteria for a Mixed Episode; The mood disturbance is sufficiently severe to cause marked impairment in occupational functioning or in social activities or relationships with others, or to necessitate hospitalization to prevent harm to self and others, or there are psychotic features; The symptoms are not due to the direct physiological effects of a substance (e.g., a drug of abuse, a medication, or other treatment) or a general medical condition (e.g., hyperthyroidism) Problems With Using Adult Criteria to Define Pediatric Bipolar Disorder 1. “A distinct period….” 2. “Elevated and expansive mood…” 3. “…of one week duration…” 4. What does grandiosity in young children look like? Children have fantasies about magic powers that may seem grandiose. 5. What is the clinical threshold for mania in young children? What is clinical elation versus the extreme of joyfulness? 6. In very young children there are developmentally normal fluctuations in mood. What is fluctuation and what is a cycle? 7. Relationship difficulties can cause mood fluctuations. The Bipolar Controversy I. What are we calling bipolar? A. “Classical” manic-depression is rare- clear episodes of mania followed by depression and euthymia in well-functioning individuals who are okay intermorbidly. B. Children with problems in executive functioning, hyperactivity, and catastrophic rages comprise the bulk of children being called bipolar. The have problems: 1. Inhibiting impulses 2. Shifting attention 3. Controlling emotions 4. Initiating activities 5. Planning/ organizing 6. Self-monitoring C. No one has connected this condition with “classic” manicdepression. Pre-pubertal bipolar children do not change after adolescence and become “classic.” What Does Bipolar Disorder in Childhood Look Like 1. A chronic course 2. Emotional and behavioral dysregulation with pronounced irritability. 3. Irritability is a non-specific symptom in psychiatric disorders in children. The type of irritability observed in pediatric mania is extremely severe and distinct from other forms of irritability seen in other childhood disorders. 4. Among Criterion A (abnormal mood) severe irritability was the predominant abnormal mood rather than euphoria (94% versus 51%). 5. Episodes last hours rather than days. 6. High rates of comorbid symptomatology. Why Is It Difficult To Diagnose Pediatric Bipolar Disorder? 1. Base-rate problem- At any given time, less than 1% of the population samples could be expected to have a manic disorder. 20-30% of children who have psychiatric problems are referred for or receive psychiatric help. Therefore, the typical clinician is likely to have a low rate of exposure to youths with mania, which makes it difficult to form a template of the disorder. 2. Cross-sectional and longitudinal variability of symptoms- Symptoms of mania in childhood are intrinsically labile and there exists gradients of severity within a given episode. A manic episode may go unrecognized if the changeable and labile presentation is not viewed as a salient characteristic of the disorder. Symptoms are not persistent. Why Is It Difficult To Diagnose Pediatric Bipolar Disorder? 3. Symptom overlap of mania with other disorders. 4. Developmental stage and symptom expressionsa. What does elation look like in a four-year-old? b. What does grandiosity look like in a four-year-old? c. What does hyper-sexuality look like in a four-year-old? d. How do you assess racing speech? Subtypes of Bipolar Disorder I. Leibenluft et al (2003) A. Narrow Phenotype- those who meet full DSM-IV-TR diagnostic criteria for mania of hypomania, including duration criteria. B. Intermediate Phenotype 1- hallmark symptoms of elevated mood and grandiosity, of short duration, 1-3 days. C. Intemediate Phenotype 2- episodic irritable mania or hypomania meeting the duration criteria without elation. D. Broad Phenotype- Non-episodic symptoms of severe irritablity and hyperarousal without the hallmark features of elated mood or grandiosity. 1. Non-episodic symptoms of severe irritability; 2. Hyper-arousal without hallmark symptoms of elated mood or grandiosity. What Do Preschool Age Children With Bipolar Disorder Look Like? Tumuluru, R.V, Weller, E.B., Fristad, M.A., and Weller, R.A. (2003) Mania in Six Preschool Children. Journal of Child and Adolescent Psychpharmacology. 1. 36 consecutively hospitalized preschool children. 17% of these children had bipolar disorder. 2. All children had irritable mood. (Ages 3-5 years) 3. Five of six cases also had: (a) a decreased need for sleep; (b) distractibility (c) agitation (d) impaired functioning 4. All had a strong history of affective illness. 5. All six children presented at some point in time with symptoms consistent with attention deficit hyperactivity disorder. Severe mood lability in the context of hyperactivity and impulsivity should raise the suspicion of mood disorder. 6. In all six children mood symptoms were most impairing to the child’s functioning, resulting in hospitalization 7. All five children treated with lithium showed improvement. How Do We Assess Bipolar Disorder? I. From whom do we obtain information? A. Parents1. Family and Developmental History 2. Preschool Age Psychiatric Assessment 3. Childhood Age Psychiatric Assessment 4. Behavioral Assessment Questionnaires (BASC-2) 5. Rothbart Temperament Questionnaires B. Child1. Self-Rating Scale (BASC-2) C. Teacher 1. Teacher Rating Scales (BASC-2) D. Parent-Child 1. Unstructured videotaping of each parent with child scored using the Functional Emotional Assessment Scale (FEAS) How Do We Assess Bipolar Disorder? II. Other Assessment Tools 1. Symptom Checklist 2. Sensory Profile 3. Behavior Rating Inventory of Executive Functions (BRIEF) 4. Intellectual Testing/Neuropsychological Testing 5. Developmental Assessment of Non-verbal Abilities (DANVA) 6. Language Assessment 7. Psychiatric consultation 8. Actigraphy Symptom Checklist Sensory Profile Behavior Rating Inventory of Executive Functions What We Are Learning From Our Work: A Bipolar Signature 1. Sensory profile shows sensory and modulation challenges in almost all areas with most hypersensitivity in vestibular processing. 2. Extremely tuned into their environments; 3. Crave sensory input; 4. Go into “active mode” when overloaded. When they are anxious they seek sensory experiences, including movement in space. 5. As they become more active, craving sensations, sensory overload is increased, escalating the problem; 6. Self-critical, self-blaming behaviors; 7. “All or nothing” thinking; 8. Counter-phobic defenses. 9. Actigraph patterns show shifts in activity level rather than constant activity level, serious sleep disturbances, hemi-circadian rhythms dominate circadian rhythm. At What Age Are We Diagnosing Bipolar Disorder in Children? Faedda, Glovinsky, Austin, & Baldessarini (2004) Measure Males (N=54) Age of 1st Symptom Age of 1st Treatment Age of 1st Bipolar Dx Age of Clinic Assessment Family History Present Adopted Special education 3.2 6.6 9.2 10.1 90.7 16.7 20.4 Females (N=28) 2.2 7.3 10.4 11.5 89.3 21.4 14.3 What Symptoms Do The Children Present? Initial Symptom Males(N=54) Females(N=28) Irritiblity/Moody Sleep Disturbance Hyperactivity Aggressive Anxiety (All Forms) Separation Anxiety Inattention/Racing thoughts Impulsive Hypersexual Pressured Speech Self Harm 44.4 42.6 38.9 33.3 24.1 9.3 7.4 1.9 0.0 1.9 1.9 75.0 50.0 35.7 17.9 10.7 3.6 0.0 3.6 3.6 0.0 0.0 What Is Missing? Greenspan, S.I., and Glovinsky, I.(2002) Bipolar Patterns in Children. 1. A unique pattern of sensory processing in which they evidence sensory oversensitivity to sound and to touch. These children respond to sensory overload with increased sensory craving, particularly with regard to movement, which is usually associated with high activity and aggressive, agitated or impulsive behavior. The more overloaded they feel, the more anxious and agitated they become, which results in even more sensory overload. What Is Missing? 2. An early pattern of interaction, which continues through childhood, characterized by a lack of fully co-regulated reciprocal affective exchanges, especially with regard to “down-” or “up-” regulation to balance states of despondency and agitation. 3. An ego organization in which affects or emotions are either not represented (i.e., remain in a prerepresentational, somatic, or action mode) or are represented as separate affect states (i.e., polarized rather than in an integrated form). We Need to Go Further! I. Emotional Dynamics- A. Reactivity/Latency B. Rise time C. Intensity- (Initial/Peak) D. Lability (changes from one emotion to another, fluctuations between positive and negative emotions, changes in discrete emotions, variations in the intensity of emotion expression. E. Persistence F. Recovery G. Range (Intensity/ Tone) We Need to Go Further! Affective-Social Competence Expression Awareness Identification Social Context Management And Regulation Reception Experience A Developmental Pathway to Very Very Early Bipolar Disorder INTERNAL COMPONENTS EXTERNAL COMPONENTS Neuro-regulatory Mechanisms Behavioral Traits Caregiving & Training A Developmental Pathway to Very Very Early Bipolar Disorder Neuro-regulatory Mechanisms (a) ANS/CNS Reactivity (b) Endocrine activity (c) Sensory sensitivities (d) Temperament factors Behavioral Traits (a) Irritability (b) Low frustration tolerance (c) High reactivity (d) High Intensity (e) Polar emotions (f) Slow emotional recovery (g) Child feels helpless Caregiving & Training (a) Parent matches child’s emotion expression (b) Parent & child spiral out of control (c) Parent tries to exert more control (d) Parent feels helpless A Developmental Pathway to Very Very Early Bipolar Disorder Beliefs & Cognitions Regulatory Style Caregiving & Modeling A Developmental Pathway to Very Very Early Bipolar Disorder Beliefs and Cognitions 1. I must take care of myself; 2. I am powerful; 3. I am a failure; 4. I have to act quickly 5. React first! Regulatory Style 1. Omnipotent; 2. Controlling; 3. Defiant 4. Oppositional Caregiving & Training A Developmental Pathway to Very Very Early Bipolar Disorder INTERNAL COMPONENTS EXTERNAL COMPONENTS Regulatory Style Interactions With Peers A Developmental Pathway to Very Very Early Bipolar Disorder Regulatory Style (a) Coercive/Angry/ Helpless Interactions with peers (a) Ungratifying (b) Rejected (c) Aggressive or Avoiding Things to Think About 1. Psychotherapeutic treatment models for treating mood disorders in children are just beginning to be developed and are generally modeled on adult models. 2. Early-onset mood disorders derail a child and parent at the primary functional emotional developmental levels of: (a) attention and regulation, (b) engagement, (c) two-way coregulated affective chains of communication; (d) behavioral organization. 3. Medication with children helps about 40% of children. Even with medication we need a model that addresses core developmental capacities. 4. Parent and child development is so severely derailed that we need a model that repairs parent/child relationships at the earliest levels of development. 2. Early-onset bipolar disorder derails a child and parent at the primary functional emotional developmental levels of: (a) attention and regulation, (b) engagement, (c) two-way co-regulated affective chains of communication; (d) behavioral organization Things to Think About 5. Intervention must consider: (a) Neuro-regulatory mechanisms ANS/CNS reactivity (b) Sensory Profiles (c) Temperament Match or Mismatch (d) Emotional Regulation Dynamics - Reactivity and Rise Time - Initial Intensity/Peak Intensity - Child and parent’s range of emotions - Lability of emotions - Recovery from upset states (e) Level of emotional competence Psychotherapy with Young Children Diagnosed with Bipolar Disorder 1. See mother and child simultaneously. 2. Focus on the dyadic interaction and the “dance” between parent and child. 3. Work on the rhythm, tempo, and pacing of the “dance.” 4. Work on spontaneous back-and-forth verbal and non-verbal communication. 5. Make sure child understands mother’s communication. 6. Work on “matching” and “balancing” the interaction. 7. Help mother to “down-regulate” as child “up-regulates.” 8. Meet with parents to review taped therapy sessions. 9. Work with mother in adult therapy to help with grief and loss. 10.Work closely with parents and educational professionals in a “tripartite” model. Things to Think About 7. Mood disorders derail a parent’s self-confidence and positive feelings about being a parent. a. Parents experience unpredictable traumatic experiences. They are afraid to take their children outside and to places typically populated by children and parents. b. Because there are so few adults who understand the illness, parents tend to feel alone and isolated. c. Parents feel rage that they fear will come out when they are with other family members and friends. d. Parents feel fearful of their own safety as well as the safety of the child. They are often needing to use control measures that evoke feelings of shame and guilt. Things to Think About 6. Clinicians often do not recognize the “traumatic effect” of mood disorders on the parent and siblings. Parents experience an affective state that is similar to post-traumatic stress. They are fearful of interactions. We need to work on the basics of emotional interactions focusing on the “dancing dialogue” and considering: (a) the rhythm of the interaction- the way verbalizations and actions are grouped together, e.g., the movements are smooth and the back-and-forth interaction is even. (b) the tempo of the interaction- e.g., fast vs. slow, overstimulating vs. under-stimulating. (c) contour of the interaction- e.g. bursts of interaction, sluggishness, attentiveness of parent, spacing, etc. Why Is Early Intervention Important? 1. “Kindling” Effect 2. Severity- Modest episodes become more profound. 3. Frequency- Inter-episode periods become more abbreviated. 4. Autonomy- Cycling initially occurs after a stressor; they subsequently develop spontaneously. 5. Tolerance- Previously effective therapies may not work. 6. Refractoriness- discontinuation of a previously effective medication can lead to relapses that no longer respond to the previous agent. 7. Ultradian fluctuations- Extreme rapidity of cycles can occur at later stages, but may also be characteristic of the earliest forms. 8. Polypharmacy- Later in the course of the illness affective episodes may not respond to a single medication. Severe Mood Dysregulation: Inclusion Criteria Inclusion Criteria Aged 7-17, with the onset of symptoms before age 12; Abnormal mood (specifically anger and sadness), preent at least half the day most days, and of sufficient severity to be noticeable by people in the child’s environment (e.g., parents, teachers, peers). Hyper-arousal, as defined by at least three of the following symptoms: insomnia, agitation, distractibility, racing thoughts or flight of ideas, pressured speech, intrusiveness. Severe Mood Dysregulation: Inclusion Criteria Compared to his/her peers, the child exhibits markedly increased reactivity to negative emotional stimuli that is manifest either verbally or behaviorally. For example, the child responds to frustration with extended temper tantrums (inappropriate for age and/or precipitating event), verbal rages, and/or aggression toward people or property. Such events occur, on average, at least three times a week. The symptoms above are currently present and have been present for at least 12 months without any symptom-free periods exceeding two months. The symptoms are severe in at least one setting (i.e., violent outbursts, assaultiveness at home, school, or with peers). In addition, there are at least mild symptoms (distractibility, intrusiveness) in a second setting. Severe Mood Dysregulation: Exclusion Criteria The individual exhibits any of these cardinal bipolar symptoms: 1. Elevated or expansive mood; 2. Grandiosity or inflated self-esteem; 3. Episodically decreased need for sleep. The symptoms occur in distinct periods lasting more than one day. Meets criteria for substance use disorder in the past three months; IQ at or below 70; The symptoms are due to the direct physiological effects of a drug of abuse, or to a general medical or neurological condition.