PowerPoint Presentation - Epilepsy Center for Kids
advertisement

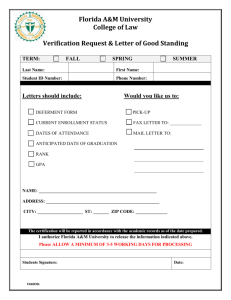
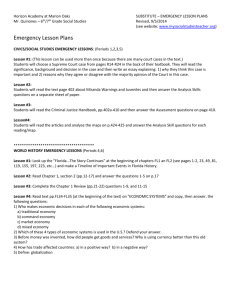
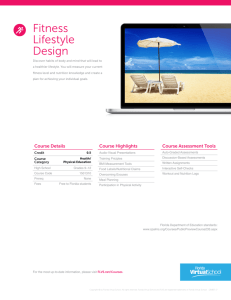
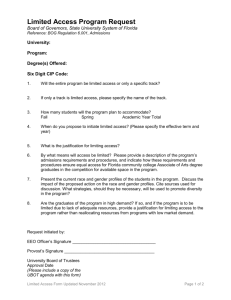
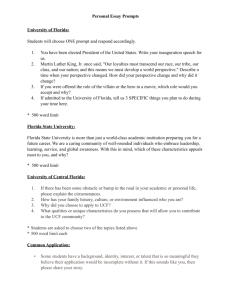
Cingulate Epilepsy Manifesting as Panic Disorder: Multimodal Approach to Diagnosis Michelle Tall, 1Functional 1 RN ; Milena Korostenskaja, 1,2,4 PhD ; 3,4 PsyD ; 3,4 PhD, ABPP-CN ; Tanya R. Grace, Michael Westerveld, Joo-Hee Seo, 3,4 4 Christine M. Salinas, PsyD ; Ki Hyeong Lee, MD 4 MD ; Jane C. Cook, 5 DO ; Po-Ching Chen, 1,2,4 PhD ; Brain Mapping and Brain-Computer Interface Lab, Florida Hospital for Children, Orlando, Florida; 2MEG Lab, Florida Hospital for Children, Orlando, Florida; 2Dirivion of Neuropsychology, Florida Hospital for Children, Orlando, Florida; 4Comprehensive Pediatric Epilepsy Center, Florida Hospital for Children, Orlando, Florida; 5Department of Radiology, Florida Hospital, Orlando, Florida INTRODUCTION Background & Significance Anterior Cingulate Epilepsy (ACE) is a diagnostic and therapeutic challenge with a wide range of nonspecific symptoms that can negatively impact an individual’s cognition, behavior, and emotions. Scalp EEG and brain MRI may not be helpful because of the deep midline location of Anterior Cingulate Gyrus (ACG). Study Aims Primary objective: To demonstrate the utility of a multimodal approach to diagnose ACE. Secondary objective: To raise awareness to the medical community about the complexity of this disorder and associated treatment delay. Patient #2 Baseline: Previous EEG and brain MRI was reported as normal. Patient’s typical episode was associated with diffuse bilateral rhythmic spikes (Fig. 3A). Ictal SPECT and SISCOM demonstrated focal hyperperfusion in the left ACG and medial frontal region (Figure 3B). Neuropsychological evaluation revealed cognitive impairments associated with frontal lobe dysfunction. RESULTS Patient #1 Evaluation: Previous EEG and 1.5T-MRI was reported as normal. Patient’s typical episode was captured during long-term video-EEG that showed diffuse ictal onset (Fig 1). 3T-MRI revealed high T2 signal in the right anterior cingulate gyrus (Fig. 2.A). SISCOM demonstrated a significant focal hyperperfusion in the right medial parafalcine frontal lobe and cingulate gyrus (Fig. 2.B). Neuropsychological test scores were normal. Follow up: Patient is seizure-free with topiramate monotherapy. Follow up: Patient became seizure-free with oxcarbazepine monotherapy. METHOD Setting & Design A retrospective chart review was conducted on two pediatric patients at the Comprehensive Epilepsy Center at Florida Hospital for Children. This study was approved by IRB at Florida Hospital. Subjects Patient 1: 3 year old, previously healthy female was diagnosed with panic attacks by her pediatrician. She presented with daily episodes of intense fear coupled with screaming and inconsolable crying that developed 5 weeks prior to admission. Fig. 3. Patient #2. A: Ictal EEG pattern arising from left frontal and midline vertex areas on long-term video-EEG monitoring; B: Ictal SPECT and SISCOM demonstrated focal hyperperfusion in the left medial parafalcine frontal lobe and ACG. CONCLUSIONS Fig. 1: Ictal EEG showed diffuse bilateral rhythmic spikes with frontal dominance. • Patient 2: 13 year old male was initially diagnosed with panic disorder by his primary neurologist. In addition, at age 7, he was diagnosed with recurrent seizures characterized by sudden frightened facial grimaces, followed by episodes of hyperventilation, repetitive wrist slapping, and walking in circles. • • Comprehensive Epilepsy Evaluation: • Long-term video-EEG monitoring • 3T-MRI with epilepsy protocol • FDG-PET, subtraction ictal SPECT co-registered to MRI (SISCOM) • Neuropsychological testing • Fig. 2. Patient #1. A: 3T-MRI revealed high T2 signal in the right medial frontal lobe cingulated gyrus; B: SISCOM demonstrated a significant focal hyperperfusion in the right medial parafalcine frontal lobe and cingulate gyrus. ACE can be misdiagnosed as generalized anxiety, behavioral problems, or other psychiatric conditions because of diverse clinical manifestation of ACE. Early identification of ACE can improve outcomes in cognition, behavior, and quality of life. MRI and EEG alone may not be sufficiently sensitive for diagnosis and localization of ACE in some cases. Our findings indicate that a combined multimodal diagnostic approach is useful for the diagnosis of ACE.