Cushing's - WordPress.com
advertisement

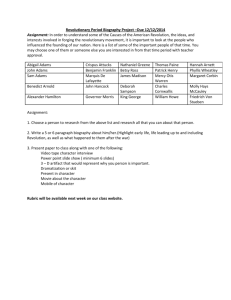
AC Station Week 4- Room #1 S-Situation Pt name: David Adams, 45 year old male Admitted under the care of Dr. Jones Room 352, Med-Surg Unit, Tech General Hospital Current time: 0745 B-Background Admission Diagnosis: Unexplained weight gain, hypertension, muscle weakness. Past Medical History: chronic back pain, kidney stones. Home Medications: Norco 7.5/500 q 6hours PRN pain. Allergies: Demerol Height: 6’2” Weight: 242lb 110kg Date of birth: 04-10-1968 Code Status: Full Code A-Assessment Mr. Adams is a 45 year old man who has been admitted from his physician’s office for a work up related to unexplained weight gain, hypertension, and mood changes. He is also complaining of muscle loss, weakness, and insomnia, increased thirst and increased urination. The patient lives with his wife and is on medical disability because of a previous back injury. Mr. Adams is now resting in bed after returning from a MRI a few hours ago and has had lab work done this morning (CBC, CMP with electrolytes, 24 hour urine cortisol, and a plasma ACTH level. A Dexamethasone suppression test is pending). He complains of back pain 4/10. Mr. Adams has a peripheral IV in his left AC with LR at a rate of 120 ml/hr. BP: 168/95 HR: 80 RR: 16 O2 Sat: 96% on room air, Temp: 98.90F R-Recommendation Complete an assessment, review labs, MD orders, and MAR. Inform faculty member of suspected diagnosis, then develop basic concept map linking assessment findings, labs, and orders. The MRI report shows a pituitary tumor and a transsphenoidal resection has been scheduled for tomorrow morning @ 0700. AC Station Week 4- Room #1 Physician’s Orders Patient ID Name: David Adams DOB: 04/10/1968 MRN: 111-22-333 ALLERGY: Demerol Date: Today 1. Admit to Medical/Surgical Unit under the care of Dr. Jones 2. Diagnosis: Cushing’s disease secondary to a pituitary tumor. 3. Allergies: Demerol 4. Code Status: Full 5. VS: Q 4 hours, weigh daily in am. 6. oxygen therapy to keep 02 sat > 96% 7. Diet: NPO except for medications pending transsphenoidal resection @ 0700 tomorrow. 8. Strict I&O’s, collect all urine for 24 hours stop @0700 and send to lab. 9. Activity: as tolerated 10. AM Labs: CBC, CMP with electrolytes, Plasma ACTH level, Plasma Cortisol level, and pituitary MRI-done. 11. Dexamethasone Suppression test lab draw at 0800 12. Medications: 13. Zestril (lisinopril) 10 mg PO once daily @0800 for treatment of high blood pressure. 15. Norco 7.5mg/500mg one to two tablets PO q 6 hours PRN pain. 16. Ambien (zolpidem) 10 mg PO q HS for treatment of insomnia. 17. LR at a rate of 120 ml/hr 18. 19. 20. AC Station Week 4- Room #1 Name: David Adams DOB: 04/10/1968 MRN: 111-22-333 ALLERGY: Demerol CBC WBC: RBC: HGB: HCT: PLT: Reticulocyte Count: Result 3 Sodium Potassium Cl Carbon Dioxide Glucose BUN Creatinine GFR Calcium Total Protein Albumin Total Bilirubin Alkaline Phosphatase ALT AST Result 140 mmol/L 3.1 mmol/L 104 meq/L 22 mmol/L 142 mg/dL 18 mg/dL 1.0 mg/dL 82 ml/min/1.73mm 10 mg/dL 7.0 g/dL 4.2 gm/dL 1.3 mg/dL 130 IU/L 48 IU/L 45IU/L Lipid Panel Total Cholesterol HDL LDL VDL 5.0-10.0 mm3 4.5 – 6.0/uL 13- 17 g/dL 40- 50 % 150- 400 K/uL 12.5 mm 5.18 m/UL 15g/DL 45 % 178 K/uL 0.3% CMP Reference Range Reference Range 136-145 mEq/L 3.5-5.0 mEq/L 98-106 mEq/L 23-30 mEq-L 70-110 mg/dL 10-20 mg/dL 0.6-1.2 mg/dL 62-120 ml/min/1.73mm 8.2-10.2 mg/dL 6.3-8.0 gm/dL 3.5-5.5 gm/dL 0.2- 1.3 mg/dL 38-126 IU/L 9-52 IU/L 14-46 IU/L Result Reference Range 220 mg/dL 45 mg/dL 140mg/dL 40 mg/dL Less than 200 mg/dL M :>45 mg/dL F:>55 mg/dL Less than 130 mg/dL 7-32 mg/dL 45 mcg/dl Pending 6-21 mcg/dl <1.8mcg/dl 350 mcg/24hr 98pg/ml 10-100 mcg/24hr <80pg/ml in am, <50pg/ml in pm Add-on Lab Plasma Cortisol Dexamethasone Suppression test 24 hour urine cortisol Plasma ACTH Lab Results: Date: Today Time: 0400 AC Station Week 4- Room #1 Tech General Hospital 24 HOUR MEDICATION ADMINISTRATION RECORD Order Date today today today DC Date Treatment and Frequency LR @ 120 ml/hr IV Due Time 0700-1900 1900-0659 0700-1900 1900-0700 Cont. Zestril(lisinopril) 10 mg PO daily @0800 for treatment of hypertension Ambien(zolpidem) 10 mg PO @ HS for treatment of insomnia. today today today today PRN meds today Norco(hydrocodone), one to two tablets PO q 6 hrs, PRN pain. today today today today Initial that MAR has been Verified/Reconciled: Initial Signature Initial Signature Patient I.D. Name: David Adams DOB: 04/10/1968 MRN: 111-22-333 ALLERGY: Demerol AC Station Week 4- Room #1 Mr. David Adams (Cushing’s disease) Assessment: VS: 168/ 95 HR: 80 RR: 16 O2 Sat: 96% on room air. Temp: 98.90F Pain: 4/10 Back pain unrelieved by position changes. Head: PERRLA @ 4 mm, GCS 15, AOx3. Patient has a notably rounded face (moon face) with red cheeks (plethora). Patient is emotionally labile. Neck: Excess adipose tissue on back of neck (buffalo hump). Chest: truncal obesity noted. Cardiovascular: S1, S2 present, regular rate and rhythm. Blood pressure elevated at 168/95. Abdominal: Pendulous abdomen with active bowel sounds in all four quadrants. Last known BM was yesterday. GU: Voids without pain; Last void was early this morning – slightly cloudy, amber, and no odor. UA shows glycosuria and hypercalciuria. Skin: The patient has thin, fragile skin with areas of purple striae over the abdomen. Areas of bruising noted on extremities. MS: Muscle wasting is noted in the extremities, patient complains of back pain, fatigue, weakness and has an awkward gait. **Suggested lab to help students if they are struggling: 24 hour urine collection, Dexamethasone suppression test, plasma cortisol, K+, UA, CT of pituitary gland.