MELANOMA Sentinel Lymph Node Evaluation: Current Status
advertisement

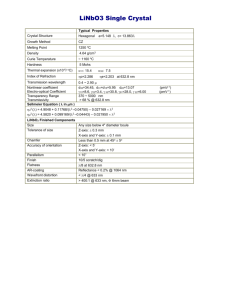
MELANOMA Sentinel Lymph Node Evaluation: Update Kim James Charney, MD Conflict of Interest None Objectives Sentinel lymph node (SLN) biopsy concept and technique Impact of SLN metastasis on recurrence and survival in melanoma Implication of isolated SLN tumor cells in melanoma SLN tumor burden Necessity of completion lymph node dissection (CLND) Candidates for SLN biopsy Stage I & II 85% of newly diagnosed patients Surgical Management of Stage I and II Goals Accurate Staging Assess risk for recurrence Recommendation for therapy Durable Local/Regional Control Cure Minimize Morbidity Stage I and II Primary Melanoma Components of Treatment Wide Excision Margins appropriate for thickness Regional Nodes? Lymph Node Involvement and Melanoma Regional nodes, most common site of first recurrence >50% chance for distant relapse 15-50% chance for in-basin failure after lymph node dissection for palpable disease Approach to the Clinically Negative Regional Basin Observation-----------------------Therapeutic Dissection ELND Intermediate thickness Selective lymphadenectomy Lymphatic mapping and sentinel lymph node biopsy Only pt’s with metastases are dissected Morton, DL, et al. Arch Surg. 1992; 127:392-399 Sentinel Node Biopsy Published Findings SLN identification rate: 99% Dual modality technique Blue dye Radio-colloid injections and gamma probe Accurately stages regional nodal basin Concomitant ELND:FNR < 5% Follow-up of SLN-neg. patients: ~3% will develop nodal disease Facilitates the use of sensitive pathologic techniques Sentinel Node Biopsy Goals Improve disease outcome for node positive patients Regional control Survival Prevent the development of clinical nodal involvement Minimally invasive approach to nodal staging Staging Prognostic Relevance 2010 AJCC Staging Changes Stage I and II (clinically localized) Stage III (regional) Thickness Ulceration Mitotic Rate >1/mm2 SLN status? Nodes In-transit disease Ulceration Stage IV (distant) Site LDH AJCC MELANOMA STAGING DATABASE Survival Curves for Stage I & II 1.0 0.9 (1) (2) Proportion Surviving 0.8 Ia Ib 0.7 (3) (4) (5) 0.6 IIa (7) 0.5 (6) 0.4 (8) 0.3 0.2 IIb IIc Non-ulcerated Ulcerated 0.1 0 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 Survival, years Balch CM, et al. J Clin Oncol. 2001;19(16):3622-3634. Incidence of SLN Metastases MDACC Database Tumor Thickness (mm) < 1.00 1.01-2.00 2.01-4.00 4.01+ Total Total No. Patients (N) 326 490 310 190 1316 All (%) 4.2 11.4 28.5 45.5 17.4 Positive SLN non-Ulcerated (%) 3.9 10.8 23.1 34.2 11.9 ulcerated (%) 12.5 21.2 37.0 55.4 37.0 Ross, MI. Clin Cancer Res. 2006;12: 2312s-2319s. 2008 AJCC Melanoma Database Stage I Survival Rates for T1 Patients (0.01-1.00 mm) According to MR (per mm2) Survival Rate Thickness MR 5-Year 10-Year n (mm) 0.01-0.50 0.01-0.50 0.51-1.00 0.51-1.00 <1.0 >1.0 <1.0 >1.0 99% 97% 98% 94% 97% 95% 93% 87% 1,194 327 1,472 1,868 2009 staging rule: T1b melanomas defined as ≤1.0 mm with ulceration or >1 mitosis / mm2 The original source for this material is the AJCC Cancer Staging Manual, Seventh Edition (2010) published by Springer Science and Business Media LLC, www.springerlink.com. Impact of MR on SLN Positivity Currently, the T1b designation is used for staging in terms of survival Is not itself a criterion to perform SLNB Evolving data suggests that MR may be predictive of occult regional nodal disease Andtbacka RH et al: SLNB in thin melanoma Suggests that SLNB is appropriate for patients with T1b melanomas, including those defined by MR Await publication of a larger analysis of patients with thin melanoma Andtbacka RH, Gershenwald JE. JNCCN. 2009;7:308-317. Prognostic Factors Influencing Disease-Specific Survival _____________________________________________________________________________ Multiple covariate Prognostic Factor Univariate Hazard Ratio p-value Age NS NS Sex NS NS Axial location .03 NS Tumor thickness <.0001 1.1 .04 Clark level > III .001 2.3 .01 Ulceration <.0001 3.3 <.0001 SLN status <.0001 6.5 <.0001 _____________________________________________________________________________ Several large single institution and multi-center databases provide consistent findings Disease-Specific Survival by SLN Status Most powerful predictor of survival Morton DL, et al. N Engl J Med. 2006; 355: 1307-1317 Does early treatment of lymph node disease improve survival? Randomized Surgical Trials Comparing ELND vs. Nodal Observation Pt’s. Thickness Site WHO Program Trial #1 Trial #14 533 227 All >1.5mm Extremities Trunk Mayo Clinic 171 All Extremities Trunk Intergroup Melanoma Trial 737 1-4mm All Not all patients benefit Long Term Results of ELND Trials 2 contemporary ELND trials with survival benefits for patients with microscopic disease Survival According to Status of Regional Nodes Cascinelli. Lancet 1998 German Retrospective Review Impact of Sentinel Node Biopsy on Survival for Node-Positive Patients SLNE: Sentinel Lymph Node positive Elective node dissection DLND: Delayed Lymph Node Dissection Kretschmer et al, Eur J Cancer. 2004; 212-218. ELND Trial Outcomes Conclusions No overall survival benefit Early dissection has no impact on the natural history of primary melanoma Incidence of node positive patients too low to adequately test the hypothesis Survival benefit observed in the node positive and other stratified subgroups MSLT-I: Immediate vs. Delayed CLND for Nodal Metastases Biopsy-proven Melanoma > 1mm Randomized 60% 40% WEX + SNB WEX + Watch & Wait Observation A: Comparison of all randomized patients SN(-) Observation SN(+) Immediate CLND Nodal Recurrence Delayed CLND B: Comparison of randomized patients with SN occult vs. palpable nodal metastases Morton DL, et al. N Engl J Med. 2006; 355: 1307-1317 MSLT-1 5-year Survival Benefit Estimates Based on previous trial observations WHO: 20% survival advantage in the microscopic node positive German multi-center trial: 15% benefit in SLN positive group Assuming 20% incidence of node positivity Overall 3%-4% survival benefit Morton DL, et al. N Engl J Med. 2006; 355: 1307-1317 Impact of Sentinel Node Biopsy on Relapse-Free Survival 5-year disease-free survival • • • 73.1% vs 78.3%, p=0.009 Median follow-up 59.8 months 26.8% patients on observation arm with relapse at any site 20.7% patients on sentinel node biopsy arm with relapse at any site Morton et al. N Engl J Med. 2006;355:1307 MSLT-I: Immediate vs. Delayed CLND for Nodal Metastases Biopsy-proven Melanoma > 1mm Randomized 60% 40% WEX + SNB WEX + Watch & Wait Observation A: Comparison of all randomized patients SN(-) Observation SN(+) Immediate CLND Nodal Recurrence Delayed CLND B: Comparison of randomized patients with SN occult vs. palpable nodal metastases Morton DL, et al. N Engl J Med. 2006; 355: 1307-1317 Stage Progression to More Advanced Nodal Disease Among “Watch and Wait” Patients vs. SNB 70% 4 3.4 Mean # Pos. Nodes 3 2 1.6 SNB 1 % SNB (+) or Nodal Recur. Watch 60% 67% SNB P=0.0001 50% 41% 40% Watch 32% 28% 30% 27% Watch SNB Watch 20% 5% 10% SNB 0% 0 Rx 1 Node N1 2-3 Nodes N2 AJCC N Stage > 4 Nodes N3 MSLT-I: Impact of Sentinel Node Biopsy on Survival for Node-Positive Patients All 2001 Patients Randomization SLNB + OBS - - Early TLND 72% 5-year survival + Delayed TLND 52% 5-year survival P= 0.004 multivariate model adjusted for known prognostic factors Morton DL, et al. N Engl J Med. 2006; 355: 1307-1317 MSLT-1 Node + Subgroups Reasons for Survival Differences False positive SLN's SLN group prognostically more favorable Early dissection prevents regional progression and distant dissemination False Positive SLN? % Node (+) or Nodal Recurrence Incidence of SN Metastases at SNB vs. Clinical Nodal Recurrence following “Watch and Wait” 40.0% 35.2 35.5 P=0.8329 30.0% 19.8 20.0% 16.2 20.3 16.4 SNB Watch 10.0% 0.0% 1.2-3.5 >3.5 Overall Breslow Thickness (mm) Cumulative Incidence of Regional Node Metastasis Morton et al. N Engl J Med. 2007;356:418-421 AJCC 2009 Stage III Changes Concept of ITCs as node-negative disease [N0(i+)] no longer used Scheri et al: 214 SLN+ patients, 57 had ITCs (≤ 0.2 mm) Akkooi et al: 388 SLN+ patients, 40 (10%) had metastases <0.1 mm CLND 6 (12%) additional + nodes, 5-yr melanoma-specific survival LOWER in ITC+ patients than SLN- patients (89% vs 94%, P=.02) 1 (3%) with additional + nodes, 5-yr OS 91% = to SLN- patients Bottom line: It remains unclear whether ITCs in the regional nodes are of clinical significance BUT, concept of “clinically insignificant nodal disease” unproven Scheri RP et al. Ann Surg Oncol. 2007;14:2861-2866. van Akkooi ACJ et al. Ann Surg. 2008;248:949-955. Microscopic metastases will become Macroscopic Do the AJCC staging criteria apply to patients with microscopic SLN tumor burden? Revised AJCC Staging System Stage III Changes Independent Prognostic Factors AJCC Cox Model – 1151 Stage III Patients Variable Number of (+) Chi Square P-Value Risk Ratio 57.6 <0.00001 1.26 Tumor Burden 40.3 <0.00001 1.79 Ulcer + 23.3 <0.00001 1.58 Nodes 6th Edition - 2002 Balch CM et al. J Clin Oncol. 2001; 19(16):3622-3634. Disease-Specific Survival Total # Positive Nodes SLN Positive Patients Only Gershenwald JE et al. WHO 6th World Congress on Melanoma; September 2005; Vancouver, BC. Disease-Specific Survival by Ulceration SLN Positive Patients Only Gershenwald et al, Ann Surg Oncol. 2000;7:160 Disease-Specific Survival by Tumor Burden Largest Focus SLN-Positive Patients Only Gershenwald JE et al. WHO 6th World Congress on Melanoma; September 2005; Vancouver, BC. Survival According to Tumor Burden in SLN’s Ross MI. New AJCC Recommendations for Melanoma Staging. Presented at: 33rd ESMO Congress Satellite Symposium: Current Trends in Melanoma Management; September 14, 2008; Stockholm, Sweden. Prognostic Factors Influencing DSS SNL Positive Patients Only Prognostic Factor Ulceration Total Positive Nodes 1 2 3+ Largest SLN metastatic focus < 2mm >2 & < 8mm > 8mm Multiple covariate Hazard Ratio p-value 2.04 .01 1.0 1.46 2.10 .25 .045 1.0 2.51 2.91 .004 .01 Fifteen-year Survival Curves for the Stage Groupings of Patients with Regional Metastatic Melanoma (Stage III) From Balch, C. M. et al. CA Cancer J Clin 2004;54:131-149. Copyright ©2004 American Cancer Society Completion Node Dissection for Positive Sentinel Nodes: Is it necessary? Staging Survival Regional Control Regional Recurrence After Surgery Alone Reference Regional Failure Rate Fuhrmann,2001 Kretschmer, 2001 Lee, 2000 Shen, 2000 Hughes, 2000 Monsour, 1993 28% 34% 30% 14% 25% 52% Miller, 1992 12% O’Brien, 1991 Calabro, 1989 Bowsher, 1986 Byers, 1986 24% 17% 15% 16% Weighted average: 692 failures/3350 patients= 21% Risk Factors for Regional Recurrence After Surgery Alone Regional Failure Rate Characteristic References Extracapsular extension 31% - 63% Lee, Calabro, Shen, Monsour >4 involved lymph nodes 22% - 63% Lee, Calabro, Miller, Kretschmer Lymph node >3 cm 42% - 80% Lee Cervical ln location 33% - 50% Lee, Bowsher, Monsour 30% - 50% if high-risk features present In-Basin Failure % Nodal Failure Selective Lymphadenectomy vs. ELND (Node Positive Only) 9 8 7 6 5 4 3 2 1 0 ELND Slingluff, 1994 SLN MDACC Study, 2003 Rational For Completion Dissection Avoid the development of palpable nodal disease - residual microscopic disease in non-sentinel nodes Staging - total number of nodes involved prognostically relevant - may influence recommendations for adjuvant therapy Incidence of non-sentinel node involvement under-estimated - based on routine pathologic techniques Reasons Against Routine Use of Completion Dissections Incidence of non-sentinel node involvement is only 10%-20% - unnecessary cost and morbidity in patients without additional microscopic disease No proven survival benefit for node dissection Incidence of nodal failure after SLN biopsy A selective approach to completion dissection is rational. Recommendations CLND for a positive SLN is the standard of care Omission of CLND should only occur as part of a clinical trial SLN Biopsy Indispensable Staging Procedure? Effectively identifies microscopic disease/Promotes early node dissection Identifies patients who benefit most with adjuvant therapy Facilitates careful pathologic scrutiny survival benefit optimizes regional control Node negative patients spared toxicity Critical prognostic information Stratification criteria for clinical trials Candidates for SLN Biopsy Incidence of Positive SLN: AJCC Stage Grouping 55.4% Percent Positive SLN 60 50 40 35.3% 30 22.1% 20 11.4% 10 3.9% 0 Ia Ib IIa AJCC Stage IIb IIc Melanoma Lymphatic Mapping Preoperative Eligibility Primary tumor criteria > 1mm Breslow thickness < 1mm MR: present (Ib) Ulceration (Ib) Clark Level IV/V Vertical growth phase? Age? After a wide excision? Ambiguous diagnosis of melanocytic lesion? Pure Desmoplastic melanoma? National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology for Melanoma. V1.2010 Balch CM et al. J Clin Oncol. 2009;27(6):6199-6206. Who Should Undergo SLNB? National Comprehensive Cancer Network, 2011 Consider SLNB for high risk Ia melanoma Discuss and offer SLNB for stage Ib, stage II CM SLNB important staging tool, but impact on overall survival unclear AJCC Recommendations Microstaging of all primary melanomas Pathologic nodal staging for stage Ib-IIc National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology Melanoma. V. 3.2011 AJCC Cancer Staging Manual, Seventh Edition (2010) published by Springer Science and Business Media LLC, www.springerlink.com. SLN Biopsy Standard of Care? Discuss with patients: accuracy of SLN biopsy predicted risk for microscopic nodal disease potential risks and benefits how the information will impact therapy Currently offered as standard of care for patients with Ib-IIc and selectively for Ia. Thank You