EMP - University of Texas System
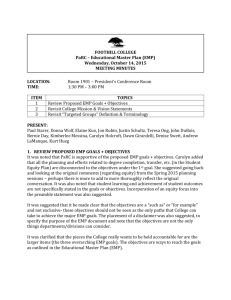
advertisement

ICU Adult Early Mobilization Program Egbert Pravinkumar, MD, FRCP Associate Professor Department of Critical Care UT MD Anderson Cancer Center Houston, Texas Presented on behalf of the ICU- EMP Task Force Objectives • • • • • • Overview Effects of immobility Benefits of early mobility Components of MDACC adult ICU-EMP Outcomes of our pilot program Future expansion of program Concept of Early Mobility • Phys Therap 1972 – Foss et al, Technique for augmenting ventilation during ambulation • CHEST1975 – Burns et al, use of special walker Early and Progressive Mobility • Early Mobility - Mobility program commenced even when patient participation is minimal or none • Progressive Mobility - Series of planned movement in a sequential manner Adverse Outcomes of Immobility Short-term • Ventilator associated pneumonia • Delayed weaning • Muscle de-conditioning/ weakness • Pressure ulcers Allen C, Lancet 1999 Morris PE, Crit Care Clin 2007 Adverse Outcomes of Immobility Long-term • Increased morbidity/ mortality • Decreased functional capacity • Dependency for ADL • Increased cost of care • Markedly impaired quality of life Herridge MS, NEJM 2003 Hopkins RO, Amer J Resp Crit Care Med 2005 Benefits of Early Mobility • • • • • • Improved outcome at 1yr post ICU Reduced delirium (ABCDE approach) Improved functional outcomes Decreased IMV days Decreased hospital days Decreased cost of care Morris PE, Am J Med Sci, 2011 Morandi A, Curr Opin Crit Care 2011 Schweickert WD, Lancet 2009 Established Standards vs. Practice • Only 3% of ICU patients were turned as per required standards • Only 50% had some change in body position • The average time between manual turns were 4.85±3.3 hr Krishnagopalan S, Crit Care Med 2002 Goldhill DR, Anaesthesia 2008 Barriers for Early Mobility • • • • • • • • Need for a culture change Perceived harm of mobilization Subjective variations in decisions Disagreement between care givers Lack of structured algorithm Excessive sedation Lack of knowledge of the benefits Lack of tools and trained staff Early Mobilization Program in Oncological ICU • Purpose: To develop, implement and evaluate an early mobilization program for adult ICU patients in a mixed medical and surgical oncology ICU. • Aim: To increase the average number of mobilization activities per patient day by 40% within an 8 week pilot period MDACC-Adult ICU EMP • Interdisciplinary team • Design of evidence based EMP algorithm • Pre-implementation – Data collection – Survey on knowledge and perceptions related to mobilization – Education • 8 week trial period from October 2010 through December 2010 - Medical & surgical patients (16/54 ICU beds) Our Interdisciplinary Team MDACC-Adult ICU EMP • Interdisciplinary team • Design of an evidence based EMP algorithm • Pre-implementation – Data collection – Survey on knowledge and perceptions related to mobilization – Education • 8 week trial period from October 2010 through December 2010 - Medical & surgical patients (16/54 ICU beds) EMP Algorithm Highlights • Contraindications • Precautions • Signs of intolerance • PT/OT consult within 24 hours of admission • 5 Levels based on RASS and functional status EMP: Contraindications ICP ≥ 15 RASS +4 Acute or Uncontrolled Intracranial Event Fio2 ≥ 0.85 on invasive mechanical ventilation PEEP ≥ 15 / VDR or HFOV Unsecured airway Active cardiac ischemia Uncontrolled arrhythmias Blood pressure instability despite vasopressors Unstable fracture EMP: Precautions Continuous dialysis VTE Lumbar drain External ventricular drain Plastic surgery Orthopedic surgery RASS +3 If precautions are present – discuss with team prior to initiating mobilization activity EMP: Signs of Intolerance RR > 40 Sp02 < 88% MAP < 50 or > 130 HR < 50 or > 130 Development of any contraindications Initial 5-Level EMP 5-Level Progressive EMP MDACC-Adult ICU EMP • Interdisciplinary team • Design of evidence based EMP algorithm • Pre-implementation – Data collection – Survey on knowledge and perceptions related to mobilization – Education • 8 week trial period from October 2010 through December 2010 - Medical & surgical patients (16/54 ICU beds) Data Collection Tool Survey: Pre-Implementation of EMP • Need for a standardized process • Need for facilitator and mobility team • Variations in MD practices • Concern over tube and line integrity • Head/Neck & Plastic surgery patients • Lack of personnel/equipment • Lack of knowledge and skill MDACC-Adult ICU EMP • Interdisciplinary team • Design of evidence based EMP algorithm • Pre-implementation – Data collection – Survey on knowledge and perceptions related to mobilization – Education • 8 week trial period from October 2010 through December 2010 - Medical & surgical patients (16/54 ICU beds) Data for Pilot Program • Total mobilization activities • Average mobilization activities/pt. day • OT/PT activity Total and Average ICU Mobilization Activities Average Mobilization Activities per Patient Day Total Mobilization Activities 18 650 16 550 14 450 12 350 Pre-Protocol 10 Pre-Protocol 2-week 2-week 4-week 250 4-week 8 8-week 8-week 6 150 4 2 50 Nursing -50 PT OT 0 Nursing PT OT Activities included: ROM, positioning, bed in chair position, splinting, dangle at the edge of bed, out of bed, ADL, and ambulation. Data Summary: PT/OT Consults Total number of visits in Pods C & D (Sep. ’10 & Dec. ‘10) PT/OT Consults and Treatments Number of Visits 250 200 150 Pod C & D 100 All Pods 50 0 Sep PT Sep OT Dec PT PT/OT Dec OT Mobilization Activities Pre and Post EMP Mobilization activities* per patient day during pre-protocol period and at 8 weeks: • Nursing: increased by 31% • Occupational Therapy: increased by 86% • Physical Therapy: increased by 78% *Mobilization activities include: bed in chair position, dangle EOB, OOB, ADL and ambulation Pilot Data Summary • Aim: To increase the average number of mobilization activities per patient day by 40% within an 8 week pilot period 47% Potential Cost Savings • Based on reduction in ICU-LOS by 1 day Non-ventilated patients [$3,872/day x 136 pts/month] = $526,592/month Ventilated patients [$7105/day x 83 pts/month] = $589,715/month EMP: Beyond the Pilot Program Simplified 3-Level EMP Highlight of Changes • Condensed to 3 Levels • Reduced contents of levels • Incorporation of visual cues Simplified 3-Level EMP Sustainability and Expansion of EMP Number of visits • Feb 1, 2011 - Expanded program to 34/54 ICU beds • May 1, 2011 - Expanded program to 54/54 ICU beds Staffing and Education • Addition of 2 FT physiotherapist • Addition of 1FT occupational therapist • On-going targeted education strategies Visual Cues - Door Signs & Communication Signs Visual Cues - Room Signs EMP Research and Publication • Abstract accepted in 2012 SCCM congress • Abstract submitted to 2012 Canadian Respiratory Congress • Oral and poster presentation in Texas and American OT Association • Oral presentation in Texas PT Association • IRB proposal for prospective outcome trial Special Thanks • Mary Lou Warren, RN, CNS-CC • Shari Frankel, PT, MBA, ATC • Stacy Ryan, PT, DPT, APC • Vi Nguyen, MOT, OTR, RRT • Becky Garcia, RN, BSN • Mini Thomas, RN, CCN • Laura Withers, MBA, RRT • Quan Nguyen, RRT • Ninotchka Brydges, MSN, ACNP-BC Thanks to Leadership of Nursing, Critical Care and Rehabilitation Services Funding provided by Volunteer Endowment for Patient Support (VEPS) Thank you Richmond Agitation Sedation Scale Future Trend System-Specific Effects of Immobility • • • • • • • Psychosocial impairment VAP/HCAP, Atelectasis, FVC Reduced CO, autonomic dysfunction Decubitus ulcers, wound healing Critical illness myopathy/ Mm. atrophy Deep vein thrombosis Insulin resistance Greenleaf JE, Exerc Sport Sci Rev 1982 Steven RD, Int Care Med 2007 Hamburg NM, Arterioscler Thromb Vasc Biol 2007, Truong AD, Crit Care 2009 Safety of EMP in Critically Ill • • • • • • Schweikert WD, Lancet 2009;373:1874 Morris PE, Crit Care Med 2008;36:2238 Bailey P, Crit Care Med 2007;35:139 Burtin C, Crit Care Med 2009;37:2499 Thomsen GE, Crit Care Med 2008;36:1119 Stiller K, Physiother Theory Pract 2003;19:239 EMP: Initial Process Orders are written: Early Mobilization Protocol: PT/OT consult & treat RN 1. Assess patient upon admission 2. Begin nursing interventions based on level 4. Delegate activities to nursing assistant PT/OT 1. Examine patient within 48 hours 2. Reinforce teaching and nursing interventions 3. Develop and implement PT/OT plan based on examination and Mobility Level 5. Update mobility levels & motivational tokens in room