Better Health, Better Care, and Cost Savings Through Improvement
advertisement

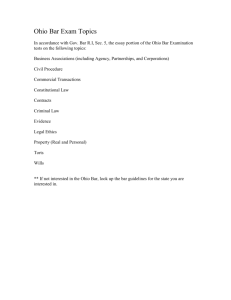
Better Health, Better Care, and Cost Savings Through Improvement Greg Moody greg.moody@governor.ohio.gov The Center for Community Solutions March 24, 2011 Medicaid is Ohio’s Largest Health Payer • Provides health coverage for low-income children, parents, seniors, and people with disabilities • Covers 2.2 million Ohioans (1 in 5) including 2 in 5 births1 • Spends $18+ billion annually all agencies, all funds (SFY 2011) 1 • Accounts for 4.0% of Ohio’s total economy and is growing2 • Funds are federal (63.69%) and state (36.31%)3 SOURCES: (1) Ohio Department of Job and Family Services, (2) SFY 2011 estimate based on $18.0 billion in Medicaid spending per ODJFS and $498 billion Ohio gross domestic product per the State of Ohio Office of Budget and Management, and (3) Federal Register Vol. 76 No. 22 page 5811. Ohioans Covered by Employer-Sponsored Health Insurance, Medicaid, or Uninsured 70% 60% 63.9% EmployerSponsored 57.4% Insurance 17.0% 18.8% 8.5% 9.8% 11.4% Medicaid 2009 2010 2011 66.3% 50% 40% 30% 20% 15.0% 10% 0% -10% Uninsured Source: Ohio Colleges of Medicine Government Resource Center, “Quantifying the Impact of the Recent Recession on Ohioans: preliminary findings from the 2010 Ohio Family Health Survey” (February 16, 2011) Federal Health Care Reform: Government Coverage Expansions 500% Federal Poverty Level Private Insurance $89,400 for a family of 4 400% Health Benefit Exchange 400% 300% 200% 100% $30,843 for a family of 4 Medicaid Medicaid Expansion Medicaid Expansion Medicaid Expansion 138% 0% Children Pregnant Women Parents Source: X Childless Adults Disabled Workers Disabled Elderly Ohio’s Health System Performance Health Outcomes – 42nd overall1 – 42nd in preventing infant mortality (only 8 states have higher mortality) – 37th in preventing childhood obesity – 44th in breast cancer deaths and 38th in colorectal cancer deaths Prevention, Primary Care, and Care Coordination1 – 37th in preventing avoidable deaths before age 75 – 44th in avoiding Medicare hospital admissions for preventable conditions – 40th in avoiding Medicare hospital readmissions Affordability of Health Services2 – 37th most affordable (Ohio spends more per person than all but 13 states) – 38th most affordable for hospital care and 45th for nursing homes – 44th most affordable Medicaid for seniors Sources: (1) Commonwealth Fund 2009 State Scorecard on Health System Performance, (2) Kaiser Family Foundation State Health Facts (updated March 2011) A few high-cost cases account for most Medicaid spending 100% 1% 3% 23% 80% 28% 60% 40% 96% 1% of the Medicaid population consumes 23% of total Medicaid spending 4% of the Medicaid population consumes 51% of total spending 49% 20% 0% Enrollment Spending Source: Ohio Department of Job and Family Services; SFY 2010 for all Medicaid populations and all medical (not administrative) costs Fragmentation vs. Coordination Multiple separate providers Accountable medical home Provider-centered care Patient-centered care Reimbursement rewards volume Reimbursement rewards value Lack of comparison data Price and quality transparency Outdated information technology Electronic information exchange No accountability Performance measures Institutional bias Continuum of care Separate government systems Medicare/Medicaid/Exchanges Complicated categorical eligibility Streamlined income eligibility Rapid cost growth Sustainable growth over time SOURCE: Adapted from Melanie Bella, State Innovative Programs for Dual Eligibles, NASMD (November 2009) “The critical flaw in our health care system … is that it was never designed for the kind of patients who incur the highest costs. Medicine’s primary mechanism of service is the doctor visit and the emergency room visit. It’s like arriving at a major construction project with nothing but a screwdriver and a crane.” Source: The New Yorker (Jan 24, 2011). Medical Hot Spot: Emergency Department Utilization: Ohio vs. US Hospital Emergency Room Visits per 1,000 Population 600 United States 500 436 400 365 452 366 450 372 Ohio 449 382 468 382 472 383 488 387 509 396 516 401 523 404 29% 300 200 100 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 Source: American Hospital Association Annual Survey (March 2010) and population data from Annual Population Estimates, US Census Bureau: http://www.census.gov/popest/states/NST-ann-est.html. Medicaid Hot Spot: Medicaid Enrollees Who Get Care Primarily from Hospitals* * Indicating a lack of primary care and/or care coordination Non-Institutionalized Medicaid Population Enrollment Spending Number % Amount % Average Cost Children 29,552 1.3% $510 million 5% $17,300 Adults 12,530 0.5% $841 million 8% $67,100 Total 42,082 1.8% $1.35 billion 13% $32,100 Source: Ohio Department of Job and Family Services for SFY 2010. Note that medical costs include those incurred by MCPs and paid by FFS, excluding institutionalized consumers and their costs. Consumers may have been in both FFS and MC delivery systems within SFY 2010. This analysis includes consumers costs in both systems. Medicaid Hot Spot: Hospital Admissions for People with Severe Mental Illness Avoidable hospitalizations per 1000 persons for ambulatory care sensitive conditions (avoidable with proper treatment) 8 Non-SMI 7 7.01 6 6.75 Severe Mental Illness (SMI) 5 4.86 4 3 3.53 3.69 4.18 3.24 2 2.33 1 0 Diabetes COPD Congestive Heart Failure Asthma Source: Ohio Colleges of Medicine Government Resource Center and Health Management Associates, Ohio Medicaid Claims Analysis (February 2011) Ohio Medicaid Spending Trend 9 percent average annual growth, 2008-2011 $25 Billion State General Revenue Fund All Other $20 $15 $13.5 $15.2 +12% $11.2 $15.8 +4% $18.0 +14% $14.3 $19.3 +7% $20.8 +8% $15.1 $14.0 $12.9 $9.1 $10 $5 + 42.8% $4.4 $4.0 $3.0 $5.3 $5.7 2012 2013 $3.8 $0 2008 2009 2010 2011 Source: Office of Health Transformation Consolidated Medicaid Budget, All Funds, All Agencies; actual SFY 2008-2010 and estimated SFY 2011-2013; “All Other” includes Federal Funds and Non-General Revenue Funds (non-GRF) The current Ohio HHS Medicaid organization Governor JFS DD MH ADAS Aging Health 12 Area Agencies on Aging 130 Local Health Departments Medicaid Single State Agency 130 County Offices 88 County Boards 56 Combined County Boards Medicaid as a % of Agency Budget JFS Medicaid Dev Disabilities Mental Health Alcohol and Drug Aging Health 73% 91% 61% 28% 83% 3% Agency Medicaid as a % of Total Ohio Medicaid 84% 8% 4% 0.3% 3% 0.1% ($13.3 billion) ($1.3 billion) ($590 million) ($63 million) ($534 million) ($17 million) Source: Legislative Service Commission, “Total Medicaid Spending by Agency” (State Fiscal Year 2010). John R. Kasich, Greg Moody, Governor Director • Elise Spriggs, Government Affairs • Eric Poklar, Communications • Monica Juenger, Stakeholder Relations Leadership Team “All Cabinet Agencies, Boards and Commissions shall comply with requests or directives issued by OHT, subject to supervision of their respective directors.” Policy Teams “OHT shall contract with state and/or private agencies for services in order to facilitate the implementation and operation of the OHT’s responsibilities.” Consultant Team Stakeholder Partners Prioritize stakeholder communication Michael Colbert John McCarthy John Martin Tracy Plouck Orman Hall Bonnie Kantor Dr. Ted Wymyslo (JFS) (Medicaid) (DODD) (ODMH) (ODADAS) (Aging) (Health) Source: Ohio Governor John R. Kasich, Executive Order 2011-02K (January 13, 2011) Executive Order Plan for the long-term efficient administration of the Ohio Medicaid Program and act to improve overall health system performance. In the next six months: 1. Advance the Administration’s Medicaid modernization and cost-containment priorities in the operating budget; 2. Initiate and guide insurance market exchange planning; 3. Engage private sector partners to set clear expectations for overall health system performance; and 4. Recommend a permanent Ohio health and human services organizational structure and oversee transition. Source: Ohio Governor John R. Kasich, Executive Order 2011-02K (January 13, 2011) The Vision for Better Care Coordination • Create a person-centered care management approach – not a provider, program, or payer approach • Services are integrated for all physical, behavioral, long-term care, and social needs • Services are provided in the setting of choice • Easy to navigate for consumers and providers • Transition seamlessly among settings as needs change • Link payment to person-centered performance outcomes Medicaid Hot Spot: Enrollment Spending by Top Managed Chronic Conditions 100% 80% 11% 23% 39% 60% 40% 31% Consumers with ONE of the top managed chronic conditions 30% Consumers without one of the top managed chronic conditions 66% 20% 0% Consumers with TWO OR MORE of the top managed chronic conditions Enrollment (2.3 million) Spending ($10.3 billion) Source: Ohio Department of Job and Family Services. Institutionalized consumers excluded. Based on SFY 2010 total medical cost either by ODJFS or Medicaid managed care plans. Top managed conditions = Diabetes, CAD, CHF, Hypertension, COPD, Asthma, Obesity, Migraine, HIV, BH, & Sub. Abuse. Ohio Health Transformation Priorities • • • • Improve Care Coordination Integrate Behavioral and Physical Health Rebalance Long-Term Care Modernize Reimbursement www.healthtransformation.ohio.gov A Case Study in Transformation: Ohio Department of Developmental Disabilities 30,000 GRF = $335M 25,000 Number of Individuals 20,000 15,000 10,000 5,000 2,637 2,683 2,807 4,495 5,550 5,601 5,663 0 1995 1996 1997 1998 1999 2000 2001 2002 2003 Waivers (Home and Community-based Care) 2004 2005 2006 2007 2008 2009 2010 DC (Developmental Center) 2011 A Case Study in Transformation: Ohio Department of Developmental Disabilities 30,000 GRF = $331M GRF = $335M 24,528 23,647 25,000 Number of Individuals 20,753 20,000 18,128 16,359 15,763 15,000 12,902 10,744 9,145 10,000 7,081 5,000 2,637 2,683 2,807 4,495 5,550 5,601 5,663 0 1995 1996 1997 1998 1999 2000 2001 2002 2003 Waivers (Home and Community-based Care) 2004 2005 2006 2007 2008 2009 2010 DC (Developmental Center) 2011 Ohio Medicaid Spending per Member per Month by Setting Institutional Services Waiver Services All Other Medicaid People with developmental disabilities $12,937 State Developmental Center $8,473 Private Intermediate Care Facility $5,568 Individual Options Transitions $4,819 $1,418 Level One People with other disabilities or over age 65 Nursing Facility $4,463 Home Care $4,584 $4,067 Transitions Aging $2,058 $1,869 $1,695 $1,356 Choices Assisted Living PASSPORT Other in Managed Care $530 Other in Fee-for-Service Other children and parents Fee-for-Service $298 $254 Managed Care 0 2000 4000 6000 8000 10000 12000 14000 Source: Ohio Department of Job and Family Services. Includes claims incurred from July 2009 through June 2010 and paid through October 2010; cost differences between institutional and waiver/community alternatives do not necessarily represent program savings because population groups being compared may differ in health care needs. Ohio Medicaid Residents of Institutions Compared to Recipients of Home and Community Based Waivers 70,000 Home and Community Based (Aging, JFS, and DD waiver recipients) 65,000 65,907 60,000 60,128 58,609 55,000 57,597 56,011 56,891 56,503 Facility-Based 52,745 50,000 45,000 59,979 (NF, ICF/DD, Developmental Center residents) 46,965 40,000 2006 2007 2008 2009 2010 Source: Ohio Department of Job and Family Services; based on average monthly recipients for SFYs 2006-2010. Medical Hot Spot: Per Capita Health Spending: Ohio vs. US US Ohio Percentage Difference Affordability Rank (Out of 50 States) Total Health Spending $5,283 $5,725 + 8% 37 Hospital Care $1,931 $2,166 + 12% 38 Physician and Clinical Services $1,341 $1,337 - 0.3% 27 Nursing Home Care $392 $596 + 52% 45 Home Health Care $145 $133 - 8.3% 35 Measurement Source: 2004 Health Expenditure Data, Health Expenditures by State of Residence, Centers for Medicare and Medicaid Services, Office of the Actuary, National Health Statistics Group, released September 2007; available at http://www.cms.hhs.gov/NationalHealthExpendData/downloads/res-us.pdf Medicaid Hot Spot: Per Enrollee Medicaid Spending: Ohio vs. US US Ohio Percentage Difference Affordability Rank (Out of 50 States) All Enrollees $5,163 $5,781 + 12.0% 36 Children $2,135 $1,672 - 21.7% 7 Adults $2,541 $2,844 + 13.5% 18 Elderly $12,499 $18,087 + 44.7% 44 Disabled $14,481 $15,674 + 8.2% 33 Measurement Source: 2007 The Urban Institute and Kaiser Commission on Medicaid and the Uninsured estimates based on data from Medicaid Statistical Information System (MSIS) and CMS64 reports from the Centers for Medicare and Medicaid Services (CMS), 2010. Unused Nursing Home Capacity In 70 counties more than 10% of beds are empty Williams 25.6% Fulton 9.2% Defiance 19.4% Paulding 29.4% Van Wert 17.8% Putnam 21.2% Darke 18.5% Miami 9.6% Hardin 21.3% Preble 9.5% Montgomery 11.5% Butler 15.1% Warren 9.8% Union 11.9% Champaign 31.8% Madison 7.0% Greene 13.4% Clinton 19.4% Hamilton 12.7% Fayette 9.2% Brown 20.0% Adams 13.6% Ashland 11.9% Pike 12.0% Scioto 12.3% Wayne 16.6% Holmes 8.0% Morrow 21.1% Knox 21.2% Licking 15.7% Fairfield 12.3% Muskingum 10.4% Perry 17.8% Vinton 25.4% Trumbull 14.5% Portage 10.8% Morgan 7.2% Athens 6.6% Gallia 13.7% Mahoning 14.8% Stark 14.5% Columbiana 12.0% Carroll 13.8% Tuscarawas 16.3% Harrison 9.2% Guernsey 20.4% Noble 22.3% Meigs 11.7% Jackson 10.5% Lawrence 13.5% Summit 10.4% Geauga 6.6% Coshocton 17.2% Hocking 13.3% Ross 7.8% Highland 10.5% Clermont 11.7% Pickaway 7.2% Medina 16.1% Richland 13.5% Delaware 11.2% Franklin 12.6% Cuyahoga 14.1% Lorain 13.6% Huron 14.6% Crawford 14.7% Marion 13.0% Logan 12.5% Clark 16.5% Erie 16.4% Seneca 14.4% Wyandot 14.5% Allen 15.6% Shelby 8.0% Sandusky 14.0% Hancock 9.9% Auglaize 18.6% Mercer 15.9% Ottawa 35.1% Wood 14.6% Henry 23.2% Ashtabula 21.0% Lake 11.8% Lucas 15.4% Jefferson 17.1% Belmont 10.0% Monroe 8.5% Washington 10.5% Nursing Facility Surplus Percentage of total bed days vacant 6.6% - 10.4% 10.5% - 12.5% 12.6% - 16.3% 16.4% - 23.0% 23.1% - 35.1% Rebalance Long Term Care Enable seniors and people with disabilities to live with dignity in the settings they prefer RECOMMENDATIONS: • Create a Single Point of Care Coordination • Consolidate and Streamline Waiver Programs • Reward Person-Centered Outcomes in Nursing Homes • Expect Greater Efficiency from NF and Waiver Providers • Decrease payments to “hold” empty beds • Reduce the nursing home franchise fee • Saves $427 million all funds over the biennium Research suggests that person-centered care is associated with improved organizational performance including higher resident and staff satisfaction, better workforce performance and higher occupancy rates. Source: 2010 Annual Quality Report, Alliance for Quality Nursing Home Care and American Health Care Association Ohio Health Transformation Priorities • • • • Improve Care Coordination Integrate Behavioral and Physical Health Rebalance Long-Term Care Modernize Reimbursement www.healthtransformation.ohio.gov Balance the Budget Contain Medicaid program costs in the short term and ensure financial stability over time RESULTS: • A sustainable system • $1.4 billion in net savings over the biennium • Align priorities for consumers (better health outcomes) and taxpayers (better value) • Challenge the system to improve performance (better care and cost savings through improvement) Total Ohio Medicaid Expenditures, SFY 2010 Medicare Buy In and Part D, 3% Managed Care Administration, 3% Other, 12% Hospital, 28% Drugs, 9% Physicians, 8% Home and Community Services, 14% Nursing Facility, 17% Intermediate Care Facilities for the Developmentally Disabled and Developmental Centers, 5% Source: Ohio Department of Job and Family Services and the Governors Office of Health Transformation. Managed care expenditures are distributed to providers according to information from Milliman. Hospitals include inpatient and outpatient expenditures as well as HCAP Home and community services include waivers as well as home health and private duty nursing. Medicaid Budget: Savings and Investments Modernize Hospital Payments Reform Nursing Facility Payments Manage Behavioral Health Service Utilization Reform Managed Care Plan Payments Reduce PASSPORT rates and service utilization Align Programs for People with DD Nursing and Home Health Payment Reform Reduce Admin for Federal Agencies on Aging Link Nursing Home Payments to Quality Create a Unified Long Term Care System Elevate Behavioral Health Financing to the State Integrate Behavioral/Physical Health Benefits Create a Single Point of Coordination Implement Federal Reform Mandates Promote Health Homes Provide Accountable Care for Children -$478 -$427 -$243 -$159 -$137 -$62 -$35 -$24 $0 $0 $0 $0 $0 $35 $47 $87 -$500 -$400 -$300 -$200 -$100 $0 $100 in millions Source: Office of Health Transformation (March 15, 2011) Medicaid Budget: Impact on Rates by Provider Nursing Facilities -7.3% Outpatient Hospital PMPM -6.7% -4.9% Nursing Services per 4 hours PASSPORT Provider Rates -3.0% -2.5% Aide Services per 4 hours Inpatient Hospital PMPM -1.8% Managed Care Plans -1.0% ICF-DD 0.6% 8.8% -8% -6% -4% -2% 0% 2% 4% 6% Physician 8% Estimated change in rate Source: Office of Health Transformation (March 15, 2011) What this budget does NOT do • • • • • Does not cut eligibility Does not cut optional services, including dental Does not make arbitrary across-the-board cuts Does not resort to smoke and mirrors Does not count hypothetical savings Thank you. Greg Moody, Director Governor's Office of Health Transformation 77 South High Street, 30th Floor Columbus, Ohio 43215 Phone: 614-752-2784 Email: greg.moody@governor.ohio.gov