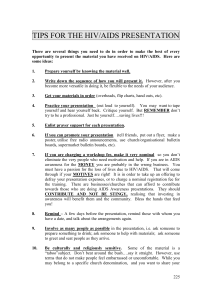
Case Study on the Integration of HIV/AIDS Services
advertisement

LESSONS LEARNT FROM THE CASE STUDIES ON INTEGRATED HEALTH SERVICES DELIVERY NETWORKS AND VERTICAL PROGRAMMES Edwin Vicente C. Bolastig, MD, MSc Consultant, PAHO/WHO 14th September 2010 Rovanel’s Resort, Tobago 2 Presentations: • Case Study on the Integration of HIV/AIDS Services in Trinidad and Tobago into Maternal, Newborn & Child Health Services, as well as Sexual and Reproductive Health Services, including Family Planning (focused on Tobago findings) • Experiences and Lessons Learned from Case Studies in the Region of the Americas 2 Case Study on the Integration of HIV/AIDS Services in Trinidad and Tobago into Maternal, Newborn & Child Health Services, as well as Sexual and Reproductive Health Services, including Family Planning Edwin Bolastig, Yoko Laurence and Karen Pierre Funded by: Pan American Health Organization/ World Health Organization OBJECTIVES OF CASE STUDY • To contribute to the body of work on health services integration • To determine: “how vertical programs and Global Health Initiatives have impacted on the health system, and affected segmentation/fragmentation” 4 TRINIDAD AND TOBAGO: • • • • • • • • Southernmost Caribbean country Independence 1962; Republic 1976 Parliamentary democracy Multi-ethnic population: 1.3M Oil and gas-based economy GNI per capita (09):US$ 17,884 10-year GDP growth(99-08): 7.7% Epidemiologic shift: CNCDs over 60% of deaths 5 CONTEXT • First HIV case diagnosed in 1983 • 8th leading cause of death in 2004 • STI-HIV co-infection prevalence rate: 42% (60% M ; 40% F) (Buensuceso, 2008) • HIV/AIDS cause enjoys strong political support • World Bank loan, EU grant, CARICOM PANCAP, government, private sector funding SOCIAL DRIVERS: • Poverty and unemployment • Gender inequality/domestic violence • High mobility: Caribbean diaspora • Stigma and discrimination • Multiple sex partners/Early initiation • Substance abuse/unprotected sex (UNAIDS , 2005) ECONOMIC DRIVERS: • Inequitable income distribution • Sex work due to poverty • Rapid urbanisation • Limited skills and poor socialisation • Sex-oriented tourism (Camara, CAREC, 2002) 6 BROAD SECTORAL CONTEXT • 1986 – National AIDS Programme • 1993 – Caribbean Charter on Health Promotion • 1996 – Health Sector Reform Programme (HSRP) National Health Promotion Plan • 2001 – Health Promotion Council; Directorate of Health Promotion and Public Health • 2004 – National AIDS Coordinating Committee (NACC) • 2005 – Vision 2020 • 2006 – MOH Corporate Plan (2006-2009) 7 SEGMENTATION/FRAGMENTATION • Decentralisation of health service delivery to RHAs with the exception of Vertical Programmes and Services • Fragmented human resource management • Dual employment system • Information and medical records management largely manual • Unstructured referral system 8 HIV INTEGRATION INITIATIVES • Integration with Maternal and Child Health PMTCT • Integration with STI and Family Planning - VCT • Integration with Population Programme - PITC • Integration with Chronic Disease Care – Tobago Health Promotion Clinic (THPC) • Integration of Treatment with Prevention – San Fernando General Hospital • Integration of Information Systems for HIV/AIDS – TERIDA Project 9 Description of the Process of Integration of HIV/AIDS services in Trinidad and Tobago using PAHO’s Framework on Integrated Health Services Delivery Networks (IHSDN) 10 1. The covered population/territory is defined and there is broad knowledge of its health needs and preferences, which determine the services provided by the system. • HIV Prevalence: 1.5% of Population (generalised epidemic) • Perception that high-risk groups are welldefined but targeted prevention not happening • In Tobago, youths targeted but not MSM or sex workers 11 2. An extensive offer of health facilities and services, which include public health services, health promotion, disease prevention, timely diagnosis and treatment, rehabilitation, and palliative care, all under a single organizational umbrella. • Tobago Health Promotion Clinic (THPC) – Dr Noel – behaviour modification, social services, housing, religious/pastoral services, mental health, substance abuse, mobile services, nutrition, dental referral, etc. 12 3. A first level of care that acts as the de facto gateway to the system, integrates and coordinates health care, and meets most of the population’s health needs. • Tobago Health Promotion Clinic (THPC) is the gateway into the system 13 4. Specialist services delivered in the most appropriate place, preferably non-hospital settings. • Pregnant women referred to THPC • Baby treated at paediatric ward in TRH • One (1) HIV specialist in Tobago for adults but none for paediatric care 14 5. Coordination of care mechanisms exist throughout the entire continuum of services. • A full and integrated coordination of care mechanism is compromised due to: – A lack of feedback to and from TPHC – Ineffective utilisation and training of personnel within organisations. 15 6. Health care centered on the person, the family, and the community/territory. • Health professionals from the health centres and THPC sometimes go out to the community to do testing via the Mobile Clinics at football games or all-fours clubs. • THPC has a programme that provides support to discordant couples, allowing these couples to have children who eventually turn out to be negative • No prevention programme for at risk families 16 7. A single, participatory governance system for the entire IDS. • National Strategic Plan for HIV/AIDS is monitored by the NACC under the Office of the Prime Minister), while implementation of the Health Sector Plan is monitored by the Ministry of Health through HACU. • In Tobago, THPC falls under the Tobago House of Assembly (THA); Tobago HIV/AIDS Coordinating Committee (THACC) serves as the link between NACC and THA 17 8. Integrated management of administrative and clinical support systems. • Disparate administrative and clinical support systems are not managed in an integrated manner • At THPC, administrative and clinical support addressed by some administrative staff but everyone working at clinic can provide support services if necessary 18 9. Sufficient, competent human resources, committed to the system. • Human resources for the THPC are considered insufficient given the comprehensive nature of the clinic in terms of HIV and chronic disease treatment, which has caused the clinic to grow continuously since its inception. • Only 16 of required staff of 27 19 10. An integrated information system that links all members of the IDS. Trinidad & Tobago HIV/AIDS Web-based Information System Figure 1: TERIDA – IT System Diagram · · · · · Expansion to other Stakeholders: Tobago GH & clinics Mt. Hope Pediatric ward PoSGH clinics Sangre Grande GH Others MRF (Medical Research Foundation) HIV/AIDS Ward, SFGH Cellma (CMS) Cellma (CMS) QPCC&C North Cellma (CMS) NACC Health Metrics 3D (BI) Internet QPCC&C South Cellma (CMS) • Tobago not included in pilot project TPHL M/Lab IT Dept MoH NBTS Blade Server Health Exchange Platform Blood Bank e-Progresa · · · NSU Health Metrics 3D (BI) Forsys (PHR-EMR) X4H Oracle DB Application Software · · · · · · · Cellma: Clinical Management System (CMS) M/LAB: Laboratory Information System HM3D: Business Intelligence suite (BI) Forsys: Patient Health Records (PHR) E-Progresa: Blood bank management System Health Exchange Integration Platform Hub X4H: Expert System for Health 20 11. Adequate financing and financial incentives aligned with the goals of the system. • 2 schools of thought in terms of adequacy of financing: – There is enough funding for HIV/AIDS, the problem is effective utilization and despite huge investments, there is no reduction of HIV in the general population. – Financing could never be enough: as progress is made in diagnosis and treatment, new techniques, equipment and drugs emerge in the market. 21 12. Broad intersectoral action. • Collaboration between THPC and support groups like TAS, OASIS and others • THACC is known for engaging the community through the village councils in the implementation of HIV-related projects. • Corporate sponsorships but discrimination happens in the workplace 22 EMERGING MODELS Three (3) Emerging Models of Integration: 1. Standalone outpatient HIV/AIDS clinic integrated with chronic disease care (Tobago Health Promotion Clinic) 2. Hospital-based HIV/AIDS testing and treatment centres – adult & paediatric (San Fernando General Hospital) 3. Satellite network of multi-tiered hospital based and outpatient health facilities 23 MODEL 1 – Stand Alone ADVANTAGES/STRENGTHS •By associating HIV/AIDS with other chronic diseases, stigma and discrimination may be minimised •Unique branding strategy associating comprehensive approach with quality care •Well-organised manual record-keeping transitioning to a paperless information system •Multi-tasking of health workers •Triaging according to purpose of visit (counselling and testing, pick-up of ARVs, consults, etc.) to avoid long queues and waiting times •Community outreach activities (home visits) ensures good follow-up/ return rates GAPS/WEAKNESSES •Weak linkage with health centres doing counselling and testing •Referrals have to be made to the Scarborough General Hospital for treatment of paediatric patients and to the OB/GYN Ward for pregnant women •Inconspicuous location – not all potential clients are aware of the clinic site (Conversely, could be an advantage too) 24 MODEL 2 – Hospital Based Testing and Treatment ADVANTAGES/STRENGTHS •Simulates “one-stop shop” for services (STI, HIV/AIDS testing, counselling and treatment, maternal and child care, etc.) in a single health facility/ compound GAPS/WEAKNESSES •Weak community outreach services •Link to family planning services missing •Hospital-based care is known to be generally more expensive than outpatient care 25 MODEL 3 – Multi-tiered Satellite Network ADVANTAGES/STRENGTHS •“Hand-holding” approach to referral of patients to other health facilities •Assurance of a wide range of services •Relatively good feedback being received from facilities where patients were referred to GAPS/WEAKNESSES •Patients being lost in the process of referring to another health facility •Patients being lost to follow-up •Longer time spent in securing appointments and attending clinics •Travel and opportunity costs of attending multiple clinic schedules 26 FINANCING – Total TTD 253.5 million 1 USD = 6.29 TTD 27 BENEFITS 1. Programmes – institutionalisation of PMTCT; integration of VCT with SRH; free ARVs 2. Resources - high levels of funding for HIV/AIDS also used for MCH, STIs and FP 3. Processes - shift from a programme approach to institutionalisation of interventions 4. Intermediate products – build capacity of committed health personnel 5. Outcomes – increased HIV testing among mothers; improved efficiency in some areas; community outreach 28 TWO SCHOOLS OF THOUGHT ON INTEGRATION: Strengthening of services as pre-requisite to integration vs. Integration as means to improve services 29 LESSONS LEARNT Facilitating factors: • Role of advocates and champions in the health system • Perception of strong political support from government • Health promotion (high risk groups and wider population) • Service delivery decentralisation (RHAs) • Increased resources for HIV/AIDS • Expanded role of civil society – “knowledge broker” 30 LESSONS LEARNT Hindering Factors: • Structural and support services – inadequate infrastructure, human resource shortages, weak reporting and referral systems • Socio-cultural – breach of confidentiality, S&D, territorialism, lack of accountability • Policy and legal environment – lacks policy framework for zero tolerance to S&D, non-adherence to protocols/SOPs 31 AREAS FOR IMPROVEMENT 1. 2. 3. 4. 5. Socio-cultural Health workforce Service delivery Systems interventions Policy and legal environment 32 CONCLUSIONS • Resources for HIV/AIDS supported integration of HIV services with other health programmes such as Maternal and Child Health • GHIs did not seem to have undermined national planning and policy development process • Integration process aligned with national priorities, along existing mechanisms for coordination 33 Experiences and Lessons Learned in the Region of the Americas: Case Studies Regional Advisory Meeting: Integrated Health Services Networks and Vertical Programs Cusco, Peru 11 and 12 November 2009 Hernán Montenegro and Caroline Ramagem Area of Health Systems and Services PAHO/WHO Integration Initiatives in LAC Country Initiative Argentina Law creating the Integrated Federal Health System Bolivia Municipal Intercultural Family and Community Health Networks and Network of Services Brazil Better Health: The Right of All 2008-2011 Chile Health Care Networks Based on Primary Care El Salvador Law creating the National Health System Guatemala Coordinated Health Care Model Mexico Functional Integration of the Health System Peru Guidelines for forming networks Dominican Republic Regional Health Services Network Model Trinidad and Tobago Experience of the Eastern Regional Health Authority Uruguay Integrated National Health System Venezuela Health Network of the Metropolitan District of Caracas Summary of Case Studies Lima Workshop, 9 November 2009 Country Type of Case Integrated health services networks Integration of vertical programs (6) (2 topical + 3 general = 5) Brazil • Care for women and children: “Mãe • HIV/AIDS (National) Curitibana” (Curitiba, Paraná) • Urgent/emergency care (Northern Macroregion, Minas Gerais) Chile Guatemala • Ñuble Health Service • Metropolitan Health Services • Children: “Chile Grows With You” (National) • Ministry of Public Health and Social Welfare and Guatemalan Social Security Institute (Department of Escuintla) Colombia • Tuberculosis (National) Peru • HIV/AIDS (National) Dominican Republic • HIV/AIDS (National) Trinidad and Tobago • HIV/AIDS (National) FACILITATING FACTORS AND BARRIERS 37 FACILITATING FACTORS • Political commitment and backing • Availability of financial resources • Leadership of health authorities and service managers • Decentralization and flexibility of local management • Alignment of financial and non-financial incentives • Culture of collaboration and teamwork • Active participation of stakeholders 38 STRUCTURAL BARRIERS • Segmentation and weakness of health systems • Reforms of the 1980s and 1990s: – Privatization of insurance – Differentiated service portfolios – Provider competition – Diversification and instability of labor regimes – Regressive cost-recovery schemes 39 STRUCTURAL BARRIERS • Powerful opposing Interest groups: – Specialists and super-specialists – Private insurers and social security – Pharmaceutical industry, supply industry, etc. • External financing modalities (Global Health Initiatives) 40 NON-STRUCTURAL BARRIERS • Deficiencies in information, monitoring, and evaluation systems • Management weaknesses 41 • Thank you! 43