Ground rules for the class
advertisement

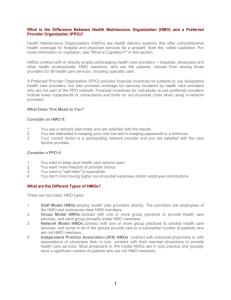
“Managed Care” Introduction to Health Policy HMS Fall 2000 Nancy Turnbull, HSPH Ground rules for the class • No idealizing the “unmanaged” health care system • Differentiate among – Managed care techniques – Managed care organizations (MCOs) – Competition among MCOs (“managed competition”) • “If you’ve seen one MCO, you’ve seen one MCO” • The plural of anecdote is not data • MCOs did not introduce the profit motive into medicine • The status quo has many constituencies “Problems in health care quality are serious and extensive...Americans bear a great burden of harm because of these problems, a burden that is measured in lost lives, reduced functioning and wasted resources… Collectively, these problems call for urgent action … Quality of care is the problem, not managed care....” Institute of Medicine, September, 1998 Variation: CABG/1000 (Medicare) Dartmouth Atlas, 1996 What is managed care? • “Anything other than an arrangement in which the insurer pays all bills without questions.” – Mark Pauly • “A term that has even less specificity than the label ‘low in fat’ in your super creamy dessert.” – Harold Luft • “A vague phrase that covers actions that range from the euphemistic to the evangelistic.” – Daniel Fox Techniques of managing care • • • • Selective contracting with providers Financial incentives for providers Financial incentives for patients Medical management/quality improvement techniques – – – – – “Gatekeepers” Precertification Referral authorization Case management Demand management -Organizational culture -Practice guidelines -Provider profiling -Disease management -Drug formularies Types of entities that can adopt managed care techniques • • • • • HMOs Insurance companies Employers Unions/welfare plans Medical management firms (full-service or specialty) • • • • • Individual providers Delivery systems Medicare Medicaid programs National health systems Common characteristics of managed care organizations • Combine financing and delivery of care (a “system”) • Enrolled population (“members”) • Prepaid premium (a “fixed budget”) • Selective “network” of providers • Requirements and/or incentives to use providers in the network • Focus on prevention and primary care • Medical management and quality improvement programs Types of Managed Care Organizations • • • • Health Maintenance Organization (HMO) Preferred Provider Organization (PPO) Point of Service (POS) Plan Managed Indemnity Plan • Comprehensive vs. single service – Mental health, prescription drug The HMO (Health Maintenance Organization) • Organized health system responsible for a. financing b. delivery • of comprehensive health services • with restricted choice of providers • to an enrolled population • for a prepaid, fixed fee The Original Types of HMOs • • • • Staff model Group model Network model Independent practice association (IPA) model • Direct contract model The creation of a mixed model MCO: Harvard Pilgrim Health Care • Harvard Community Health Plan-staff model HMO founded in early 1970s • Merged with Multigroup, a group model, in 1988 • Merged with Pilgrim, direct contract model HMO, in 1994 • Formed an insurance company in 1995 • Spun off health centers (staff model) to form Harvard Vanguard Medical Associates in 1997 • Acquired Neighborhood Health Plan, network model HMO, in 1998 • Bought half of Health New England, an IPA HMO, in 1998 The PPO (Preferred Provider Organization) • An organization that contracts with employers or insurance companies to provide health care from a selected group of providers (“preferred providers”) • Distinguishing characteristic from an HMO: – Consumers may use non-preferred providers but must pay more out-of-pocket Key PPO Characteristics • Select provider network • Negotiated rates of payment • Incentives in benefit structure for consumers to use preferred providers • (More or less) Utilization management and quality improvement programs POS (Point of Service) HMO Plan • Hybrid HMO product that is similar to a PPO – Member may use non-HMO providers but must pay higher out-of-pocket costs • Fastest growing segment of managed care • Broader choice of provider than HMO • (Potentially) greater ability to control costs and utilization than a PPO Managed Indemnity Plan • Traditional insurance plan that adopts some features of managed care – Most common examples • Prior authorization of hospital admissions • Catastrophic case management • Specialty utilization management of certain services (e.g., mental health, pharmacy) • Freedom of choice of providers • More limited ability to control costs Average annual change in employer health benefit cost: 1987-1999 20.0% 15.0% 10.0% 5.0% 0.0% 87 88 89 90 91 92 93 94 95 96 97 98 99 -5.0% % annual change Employer techniques to control costs • Increased cost-sharing with employees – Premiums – Deductibles, coinsurance, copayments – Defined contributions not defined benefits • Benefit cutbacks • Eligibility reductions • Managed care plans US Managed Care Penetration: 1993 vs. 1998 1 0.9 0.8 0.7 0.6 0.5 0.4 0.3 0.2 0.1 0 91% 52% 52% 1993 1998 16% 9% Employed Medicare 14% Medicaid 19 Change in percentage of workers in various types of health plans: US 1993, 1996-1998 60 50 48 35 36 40 30 20 10 27 23 30 30 25 27 31 19 20 19 15 9 7 0 Traditional HMO POS PPO 1993 1996 1997 1998 Growth of products with “choice” • Majority of managed care enrollment is in PPO and Point of Service products • Consumers equate “choice” with quality • MCOs want broadest provider networks for marketing reasons – Managed care plans have diffuse and largely overlapping provider networks – Most providers do not distinguish among MCOs in delivering care 21 Potential strengths of managed care • Containing the increase in health care costs • Improving quality – – – – – – Creating more rational systems of care Improving coordination of care Enhancing communication among providers Reducing variation in practice Improving access Promoting prevention and wellness • Enhancing accountability Potential concerns about managed care • • • • • • • Impaired continuity of care Withholding of necessary care Failure to provide “state of the art” care Increased administrative costs Reduced clinical autonomy Hindering provider advocacy for patients Promoting competition based on risk selection and not efficiency of providing care Managed care is still an experiment • Limited research on results of managed care • Results seem to suggest: – Lower rates of hospitalization – Less intensive use of some resources – Clinical quality measures as good, sometimes better (not clear for frail and poor) – Satisfaction higher for costs, paperwork – Satisfaction lower for access; lower for the poor and frail elders – Lower “costs” (at least until last two years) Past results may not be predictive of future • Limited number of HMOs studied; mostly staff and group • Focus on traditional, lock-in products • Inadequate correction for selection bias • Comparison usually of HMOs to unmanaged, indemnity plans • Focus on “does MC work” rather than “what in MC works” Little evidence that MCOs have achieved sustainable reductions in the rate of increase in costs • Some scattered victories, but battle continues • Premiums are not costs – MCO pricing decisions – Cost-shifting • By purchasers to covered individuals and by dropping coverage • Among purchasers • To families (e.g., home health) – Benefit differences – Administrative costs not adequately included – Risk selection – Differences in different market segments (e.g., small group, nongroup) Managed care has not altered most of the causes of rising costs • • • • • • Technology Demographics Mix of primary and specialty physicians Excess capacity Lack of universal coverage Culture (“death is optional”) The Possibilities of Managed Care 1. Manage Cost • Manage insurance risk: benefit package design, pricing, marketing • Manage provider pricing: network formation, contracting • Manage utilization: utilization review, provider financial incentives, consumer cost-sharing The Possibilities of Managed Care 2. Manage Care • Develop and implement protocols for prevention and treatment; monitor outcomes • In-hospital acute case management / “care pathways” • Disease management across continuum of care; shift resources from acute to chronic, inpatient to community-based sites of care The Possibilities of Managed Care 3. Manage Health • Population-based interventions – – – – Risk assessment Outreach Intervention Monitoring and follow-up • Shift resources from health sector to non-health sector (education, social services, housing, transportation) Why the growing scrutiny and public discontent with managed care? • Managed care is not a “voluntary” choice for most people • No more “safety valve” of unmanaged care • Middle class has shifted debate from coverage and affordability to allocation • Massive transfer of power from providers to purchasers • “As the pie shrinks, the table manners deteriorate” • Impingement on autonomy of providers • Complexity and administrative hassle Why the growing scrutiny and public discontent with managed care? (cont’d) • Growth of for-profit plans/distrust of “Wall Street” • Some true horror stories (although these existed in unmanaged care as well) • Managed care introduces a more obviously “accountable” entity • Managed care doing the “dirty work” of cost containment and resource allocation • Consumers have not benefited from the cost savings of managed care “Hot” regulatory issues • Access to care – Any willing provider laws – Access to emergency treatment/standards to judge what is an “emergency” – Use of specialists as “gatekeepers” – Continuity of care following enrollment and provider termination • Quality of care – Standards for utilization management decisions – Standards for specific diagnoses/conditions – Collection and reporting of access and quality information An Act to protect patient continuity of care A health plan that requires the designation of a primary care physician shall notify a member at least 60 days prior to the disenrollment of such member’s PCP and shall permit such member to continue to be covered for covered health services by such physician at least six months after said physician is disenrolled, unless the physician is disenrolled for quality reasons …A member in her third trimester of pregnancy may continue treatment with said provider until after her first postpartum visit…A member who is terminally ill (meaning an illness which is likely, within a reasonable degree of medical certainty to cause death within one year), may continue treatment with said provider until the member’s death.” Pharmacy Freedom of Choice “An HMO must contract with any pharmacy willing to accept the terms and conditions of the HMO’s provider contract, including reasonable credentialing criteria, rates of payment, utilization management, and quality assurance requirements.” Minimum Maternity Length of Stay Any HMO shall provide coverage of a minimum of 48 hours of inpatient care following a vaginal delivery and a minimum of 96 hours following a cesarean section. Any decisions to shorten these minimum coverages shall be made by the attending physician in consultation with the mother. Coverage in the event of an early discharge shall include necessary home visits, patient education, and any appropriate tests. “Hot” regulatory issues (cont’d) • Due process protections – Grievance and complaint procedures – Right of appeal to independent entity – Provider due rights and process • Access to prescription drugs not on formulary • Ability to sue MCOs for medical malpractice • Provider payment and financial incentives – prohibition against individual capitation – mandatory stop-loss protections – need for risk adjusted payment “Hot” regulatory issues (cont’d) • Regulation of providers assuming financial risk and providers contracting directly with purchasers • Privacy of of patient medical information • Minimum Medical Loss Ratios/”Care Share” • Disclosure to consumers – – – – Provider payment methods Provider networks Medical necessity and medical management criteria Quality report cards Minimum Medical Loss Ratio “An HMO must spend at least 90% of annual earned premium on medical expenses. Any HMO failing to meet this standard shall refund to its policyholders any amount by which its medical loss ratio failed to meet this standard, either by actual refunds or by offsets against future premiums.” An Act to protect the privacy of mental health information “No health plan shall require consent by a member to the disclosure of information, other than the patient name, diagnosis and date and type of service, as a condition to receiving mental health and substance abuse benefits….No health plan shall acquire or disclose any communications by a member to a psychotherapist arising out of the diagnosis or treatment of a mental condition without the express and informed written consent of the member, and such informed consent shall include notification of the right not to give such consent.” What should health professionals do to help realize the possibilities of managed care? Work to change the US financing system – – – – – – Universal coverage Sharing the financing burden equitably Publicly accountable health planning processes Societal affordability (e.g., budgets) Controls as close to caregivers as possible Put savings from managed care into systems to expand coverage and improve health