Mock Trial Script - cindyTwhite
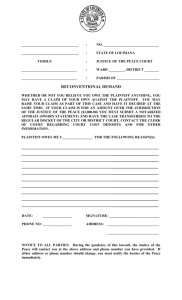
advertisement

Running head: MOCK TRIAL METHOD 1 Using a Mock Trial Method to Address Clinical Practice Issues and Enhance Teaching Effectiveness of Evidence Based Practice in Nursing. Cindy T. White DNPc, MA, RN, CNML N789 DNP Project December 2012 Submitted to DNP Committee: KT Waxman, DNP, MBA, RN, CNL DNP Committee Chair Judith Karshmer, PhD, RN, PMHCNS-BC Pat Cornett, EdD, MSN, RN DNP Committee DNP Committee MOCK TRIAL METHOD 2 Table of Contents ABSTRACT .................................................................................................................................... 3 DEFINITIONS OF TERMS USED IN THIS PAPER: .................................................................. 4 USING A MOCK TRIAL METHOD TO ADDRESS CLINICAL PRACTICE ISSUES AND ENHANCE TEACHING EFFECTIVENESS OF EVIDENCE BASED PRACTICE IN NURSING ....................................................................................................................................... 5 SECTION I ................................................................................................................................. 5 SECTION II .............................................................................................................................. 19 SECTION III............................................................................................................................. 30 SECTION IV ............................................................................................................................ 42 SECTION V .............................................................................................................................. 48 REFERENCES ............................................................................................................................. 55 APPENDIX A ............................................................................................................................... 60 Tally Sheet of Quality Ratings .................................................................................................. 60 APPENDIX B ............................................................................................................................... 61 Rating the Quality of the Evidence ........................................................................................... 61 APPENDIX C ............................................................................................................................... 63 IRC Application ........................................................................................................................ 63 APPENDIX D .............................................................................................................................. 72 STEPS IN MOCK TRIALS ...................................................................................................... 72 APPENDIX E ............................................................................................................................... 84 Cast of Characters ..................................................................................................................... 84 APPENDIX F................................................................................................................................ 89 Mock Trial Script ...................................................................................................................... 89 APPENDIX G ............................................................................................................................. 146 PowerPoint .............................................................................................................................. 146 APPENDIX H ............................................................................................................................. 163 Mock Trial Agenda ................................................................................................................. 163 APPENDIX I .............................................................................................................................. 164 Elements Of Negligence Deliberation Worksheet .................................................................. 164 APPENDIX J .............................................................................................................................. 165 Pre and Post Survey Questions ............................................................................................... 165 APPENDIX K ............................................................................................................................. 167 Polling Outcomes .................................................................................................................... 167 MOCK TRIAL METHOD 3 ABSTRACT Traditional teaching methodologies that are teacher-centered (passive, instructor-led) instead of learner-centered (active, learner-interactive) may not be the most effective methodology for educating the adult learner. In addition, the perceived relevance of a topic as related to the attitude or inherent values of the learners has profound impact on the success of a teaching goal. Teaching to the ‘evidence’ that substantiates best practice for the bedside clinician requires not only specific knowledge of the science, it also requires a systematic approach to transfer this knowledge into skills at the bedside and clinical inquiry of the learner’s own practice. Collectively these issues present challenges to nurse educators as they strive to convey the significance of practicing to the best evidence and defending this through clinical documentation as it relates to achieving optimal patient outcomes. A mock trial experiential educational activity was selected as the best way to demonstrate the value of a learner-centered approach as adjunct education to convey the practice of nursing, evidence-based practice, legal documentation, and patient outcomes related to a newly implemented opioid sedation scale. The simulated role-play trial was used as an engaging courtroom drama where the nurse ‘defendant’ was challenged to substantiate practice based on ‘evidence.’ Seminar ‘jury’ participants scrutinized testimony through deliberation and then delivered the final verdict. Keywords: mock trial, nursing, healthcare, evidence-based practice, learner-centered education MOCK TRIAL METHOD 4 DEFINITIONS OF TERMS USED IN THIS PAPER: Evidence-Based Practice: the practice of nursing in which the nurse makes clinical decisions based on the best available current research evidence, his or her own clinical expertise, and the needs and preferences of the patient. (Mosby, 2009) Traditional teaching methods: teacher-centered, classroom lecture, discussion, note taking, memorization, and learning packets. (DeYoung, 2008) Learner centered teaching methods: a teaching methodology that emphasizes the importance of understanding and catering to the students' needs, interests, and abilities. (Education.com, 2012) Simulation: the imitation or representation of one act or system by another. (SSIH, 2012) Role Play: a learning activity in which participants act out a set of defined role behaviors or position with a view to acquiring desired experiences. (Sogunro, 2004) Mock Trial: a simulated trial that involves active participation in a fictitious courtroom case. (Mock Trial Academy, 2011) Shared Governance: a decentralized system of management in which shared decisionmaking is based on the principles of partnership, equity, accountability, and ownership at the point of service. (Swihart, 2006) High Alert Medications: drugs that bear a heightened risk of causing significant patient harm when they are used in error. (ISMP, 2012) MOCK TRIAL METHOD 5 Audience Response System (ARS) – a device that allows a group of people to vote on a particular question or topic remotely while communicating to a main computer for polling and tabulating results. (Martyn, 2007) USING A MOCK TRIAL METHOD TO ADDRESS CLINICAL PRACTICE ISSUES AND ENHANCE TEACHING EFFECTIVENESS OF EVIDENCE BASED PRACTICE IN NURSING SECTION I The value of evidence-based practice (EBP) and its impact on professional nursing practice and patient care outcomes have been garnering the attention of healthcare practitioners within the past few years. EBP has been incorporated into revised nursing practice standards and guidelines such as the American Nurses Association (ANA) Standards of Professional Nursing Practice (American Nurses Association, 2010), are fundamental elements in the Quality and Safety Education for Nurses (QSEN) competencies (QSEN, 2012) and critical components of the prestigious American Nurses Credentialing Center (ANCC) Magnet designation. (ANCC, 2012) EBP is defined as the practice of nursing in which the nurse makes clinical decisions based on the best available current research evidence, his or her own clinical expertise, and the needs and preferences of the patient. (Mosby, 2009) Knowing about and practicing to a set of standards has an impact on safe patient care and legitimizes existing evidence through improved patient outcomes. (Pravikoff, 2005) (Titler, 2008) Teaching evidence-based practice provides a challenge to the nurse educator as it compels a strong relationship between education and practice. (Pennington, 2010) Traditional teaching methodologies that are teacher-centered or passive learning instead of learner-centered or active learning can present challenges to adult learners. Traditional approaches to teaching and training methodologies such as instructor-centered lectures and learner centered self-study modules do not produce the change in knowledge, skills, and attitudes (KSA) that is essential for MOCK TRIAL METHOD 6 change in practice performance and translation to the improvement of patient outcomes at the bedside. In fact, traditional teaching methods often deter learning and practice change due to the passive exchange of knowledge. (Biddinger, 1999) There is therefore a need to supplant the traditional self-learning module efforts for more non-traditional, interactive approaches centered on the learners not the educators. Concomitant with training methodology is the attitude or inherent values of the learner. Intrinsic motivation or value of the learning experience may be inherent within and significant to the learner and/or conveyed during instruction. Whatever the case, the value or belief in what is being taught is key to adoption and application of essential learning components. Instructional strategies then must be intentional to elicit intrinsic value for adoption and application of learned principles to practice. Instructional strategies can be designed to invite the learner to value the learning. Certain conditions can be ascribed to the learning in order to enhance intrinsic motivation as noted below(Wlodkowski, 1999): Inclusion – creating an environment of respect and connectedness between learner and instructor. Attitude – creating a favorable environment and disposition for the learner by establishing relevance. Meaning – creating thought provoking and challenging experiences that include the learner perspectives and values. Competence – creating an environment for learner understanding and engagement of content value to practice. Inclusion of these principles in instructional design helps to keep attention focused on the learning and the learner. MOCK TRIAL METHOD 7 Collectively, all these issues combined present challenges to nurse educators as they strive to convey the significance of clinical practice concerns, achieving optimal outcomes through applying the best evidence to guide their practice, and defending all of this through clinical documentation. The basis for crafting effective teaching methods for EBP and to bring about change in the learner to affect performance at the point of service remains an area to be explored and validated. Kahn and Coomarasamy (Khan, 2006) proposed a hierarchy of teaching and learning methods for evidence-based practice based on educational evidence, theory and principles referenced in Table 1 below. Level 1 includes EBP that is clinically integrated into teaching and Table 1. Hierarchy of Evidence-Based Medicine Teaching and Learning Level 1: Interactive, and clinically integrated teaching and learning activities. Level 2: a. Interactive, classroom based teaching and learning activities. b. Didactic, but clinically integrated teaching and learning activities. Level 3: Didactic, and classroom or stand-alone teaching and learning activities. is more effective than classroom instruction due to the interrelationship and unification of the clinical subject into the teaching and learning. By its very nature, the interactive component is reflective for the learner as it allows for discovery of gaps in knowledge and bridging of new information; it encourages deeper learning that is important for understanding and transference of new learning into practice. Level 2 includes interactive, classroom teaching or didactic but clinically integrated teaching, i.e., that involves some type of activity such as role-play, small MOCK TRIAL METHOD 8 group work, or case discussions. Didactic teaching should be clinically relevant and as such focus on the evidence as related to the patient problem. Level 3 includes didactic, classroom, or stand-alone teaching which are more ‘traditional’ in approach such as instructor-led presentations. This level is the least effective for the learner due to its passive style of learning that encourages more superficial understanding and application. (Khan, 2006) These levels suggest that in order to effectively teach evidence-based practice in nursing, it becomes necessary to incorporate learner based interactive activities into the teaching methodology along with current and clinically relevant patient issues. Demonstrative of Khan’s claims is the growing body of evidence that suggests the use of simulation as an educational tool becoming increasingly prevalent, relevant, and effective in health care practices today. More academic and service institutions have adopted simulation as a training methodology for healthcare professionals in the past several years than ever before. The simulated experience provides a teaching environment where there is a link to instruction and the cognitive processes of perceiving, thinking, and processing information. Simulation role-play involves replaying, re-evaluating, and experiencing the feelings associated with the experience. This involves active reflection and thinking through the actions and outcomes, as they are performed real time. (Rutherford-Hemming, 2012) As simulation use has increased, so has the literature yielding evaluation and validation of this as a teaching approach. In particular, simulation of a mock trial role-play has been shown to teach standards, regulatory requirements, policies, procedures, documentation, scope of practice, and legal implications all at the same time. (Patrick, 2007) Though increasing in popularity with academic institutions, evaluation of effectiveness in clinical practice outcomes continues to be an area in need of further research study. MOCK TRIAL METHOD 9 The Clinical Concern Incorporated into the philosophy of a large San Francisco Bay Area trauma center is an organizational commitment to performance improvement through ongoing assessment and improvement in outcomes of patient care. Performance improvement requires a coordinated and integrated system-wide approach and staff that are committed to a cooperative effort to improve care by actively participating in the identification, assessment, and improvement of patient care processes and outcomes. Through examination of the existing process to assess patients following opioid infusion for pain management, it was determined that there were inconsistencies in nursing practice standard of performance and inadequate tools to inform early detection and intervention of increasing patient sedation and ensuing respiratory depression. Upon review and evaluation of current variation in practice along with a rise in the administration of reversal agents given for advanced respiratory depression in patients, it was determined there was a need for a systematic way to monitor sedation levels to prevent, monitor and manage patients with intravenous infusion of high alert opioid medications. The Post Anesthesia Care Unit (PACU) nursing staff conducted a literature search to investigate current best practices in assessing and monitoring sedation levels for patients receiving opioid infusions for pain management. Their findings indicate that gradual increases in sedation are early warning signs of ensuing respiratory depression, leading pain experts to recommend that the level of sedation must be monitored routinely along with the management of and accompanying decrease in opioid administration until the patient demonstrates an acceptable level of sedation. (Pasero, 2009) In addition, they learned that according to a study done by Nisbet and Mooney-Cotter, (Nisbet, 2009) the Pasero Opioid Sedation Scale (POSS) was found to be the most valid and reliable tool, particularly for MOCK TRIAL METHOD 10 informing the nursing process and decision-making. The POSS tool scored highest in ease of use with clear guidelines for nursing and confidence in making clinical decisions for patient care management. The POSS scale links the interventions to the level of sedation and is displayed in Table 2. Table 2. Pasero Opioid Sedation Scale (POSS) ATTRIBUTES INTERVENTIONS S= Sleep; easy to arouse. S= Acceptable. No action necessary. Supplemental opioid may be given if needed. 1= Awake and alert. 1= Acceptable. No action necessary. Supplemental opioid may be given if needed. 2= Slightly drowsy; easily aroused. 2= Acceptable. No action necessary. Supplemental opioid may be given if needed. 3= Frequently drowsy; arousable; drifts off to 3= Unacceptable. Decrease opioid sleep during conversation. dose by 25–50 percent . Administer acetaminophen or an NSAID, if not contraindicated, to control pain; monitor sedation and respiratory status closely until sedation level is less than 3. 4= Somnolent. Minimal or no response to 4= Unacceptable: Stop opioid. Notify physical stimulation. anesthesia provider; very slowly administer dilute IV naloxone (0.4 mg naloxone in 10 mL saline; 0.5 mL over 2-minute period); administer acetaminophen or an NSAID, if not contraindicated, to control pain; monitor sedation and respiratory status closely until sedation level is less than 3. The PACU nurses presented their findings to various nursing practice committees and received approval for implementation of the POSS. The traditional approach to education through a self-study learning module was developed by the Nursing Education Department and assigned to all clinical nursing staff. Nurse educators believed that additional reinforcement of educational efforts was required post implementation based upon the fact that this was a change in nursing practice. The basic learning model in support of an additional educational strategy MOCK TRIAL METHOD 11 requiring learner involvement can be seen in the Learning Pyramid, Figure 1. The Learning Pyramid provides supporting evidence for best practices in learning through more participatory teaching methods. The Learning Pyramid was developed by the NTL Institute for Applied Behavioral Science in the early 1960s and illustrates that active participation in the learning process results in more effective retention of learning. (NTL Institute, 2012) Figure 1. The Learning Pyramid To summarize the percentages in the pyramid (which are sometimes cited slightly differently) indicate that learners retain approximately 90% of what they learn when they teach someone else/or use immediately; 75% of what they learn when they practice what they learned; 50% of what they learn when engaged in a group discussion; 30% of what they learn when they see a demonstration; 20% of what they learn from audio-visual; 10% of what they MOCK TRIAL METHOD 12 learn from reading; and 5% of what they learn from lecture. This is a strong and sturdy defense for active, participatory learning to involve all the senses. The shared governance nursing Education Council (Council) along with the Nursing Education Department were subsequently challenged to design an effective learning approach that would have a direct impact on the nurses’ learning and adoption for practice performance. Discussion with the Council resulted in a unanimous decision to employ a mock trial experiential approach to educating the staff. The design would be an all day staff development continuing education program to engage nurses in a role-play courtroom drama where the nurse ‘defendant’ would be challenged to substantiate her practice based on the value and adoption of the best ‘evidence.’ National nursing initiatives provide the support and standards for nurses as they critically examine their practice and select the best evidence that informs quality and safe patient experiences and outcomes. The Quality and Safety Education for Nurses (QSEN) project was launched and funded by the Robert Wood Johnson Foundation in 2005 with the goal to address the challenge of preparing future nurses with the knowledge, skills, and attitudes (KSA) necessary to continuously improve healthcare quality and safety. These goals have been widely accepted and adopted in schools of nursing and are beginning to be further adapted into acute care practice settings. In order to accomplish these goals, six competencies were developed and based upon the Institute of Medicine goals for safety. Whether or not these competencies are fully adapted into all practice settings and become the national standard, there is little dispute that these are essential components of safe and quality nursing and patient care practices. In the context of the search for best practices and in the development of the mock trial script, all six of the QSEN competencies were addressed and are described in Table 3. MOCK TRIAL METHOD 13 Table 3. Quality and Safety Education for Nurses (QSEN) Competency 1. Patient Centered Care 2. Teamwork and Collaboration 3. Evidence Based Practice 4. Quality Improvement 5. Safety 6. Informatics Definition Recognize the patient or designee as the source of control and full partner in providing compassionate and coordinated care based on respect for patient's preferences, values, and needs. Function effectively within nursing and interprofessional teams, fostering open communication, mutual respect, and shared decision-making to achieve quality patient care. Integrate best current evidence with clinical expertise and patient/family preferences and values for delivery of optimal health care. Use data to monitor the outcomes of care processes and use improvement methods to design and test changes to continuously improve the quality and safety of health care systems. Minimizes risk of harm to patients and providers through both system effectiveness and individual performance. Use information and technology to communicate, manage knowledge, mitigate error, and support decision-making. (Cronenwett) (Institute of Medicine, 2003) Theoretical Framework Teaching and learning models that informed this project were centered on the MOCK TRIAL METHOD 14 constructivist learning theory. Constructivists believe that knowledge is constructed when an individual attaches meaning to an experience or activity. (Merriam, 2007) This theory posits that learning is an active versus passive endeavor that includes dialogue, collaborative and cooperative learning. The key foundational beliefs of constructivists are that personal and social transformation involves a cognitive change in the way meaning is constructed, therefore, it is easier to connect to a transformational learning experience. David Kolb, professor of organizational behavior, viewed learning as a concrete experience whereby the process of knowledge attainment is created by transformation of the learning through reflection, observation, cognition, and behavior. (Lisko, 2010) According to Kolb, learning is a continuous process and knowledge is created by transforming experience into existing cognitive frameworks, thus changing the way the learner thinks and behaves. He postulated that “learning is the process whereby knowledge is created through the transformation of experience” (Kolb, 1984)) and that learners require varied experiences in order to grasp key concepts. Kolb’s four-stage cyclical theory of experiential learning theory is a holistic perspective that combines experience, perception, cognition, and behavior. The model of learning is such that learners may begin at any stage, but must follow each other in the sequence: 1. Concrete experience (or “DO IT”) 2. What happened; reflective observation (or “OBSERVE”) 3. So what? abstract conceptualization (or “THINK”) 4. Now what? active experimentation; test out in new situation (or “PLAN”) MOCK TRIAL METHOD 15 Figure 2. Kolb’s Experiential Learning Cycle The simulated role-play creates the environment for active learning to occur; the participant constructs knowledge by attaching meaning to the mock trial experience and connecting that knowledge to the current or future practice of nursing and the patient care issues emphasized. The construction of the knowledge learned could be from a personal constructive orientation or value of the experience to the individual participant or a social constructive orientation or the way in which meaning is derived from the collective experience of all participants, faculty, and scripted role-play. The experience is intentionally designed and certain to include dialogue, collaborative and cooperative learning between the participants, with other participants and with instructor(s). Simulation of the real world experience provides the opportunity for a transformed experience and creates an atmosphere where internal and external processes of learning can occur. The constructed environment is also conducive to reflective thinking that challenges the participant to contemplate how he or she might act and think differently if approached with a similar situation in the actual practice setting. MOCK TRIAL METHOD 16 Finally, continuing competence and lifelong learning are fundamental to the profession of nursing and thus professional development activities become essential underpinnings. The reinforcement and enrichment of learning through the construction of an all day educational program and mock trial was aligned with the obligations in nursing for ongoing professional development. Lifelong learning is a professional nursing responsibility that involves active participation in activities that develop and maintain competence, enhance professional practice, and support achievement of career goals. Nursing professional development builds on the educational and experiential bases of nurses across the continuum of their professional careers towards the ultimate goal of ensuring the quality of health care to the public. Nursing professional development activities can be described as existing in the domains of continuing education, staff development, and academic education. As seen in Figure 3, these areas overlap as individuals select the most effective way to meet their professional development needs and as educators engage in their practice roles. Staff development includes continuing education activities, academic education, or both as preparation for practice. Continuing education can be part of staff development, part of a formal academic program, or study in an accredited program for the purpose of enhancing nursing practice. (American Nurses Association, 2010) MOCK TRIAL METHOD 17 Quality of Care Continuing Education Staff Development Academic Education Professional Development Activities Figure 3. Framework for Nursing Professional Development (adapted from Scope and Standards of Practice for Nursing Professional Development) (American Nurses Association, 2010) The use of a professional development framework sanctions a commitment at the national level and supports ongoing advancement. Increased education makes possible a shift from current reality to the preferred outcomes of enhanced learner results -- a goal to which all educators should subscribe. Assumptions To quote C.S. Lewis, “the most dangerous ideas in a society are not the ones being argued, but the ones that are assumed.” Assumptions for this project were that: The strategic teaching design methodology of the mock trial approach will be effective in engaging participants in realizing the value of adoption of the new POSS tool for practice change. MOCK TRIAL METHOD This approach will help nurse participants to positively and actively engage in the learning process. Nurse participants will be able to recognize stated and unstated suppositions during the course of the trial role-play. This approach will foster retention of learning for at least 6 months post program. The perceived advantage of this type of training assumes that the degree of difficulty or complexity influences the approach or methodology. In an effort to validate adoption and effectiveness of this type of teaching and learning strategy, a pre and post program survey was designed and is described in Section IV. Goals Project goals were three-fold: 1) establish a fun, innovative, and engaging day for the participants, 2) design a relationship between nursing practice, EBP, documentation, legal implications, and patient outcomes, and 3) reinforce previous learning regarding the POSS opioid sedation scale. An additional measure of success would be the enrichment of the participants desire to learn and the value their practice through reflection, critical thinking, reasoning, decision-making and clinical inquiry. Theoretical Framework The framework, used to inform improvement at the point of care was the Institute for Healthcare Improvement (IHI), Plan-Do-Study-Act (PDSA) rapid cycle model for change in healthcare process and outcomes and shown in Figure 4. (Langley, 2009) 18 MOCK TRIAL METHOD 19 PDSA Cycle Act Plan Study Do Figure 4. PDSA Improvement Model During the ‘Plan’ part of the cycle, the focus of the learning is centered on the specific concern to be addressed, the ‘target’ audience, as well as current process and standards of care. Identification of the root cause of the problem can also occur during this phase so evaluation metrics can be designed. The specific concerns of this project were centered on discovery of the root cause of over-sedation; identifying a new EBP tool, best practice protocols, and standards of care, which would enable early detection and intervention through use of the POSS scale. The ‘Do’ phase of the cycle is the implementation of the plan. This involved the design of the daylong training and mock trial with content relevant to the practice concern. The ‘Study’ phase is the analysis of the evaluation results or the pre and post measurements. The ‘Act’ phase of the cycle is the process to monitor the gains through ongoing established metrics. SECTION II A review of the literature was conducted to investigate previous interventions to support the validity of choosing a simulated role-play, mock-trial approach for teaching evidence-based MOCK TRIAL METHOD 20 practice. The specific and supporting articles using search terms for innovation, teaching EBP in nursing, mock trial, role-play, simulation, and audience response systems were located using CINAHL Plus. The inclusion criteria was set based on information from articles published no earlier than 2009, conducted in the United States, preferably in hospital settings, and teaching of EBP, mock trial, or simulated role play for clinical nursing practice. Though much is written about use in academic settings, there is little published about use in hospital settings that met the specific criteria. Thus, additional criteria were added to broaden the review of literature. The articles are described in the following subsections. A tally sheet for rating the quality of the evidence in each article can be found in Appendix A; relevance and validity criteria for quality ratings can be found in Appendix B. Innovation Phillips and Vinten (Phillips, 2010) designed a study to measure how faculty perceive and describe the characteristics of innovative teaching strategies. They found that Rogers’ theory of diffusion of innovation - compatibility, trial-ability, and relative advantage – was the most influential in the adoption of innovative teaching strategies. The participants included in the study were a convenience sample of clinical faculty who completed an online course designed to orient faculty to the principles of teaching and learning in the clinical setting. (N=71 or a 95% response rate) The majority of faculty (58%) had been teaching nurses for up to two years ; 41% taught in associate degree programs. Fifty-six percent had worked as nurses for more than 20 years, and 53% had a master’s degree as the highest level of education. A four section instrument developed by the authors was used to measure demographic characteristics, innovativeness of ten teaching strategies (Table 4), the influence of Roger’s five perceived characteristics of innovation on their likeliness to adopt future innovative teaching strategies MOCK TRIAL METHOD (Rogers, 2003), along with two open-ended questions: a) describe any innovative teaching strategies that you presently use in the clinical setting, b) describe any innovative teaching strategies that you intend to use in the clinical setting in the future. All scores other than the open ended questions were measured on a five point Likert scale 1 = strongly disagree, 5= strongly agree. Table 4. Socio-Culturally Based Teaching Strategies (Bonk, 1998) 1. Role Modeling to illustrate performance/practice standards and verbalize internal processes. 2. Coaching to observe and supervise students in guiding them toward expert performance/practice. 3. Providing guidance in supporting what learners cannot yet do and gradually removing that support as competence is displayed. 4. Questioning to request verbal response for learners by supporting them with mental functions they cannot produce alone. 5. Encouraging student articulation of their reasoning and problem-solving process. 6. Encouraging student exploration and application of their problem-solving skills. 7. Fostering student reflection and self-awareness. 8. Providing cognitive task structuring by explaining and organizing the task to guide students toward maximizing their potential. 9. Managing instruction with constructive feedback and positive reinforcement. 10. Using direct instruction to provide clarity and any additional learning content. 21 MOCK TRIAL METHOD 22 The “exploration and application” category of teaching strategies was the most frequently cited for both current use and intent to adopt in the future (n=46). Examples included in this category were use of concept maps, role-playing, simulation, and live vignettes. The most frequent categories of innovative teaching strategies respondents intended to adopt included exploration, application, reflection, and self-awareness. All of these promote student centered learning experiences. All 71 respondents agreed that innovation would influence their adoption for future teaching strategies. These findings help to inform the growing body of knowledge that demonstrates the changing role of the clinical nurse educator from teacher- centered, unchallenged experts, to student – centered, experiential and self-reflective styles. This study sets the backdrop for the future evaluation of the design of specific educational programming and methodologies and adoption of innovation as effective teaching and learning strategies. Teaching EBP A cross sectional survey study by Gerrish, et al, (Gerrish, 2011) was conducted to identify factors influencing advanced practice nurses’(APN) contribution to promoting evidencebased practice among front-line nurses. For the purpose of this study, APN was defined as any nurse working in the area of adult nursing whose role involved an element of clinical practice requiring expert knowledge and skill. The study included 855 advanced practice nurses working in 87 hospital/primary care settings in England. The survey examined the respondents’ understanding of evidence-based practice, sources of evidence used, ways of working with frontline nurses, perceived impact on front-line nurses, skills in evidence-based practice and barriers to promoting evidence-based practice. The questionnaire was comprised of 66 items addressing the following areas: Understanding EBP MOCK TRIAL METHOD Barriers to promoting EBP Biographical information Sources of evidence used by APNs Methods of working with front-line nurses Impact of the role on care given by front-line nurses Self-assessment of knowledge and skills to support EBP 23 Respondents were asked to give a free text description of their understanding of EBP and how they influenced front-line nurses to engage in EBP at the bedside. There was less agreement on whether APNs perceived that the information they gave to patients subsequently influenced the care given by front-line nurses and less agreement on the extent to which the APNs were able to create a culture in which front line nurses felt able to question practice. Data was analyzed using descriptive statistics. Comparisons were made between advanced practice nurses with masters of science in nursing (MSN) degrees and those with less than a masters degree) 36.5% held a bachelors degree, 28.9% held a masters degree, 0.7% held a doctorate degree, 19.5% held a diploma degree; and 14% ‘other’). Findings revealed that APNs used different sources of evidence, engaged in various activities to promote evidence-based practice and had a positive influence on front-line nurses’ practice. APNs with Masters degrees perceived themselves to be more skilled in all aspects of evidence-based practice than those with lower qualifications. In relationship to research, 45% of the APNs identified themselves as being a novice yet demonstrated they are clinical leaders that promoted EBP of front-line nurses but require further development of their own EBP skills as well. Another article described the challenges of teaching EBP in accelerated second-degree programs. (Kruszewski, 2009) In one program delivered in a twelve month format, the EBP MOCK TRIAL METHOD 24 curriculum was intentionally designed using a collaborative model where academic faculty shared the concepts of EBP with ad clinical nurses in the practice setting who then guided the implementation with student’s active participation. Two goals of the program required students to gain competency in developing EBP solutions to clinical problems in the practice setting, and to develop learning experiences that built on the experiences of second-degree, diverse, and adult learners. Students were required to enroll in two specifically designed courses: EBP, and Acute Care of Patients and Families Across the Life Span. Learning activities within and between academic faculty and nursing clinicians were shared with the aim of delivering a final product that would be useful in the clinical setting. Teaching and learning strategies were designed to integrate EBP in the clinical setting to provide relevance for the adult learner thus making the work meaningful. The EBP course used topics from the Iowa Model of EBP to Promote Quality Care and Rogers diffusion of innovations model. (Doody, 2001) (Rogers, 2003) Content was delivered by web based learning modules supplemented by weekly classroom ‘help’ sessions. In the Acute Care of Patients and Families Across the Life Span course, students worked with clinical nursing staff to identify a clinical problem that was a priority for the patient care area. Students worked together in groups to design an EBP protocol using the steps in the Iowa Model of EBP. Academic instructors collaborated with each other as well as the clinical nursing units and the students to help design final project and poster presentation to be delivered to staff, students, and faculty. The cohort consisted of 24 students ages 22 to 45. Previous degrees included: engineering, social work, business, liberal arts, and biological sciences. Most of the students held bachelors degrees as their level of previous education, though some held master’s MOCK TRIAL METHOD 25 degrees and one student completed doctoral coursework. Instructors guided students each step of the way from topic selection, literature search, critique, best practice recommendations, design, implementation, and evaluation. Outcomes were measured through focus groups evaluated by collecting data using semistructured questions, values and attitudinal aspects of EBP rated on a performance scale, and student self rating on their ability to develop a clinical problem statement, retrieve, critique and synthesize evidence, and write an EBP protocol. Mean scores were 8.91 (SD=0.087) for knowledge of the meaning of evidence and EBP; 9.36 (SD=1.05) for belief in the value of EBP, 8.45 (SD=1.14) for ability to identify a patient problem, 7.36 (SD=1.53) for competence in critiquing evidence, 8.50 (SD=1.22) for identifying gap in literature and practice performance, 7.50 (SD=1.95) for readiness to implement in practice, 6.0 (SD=2.39) to identify change process using change model, 6.36 (SD=2.28) for adaptation, design, and implementation of a change process, 6.68 (SD=2.82) to describe and implement evaluation of change, and 6.86 (SD=2.61) for developing a way to maintain and improve change over time. Instructors and students reported high confidence levels in the experience and in the collaborative process. Clinical nursing staff felt more connected to the students’ learning experience and the EBP project. Collaboration and engagement of all key stakeholders helped students effectively translate knowledge into best practice at the bedside. Mock Trial / Role Play / Simulation For all intents and purposes, the mock trial method can be considered a dramatic simulated role-play. Types of role-playing scenarios differ depending upon the subject matter to be taught, however the experience has the potential to transform theoretical concepts into an experiential framework. Clinical simulation has been recognized as a teaching method using MOCK TRIAL METHOD 26 learning exercises that closely mimic real-life situations with student immersion in a representative patient-care scenario that mimics the actual environment with sufficient realism to allow learners to suspend any disbelief. (Waxman, 2010) In support of using a mock trial as an effective methodology for teaching EBP, few articles have been written and of those published, there was reassuring validation for the effectiveness of this approach. Mock trials have been used as an educational tool for many years to teach law students how to prepare for actual litigation in the judicial system. Its popularity spread to teaching students of all ages in a variety of other subjects and professions. Specific to the practice of nursing, the mock trial approach has been used as an innovative way to teach standards, policies, compliance, critical thinking, reasoning, decision-making, and legal documentation in the healthcare profession. (Biddinger, 1999) The added benefit of teaching the legal liability in relationship to practice supports good documentation. Jenkins and Lemak (Jenkins, 2009), emphasize the effectiveness of a mock trial simulated role-play approach to teach nurses how the legal system can scrutinize their clinical decision-making as nurses’ documentation of the ‘facts’ of the case drives the strength of a lawsuit in court. The mock trial also emphasized the importance of following standards of care and documentation of such in the medical record. A simulation of a critical care lawsuit was conducted for the critical care team and included each member taking an active role in the case and participating in the post-trial debriefing and discussion. The course was done in two sessions with the first session introducing basic legal concepts that apply to healthcare, the facts of the case, and the role-play simulation. The second session was the actual mock trial, jury verdict, post-trial debriefing and discussion. MOCK TRIAL METHOD 27 Using a likert scale of 1 (disagree) to 5 (agree), formal, written evaluation from 20 participants revealed extremely positive experiences overall for instructional method, effectiveness of presentation, content, and objective achievement. Qualitative data further validated the successful experience through comments such as, “every employee should have to go through this great learning experience as the simulation was an excellent way to instruct and an extremely useful way to learn,” and “as my peers role-played their assigned tasks, an incredible learning experience was unfolding for everyone involved.” This mock trial experience reinforced the principle that one of the best ways to learn, digest, and remember material for participants from different roles, training, and experience backgrounds is by applying such in a hands-on simulated environment. When reinforcing a policy or procedure that can be fairly dry when presented via the traditional teacher-centered approach, it is helpful to use a mock trial that involves the learner as active participant. This simulated role-play student-centered approach requires the learners to be involved in their learning process and emphasizes adult learning and critical thinking concepts. (Billings, 2005) Billings also reported that using real-life scenarios increases retention of knowledge, and practicing in a safe environment is advantageous to learning. Staffileno and McKinney used the mock trial to demonstrate evidence–based nursing practice and how to incorporate into clinical decision-making. (Staffileno, 2010) The event was held in a large hospital auditorium for approximately 100 employees. Staff nurses engaged in the role-play experience and the jury was selected at random – twelve audience seats had envelopes taped under the seats with juror instructions enclosed. At the conclusion of the trial, educators collected post-trial qualitative questionnaires and conducted a debriefing. Among the themes from the attendees were: the quality of the presentation kept the audience captivated; the MOCK TRIAL METHOD 28 importance of using the best available evidence for clinical practice was highlighted; and the quality and effort put into launching the presentation were positively reported. Teaching with an Automated Response System Patterson, et al (2010) reports that with increasing classroom sizes, active student participation and engagement is key to learning effectiveness. This study was a quasiexperimental comparison of nursing students enrolled in a medical/surgical course. One section used an audience response system (ARS) and another section of the same course did not. Students independently registered for the course sections and did not know in advance there was a difference in instructional techniques. While not a random assignment, participants were not screened in or out of the study – all participants in both sections were automatically enrolled as a convenience sample. The total number of students enrolled in the study was N=70. There were n=38 students in the experimental group and n=32 students in the control group. The same faculty member facilitated both sections and taught the same content.. Students in both sections completed the same pre test, unit tests, and final exam. Throughout the course, a variety of knowledge-based to analysis level questions were posed to the students. While control group students were verbally asked questions by the faculty verbally and answered via the traditional ‘hand raise’, the experimental group had the questions integrated into a power-point presentation and answered via ARS technology (hand held “clickers”) where a histogram immediately displayed participant responses. Focus groups were conducted with the experimental group and asked questions such as: 1. What were the strengths of using clickers in the classroom? 2. What were the limitations of using clickers in the classroom? 3. How did the clickers influence your learning of the course content? MOCK TRIAL METHOD 29 Generally, students perceived the clickers as “fun” and they “looked forward to it.” Three themes emerged from the focus groups. The first theme was ability to respond anonymously and was preferred to other methods such as having to raise your hand and risk being ‘wrong’. The second theme was receiving validation of an answer through immediate feedback that confirmed and clarified understanding of specific content. The third theme was provision of an interactive and engaging environment -- students felt use of clickers gave them something to do and they perceived this interaction brought them closer with other students through the interface of technology, student, and faculty. Quantitative analysis did not demonstrate any significant differences between sections even though the groups were similar in demographic and attribute variables. T-tests revealed no significant differences between groups on any measure of outcome performance. Although this study did not reveal improved learning outcomes, perceptions of student participants indicated increased classroom engagement. A review of the literature by Mareno, et al (Mareno, 2010) reported the use of the ARS as an active learning strategy in nursing education that allowed for the dynamic engagement of students through immediate two-way communication with faculty. This type of learning acts as a springboard for discussions and subsequently used for further verification, clarification, and amplification as indicated from responses. The authors’ findings identified themes in the evaluation literature, highlighted gaps in the literature as it pertained to evaluating the effectiveness of using simulations as a teaching tool, and supported the need for further research into the evaluation of simulation as a teaching tool. The review of literature revealed the effectiveness of simulation, role-play, interactive learner participation in activities, use of polling with audience response systems, and innovative MOCK TRIAL METHOD 30 approaches such as mock trials. These were the key elements that influenced the intervention design of a mock trial learning event at the local area trauma center. SECTION III In keeping with the goals of the project to establish a fun, innovative, and engaging day for the nurse participants and convey a relationship between nursing practice, EBP, documentation, legal implications, and patient outcomes, as well as reinforce previous learning regarding the evidence-based POSS opioid sedation scale, the work of creating the evidence through testimony was in order. The organizational Institutional Review Committee (IRC) determined this performance improvement project did not require committee approvals so full board review was waived. Refer to Appendix C for IRC submittal documentation. Development of the Mock Trial Case & Script Pre-trial preparation began months in advance of the scheduled event to allow for time for case selection, development of the facts, character briefs and role assignment, literature review, script writing, along with consideration and provision for drama, controversy, scholarly discussion and analysis in preparation for the deliberation process. The most important part of the trial was to provide clear evidence and persuasive arguments for the respective opposing position. Neither acting ability or the simulated courtroom scene were on trial – fun and enhanced participant engagement were paramount. In order to keep the case applicable to the nurse learners, the creation of a patient scenario was one that was relevant and routine in nursing practice so the outcome (death) would be unexpected and thus provoke a compelling critical examination of the root cause(s). The case that would ‘go to trial’ was one of a 42-year-old obese male patient, Mr. C., admitted for right total knee arthroscopy. This young and previously healthy individual would be transferred to a MOCK TRIAL METHOD 31 medical/surgical unit post operatively, receive patient controlled analgesia infusion of Dilaudid to control pain, experience severe respiratory depression, subsequent respiratory failure and death following failed code resuscitation attempts. This heretofore ‘-routine’ surgical case was one that most nurses could relate to, even if they did not typically care for this patient population. The non-routine part of the case, i.e., the unexpected outcome, was intentional in design to help nurses identify with best practices and evidence in support of appropriate assessment, management, and monitoring of the ‘routine’ case high alert medication (opioid) being infused through the self administered parenteral route. In addition, in order to make this case ‘negligence’ and not ‘malpractice’, focus had to be placed on the nurse, not the physician, in meeting or not meeting the standard of care based on the best evidence for quality and safe patient care. Negligence is defined as conduct that is culpable because it falls short of what a reasonable person would do to protect another individual from foreseeable harm. (U.S. Legal Definitions, 2012) The four elements of negligence that must be proven are: 1) Duty to treat – the legal duty that exists whenever a hospital or healthcare provider undertakes care or treatment of a patient. 2) Breach of duty - failure of a hospital or healthcare provider to conform to the relevant standards of care; the standard of care is proven by expert testimony or obvious errors. 3) Causation – the breach of duty was the proximate cause of harm. 4) Harm – the negligence must be the proximate cause of harm. These elements were used as the platform to elucidate the unfolding evidence and fact base of the case and are further summarized below. MOCK TRIAL METHOD 32 Professional Duty In order to establish a shared meaning of professional duty, the first part of the seminar day was dedicated to subject matter expert presentations on a review of professional role, responsibilities, nursing scope and standards of practice, evidence-based practice, and the link to accurate and comprehensive documentation. Breach of the Standard of Care Through the course of treatment and care of the fictitious patient, it was essential that the ‘facts’ in the script addressed whether the standard of care was met or not. It was determined the issues to be highlighted and called into question through persuasive attorney arguments and banter followed the steps and rules of ‘evidence’ for trial experiences. (Appendix D) The issues are summarized below along with the persuasive attorney arguments and banter that made for good drama and fun. The issues brought forth in the trial also answered the PICO question (Table 5) when addressing the ‘evidence’ through use of ‘expert’ testimony and inclusion of evidence based practice verses expert opinion arguments. Table 5. The Five Steps of Evidence-Based Practice (Melnyk, 2004) 1. Ask the clinical question in PICO format to yield the most relevant and best evidence. P: Patient population of interest I: Intervention or issue of interest C: Comparison of interest O: Outcome of interest 2. Collect the most relevant and best evidence to answer the clinical question, searching first for systematic reviews, meta-analyses, or evidence-based clinical practice guidelines. 3. Critically appraise the evidence that has been collected for its validity, relevance, and MOCK TRIAL METHOD 33 applicability. 4. Integrate the evidence with one’s clinical expertise, an assessment of patient characteristics and healthcare resources available, and patient preferences and values in order to implement and evidence-based practice decision. 5. Evaluate the evidence-based practice change. Expert opinion and EBP were actively debated during the discussion with expert witnesses related to a research article concerning the specific orthopedic patient population and post surgical pain management with infusion of PCA opioid medication. (Brown, 2005) The research question is described in the PICO format below: P: Patient population of interest - post operative patients receiving opioid Patient Controlled Analgesic (PCA) intravenous infusions for pain management. I: Intervention or issue of interest – implementation of the POSS sedation scale. C: Comparison of interest – use of other scales as compared to the POSS for assessing, monitoring, and managing advancing respiratory depression O: Outcome of interest – early detection and intervention as best practice to avoid advancing sedation and ensuing respiratory depression. According to standard practice respiratory risk precautions, the patient in the unfolding mock trial case was opioid naïve, however documentation of this was lacking; arguments were built around if this assessment occurred at all and if risk precautions were implemented. To build upon the ‘breach’ in the standard of care in the case, the PCA was set for continuous basal infusion plus demand dosing which was not an appropriate rate for Mr. C’s respiratory risk factors. The patient rated his pain as 6/10, which was considered ‘moderate’ according to the MOCK TRIAL METHOD 34 pain scale used; however the nurse administered the dose ordered for ‘severe’ pain instead. The handoff report from the off-going to the oncoming nurse was not complete and did not include the standard of care and best practice of ‘in the room’ independent verification of pump settings for ‘high alert’ medication infusions. The early indicator of respiratory depression, sedation level was not documented as being monitored. The developing facts and controversy in the case were created to lead patterns or trails of evidence that a jury or trial could understand, debate, question, and consider. As the case took form, particular issues or ‘arguments’ of the case emerged and scripted as facts in order to create controversy to both convince and dissuade the jury to consider proximate cause/harm. Proximate Causation / Harm The dosage order for Dilaudid at 0.4mg to 1mg was too high for a patient who was opioid naïve – it should have been 0.4mg to 0.6mg and the nurse did not document or challenge this order with the physician. Mr. C. developed increased sedation with PCA plus continuous basal rate plus IV bolus – an inappropriately high dosage for his high-risk status, failure to place the patient on respiratory risk precautions, monitor and manage Mr. C. as best practice indicates, and without supporting documentation, it would be up to the Plaintiff’s attorney to prove all these actions and non-actions led to the increasing respiratory depression, failure, code and subsequent death. A brief outline of the plaintiff and defense opposing and supporting attorney views to be proven in the courtroom are listed in Table 6 below. MOCK TRIAL METHOD 35 Table 6. Opposing and Supporting Attorney Cases Plaintiff’s case The plaintiff will try to prove: Nursing negligence was the direct cause of harm (death) Patient received a ‘overdose’ of Dilaudid PCA Nurse failed to recognize patient was opioid naïve Nurse administered high end dose of opioid medication instead of starting with the lower end of the range order. Respiratory risk precautions were not implemented to protect the patient from harm. Defendant’s case The defense will try to prove: Nurse met the standard of care Nurse exercised sound judgment and EBP in her assessment and care of the patient based on nursing scope and standards of care and the BRN best practice guidelines on pain management. Nurse did what any reasonable and prudent nurse would have done given the same set of circumstances. A bad outcome alone is not evidence of negligence; the patient’s outcome was a tragic and unexpected response to a commonly used medication. The script evolved around all these issues as the fact patterns expanded and employed standard legal ‘evidence’ rules with interposing attorney objections, irrelevant evidence, leading questions, and hearsay to spice up the dialogue. Pro and con persuasive controversy was incorporated as ‘facts’ to compel participants to listen intently as evidence patterns evoked reflection and consideration for the jury. Expert witnesses debated the best evidence for opioid naïve assessment, monitoring and management based on the latest research and best evidence in the management of pain for patients receiving opioid infusions. Other disciplines were recruited to fill vital roles of the bailiff – a retired police officer; an expert pharmacist – director of the pharmacy; and a nurse attorney played the role of the judge. Character briefs for each role in the case were crafted and these profiles guided the respective and lively trial ‘performances.’ (Appendix E) The script (Appendix F) was finalized with all MOCK TRIAL METHOD 36 pertinent issues concerning the patient’s current and past medical condition, hospital course, lab tests, physician orders and nurses’ notes synthesized as ‘exhibits’ (Appendix G) for the benefit of judge and jury. The script followed the steps of trial procedures to include beginning with opening statements, defense call for the witness first, then the plaintiff attorney can decide to cross-examine. The judge decided the validity of objections, outbursts, etc. Expert testimony from both plaintiff and defense were laced with expert opinion verses research and evidencebased practice and designed with intent to give rise to scholarly discussion during the jury deliberation phase as learners familiarized themselves with the new sedation scale, policy, procedures, and best practices in monitoring and managing this at risk population of patients. See Table 7 for the basis of the opposing and supporting controversy and arguments presented during the trial. Table 7. Opposing and Supporting Views Issue Plaintiff’s Argument Defense’s Argument Handoff Report Handoff report occurred at The nurse was not given shift change as per policy an adequate handoff report and included standard to inform accurate SBAR components. stability of patient status. Independent verification / signatures Standards of Care and Practice / EBP No documentation of 2nd nurse independent verification of pump settings for high alert medication at shift change, therefore it did not happen. The patient rated his pain as 6/10 and is ‘moderate’ according to the pain scale, however, the nurse administered the dose for ‘severe’ pain. Newly recommended Independent verification was conducted but not yet documented due to the patient’s complaint of ‘severe’ pain and nurse’s goal to relieve pain. The California BRN guidelines state that pain be assessed and treated promptly and effectively for as long as the pain persists. BRN guidelines further state: MOCK TRIAL METHOD 37 Table 7. Opposing and Supporting Views Issue Plaintiff’s Argument Defense’s Argument opioid dosing orders The RN is encouraged to decreased patient risk. use his/her nursing Strategies to reduce risk: judgment and give Independent verification patients routine and by two RNs, line consistent pain medication reconciliation, smart pump within the first 24-48hrs technology. after surgery. Pain management in order of importance is: Patient’s self report. Recent EBP article: clinical or statistical significance – findings inconclusive. Opiate Naïve Patient Assessment PCA Infusion with high alert medications Assessment of the opioid naïve patient was not documented therefore, was it done? The nurse mistakenly believed that the patient’s symptom of snoring was a sign of pain relief instead of a warning sign for impending respiratory failure. Patient’s wife stated that he snored at home. Patient should have been placed automatically on respiratory risk precautions. Initial opioid IV infusion dose PCA plus basal-/ rate was too high for opioid naïve patient. Nurse did not question the Assessment was done but not documented because the goal was to relieve the patient of his stated “severe” pain at the time he reported it at change of shift. Snoring in and off itself does not lead to fatal consequences. Respiratory rate is known to be an unreliable indicator of the presence or absence of respiratory depression. Clinical experience with this patient population suggests the majority of opioid naïve patients can be very tolerant and not MOCK TRIAL METHOD 38 Table 7. Opposing and Supporting Views Issue Plaintiff’s Argument Defense’s Argument high initial orders but have adverse effects. knew it was on the high MD orders were range. (0.2-1.0 mg IV Q2h considered as well as for pain) individual patient When written as range diagnosis, co-morbidities, order – nurse must begin and pertinent medical at the low range and titrate history that may affect up as needed. drug metabolism. Nurse used good clinical reasoning and individualized care. There are constantly changing approaches to pain management. Hourly Rounding Nurse failed to check on the patient within the prescribed one hour of intervention to determine response and respiratory rate. PCA by Proxy Patient and family education – testimony by the patient’s wife revealed she was pushing the PCA button to “help” her husband who was in pain. Did the nurse provide education to the patient and family? No evidence in the documentation that patient / family teaching was Initial assessment with patient exhibiting several signs of ineffective pain relief. Priority was to obtain and administer pain medication. Patient was seen by either the RN or CNA every 1020 minutes throughout specified time frame. Patient and family education included use of the PCA button and not to use by proxy – this is also clearly labeled on the button itself. Patient’s wife disregarded label and covertly admitted to pushing the button herself to try to relieve her husband’s pain. MOCK TRIAL METHOD Table 7. Opposing and Supporting Views Issue Plaintiff’s Argument done. Sedation Scale Use of the opioid sedation scale – did the nurse use the POSS scale? If not, why not? What was the nurse monitoring – respiratory rate or sedation scale? No documentation of sedation level. Reversal Agent Over-sedation was not recognized nor treated immediately according to best practice guidelines. 39 Defense’s Argument Did not use it immediately because the patient exhibited 8 out of 10 signs and symptoms of uncontrollable pain and policy supports immediate intervention for severe pain. Nurse stayed WITH the patient to immediately perform CPR; the nurse would have had to leave the room in order to retrieve med so she cared for the most immediate needs first. The Trial – the ‘transformed’ classroom The day unfolded to a packed auditorium of over 150 registered nurses. Upon entry into the auditorium, participants were handed the agenda along with the electronic ‘clicker’ ARS device for polling of demographics and participant knowledge of evidence-based practice issues to be covered in the trial. The clickers would also to be used by participants to register the final verdict at the end of the trial. The beginning of the day was carefully crafted with subject matter experts providing a review of the nursing practice act, scope and standards of practice, chain of command, evidence based practice, legal implications of documentation and a brief presentation on the basics of what to expect during a courtroom trial. (Appendix H) This content was essential to establish clear guidelines for ‘juror’ participants to evaluate nursing practice, patient MOCK TRIAL METHOD 40 care, documentation, and all evidence presented during the trial that would be conducted in the afternoon and designed through Kolb’s (Kolb, 1984) organizing framework. Beginning with the review of the nursing role and practice standards was intended to guide individuals in a concrete way bringing the abstract and theoretical concepts and models into context through dialogue, drama, engagement, and self-reflections in the intentional learning environment. Members of the jury were given a notebook that contained all the evidence presented in the trial and a deliberation worksheet (Appendix I) to record notes on their thoughts and findings throughout the day. They were instructed to pay close attention to the evidence presented throughout the trial and make notes on their deliberation worksheets as the outcome would depend upon them after carefully weighing the information presented designed to influence the final verdict. The trial session ensued in the afternoon when the ‘courtroom’ came alive with judge, jury ‘box,’ bailiff, plaintiff and defendant attorneys carefully arranged on the auditorium stage and with expert witnesses covertly embedded within the audience for an added element of surprise when called to testify. Evidence was presented in the dramatic simulated role-play scripted scenario equipped with the cast presenting in full dress and role characterization. The judge entered the courtroom with black judicial robe regalia to the booming voice of the security guard clad bailiff bellowing out “ALL RISE”. The plaintiff’s attorney was pretty in pink as the Elle Woods fashion icon character of the Legally Blonde movie fame – complete with ‘yapping’ miniature dog in pint sized carrier which she positioned high atop the attorney’s desk so all could see. The wife of the deceased patient was the plaintiff and she was believable as a woman in her final trimester of pregnancy – complete with belly pillow - and extremely emotional with outbursts of uncontrollable weeping and hankie tossing throughout the role-play. MOCK TRIAL METHOD 41 The defendant’s attorney was dressed in a more serious minded two-piece business suit and maintained a steady poise during the entire debate. The nurse defendant was similarly convincing as an authentic and caring experienced clinician, who maintained credibility in establishing her knowledge, experience, and competence. One nurse expert witness was dressed in stereotypical scholarly fashion with hair pulled back and glasses slightly tipped on her nose looking down condescendingly at everyone. Another nurse expert witness was portrayed as an over-confident experienced nurse clinician who claimed value in evidence-based practice however, she felt the real world value of expert clinical practice could be more valid and valuable than the best nursing research. The expert pharmacist stayed the course and stuck to ‘just the facts,’ as it related to pharmacology science and the latest and best literature. All courtroom exhibits were shown on the projection screen in the center of the stage so the nurse ‘jury’ participants could see the evidence as it was entered into testimony. The addition of humor with role characterization and realism in the courtroom scene with judges’ bench, jury box, attorneys’ desks, a daunting bailiff swearing in each of the witnesses and calling out directives from the judge for ‘‘order in the court’’ along with elements of surprise and uncertainty, all encouraged an appealing and fun learning atmosphere which begged participants full and captivating engagement. At trial conclusion, the judge gave instructions to the jury concerning deliberations. The judge then exited the courtroom and participants were asked to divide into twelve groups of 1215 participants each, and then given 45 minutes to deliberate. Each group represented the vote of one juror, and the majority vote within the group (50% plus 1 = majority) would be the final decision to be registered via ARS. Groups engaged in active and lively discussions regarding the MOCK TRIAL METHOD 42 content and context of the trial and its relevance to the ‘evidence’ presented. The auditorium was buzzing with dynamic, informative, and appealing scholarly dialogue. At the end of the deliberation period, the ‘judge’ re-entered the courtroom and asked the jury ‘foreman’ for the final verdict. For dramatic effect, the jury foreman handed a (blank) card over to the judge representing the jury’s decision at the same time the votes were being registered electronically. Each group entered their final vote –one vote per group. The final verdict was 10 to 2 in favor of NOT NEGLIGENT. Once the verdict flashed upon the projection screen there was an audible, collective exhalation from the crowd with mixed emotions of surprise, sadness, and relief. It was clear that the audience was deep into the realism of the experience and the verdict represented each participant’s personal resolution and reflection on the case. SECTION IV The pre and post survey questions tailored towards collecting demographics from the participants through ARS polling survey were displayed at the front of the auditorium onto the projection screen. Pre survey polling conducted to the beginning of the seminar included questions regarding both demographic and evidence-based practice content while post survey polling was conducted immediately after the seminar and included only the evidence-based practice content. The abbreviated survey content is listed below and the full questionnaire can be reviewed in Appendix J. Demographics Survey Poll o Current role (RN, CNA, Academic Clinical Faculty, etc.) o Area of work (acute care, skilled nursing, outpatient, home health, academic, other) MOCK TRIAL METHOD 43 o Specialty area (medical/surgical, critical care, surgery, case management, ED, OB, other) o Years worked in the healthcare field (from 0 to over 20 years) o Entry into practice education (Diploma, ADN, BSN, MSN) o Highest level of education (Diploma, Associates, Bachelors, Masters, Doctoral) o Currently hold a national certification (yes or no) Evidence Based Survey Poll o Definition of an opioid naïve patient. o Recommended starting dose of opioid infusion for an opioid naïve patient. o Likelihood of PCA administered opioid medications to cause respiratory depression than other means of administering these medications. o Respiratory rate as a reliable indicator of the presence or absence of respiratory depression for patients on opioid IV infusions. o Risk factors / conditions that patients may be considered at higher risk for respiratory depression when placed on an IV opioid infusion. Demographics polling revealed ninety seven percent of participants were registered nurses working in an acute care setting with the majority working inpatient medical/surgical divisions and next highest representation was nurses working in the specialty divisions of critical care and emergency services. Sixty three percent had twenty years or greater of nursing experience; fifty percent had earned a bachelor of science (BSN) as their entry into practice degree, thirty one percent were associate degree nurses. There was a thirteen percent increase in BSN and over forty percent increase in masters of science in nursing (MSN) since initial practice degree, with sixty five percent holding national certifications. The characteristics of this population MOCK TRIAL METHOD 44 represented a well-educated and clinically experienced group of ‘jurors’ that had advanced their education from their initial entry into practice degrees. Pre conference questions regarding knowledge base of the topics included in the trial revealed an overall average of fifty percent correct responses from all questions asked. This was the baseline from which learning would be measured at the end of the day. As the final order of the day, post-test questions – the same as pre trial -were then queried to substantiate an impact on learning. Of the six questions surveyed, the majority of participants scored fifty percent correct pre conference and one hundred percent correct post conference. Interestingly, there were two questions participants were still unclear on post trial and those questions contained the most emphasized controversial issues in the trial. Though intended mainly for controversy, these issues presented during the trial as literature reviews and evidence were debated as too small of a sample size to yield convincing results. The same survey questions were distributed via electronic survey polling six months post seminar to evaluate for sustaining the gains. A total of thirty-seven participants responded to the six-month survey, a majority of who were medical/surgical inpatient nurses with BSN degrees as their entry into practice education. Ten nurses advanced further professionally from their entry into practice education to either a BSN or MSN degrees. Twenty-five nurses held a nationally recognized certification. This sample was well educated and representative of the larger audience that attended the seminar. All responses were correct except the two questions that posed the greatest amount of controversy during the trial. Participants paid particular attention to these evidence-based issues equally weighted with supporting and opposing arguments threaded throughout the trial as attested by their conflicted responses to the post conference questions – MOCK TRIAL METHOD 45 this could also be considered a very convincing case of the impact of learner engagement. Polling outcomes have been graphed for easy viewing in Appendix K. At the end of the seminar day, an open microphone session ensued to give the ‘jury’ or participants an opportunity to cite the evidence that influenced their decision and tipped the scales of justice one way or the other. Resulting dialogue was rich with enlightened acumens about the value and legitimacy of the evidence presented which then sparked more debate. The auditorium was once again buzzing with dynamic, informative, and appealing scholarly dialogue within the larger, all-inclusive assemblage. During this final interchange, there was overpowering agreement there was not enough ‘evidence’ in the documentation to reach a verdict of NEGLIGENT although the case was noticeably ‘convincing’ in its relevance and authenticity. Time was set aside for the participants to debrief the ‘mock trial’ approach for learning, the advantages and disadvantages of this type of learning, if the trial and witnesses were believable, and if anyone made up his/her mind during the trial itself or during deliberation process and, if so, what was it about the process itself that swayed their thinking. Overwhelmingly, responses yielded in favor of this learning approach with “interactive,” “relevant,” and “engaging” as common replies. Participants loved the case, the learning approach, the witnesses, plus the drama and humor. The nurses liberally articulated the strong and weak arguments presented during trail from each side of the bench and any additional information that might have been helpful to include. All comments were directed toward the fact that they required more evidence in the patient’s medical record in order to give credence to the argument that the nurse did or did not practice to the standard. It was this ‘lack of evidence’ that participants remarked tipped the scales, as there was not enough conclusive evidence to convict. Lack of this conclusive MOCK TRIAL METHOD 46 documentation was an intentional design feature to challenge participants’ connection to the importance of practice performance validation through documentation. The substance of the conversation and the questions posed provided evidence that the nurses made this connection. The standard written class evaluations were useful in capturing the thoughts on the full immersive experience of the day. A preponderance of affirming comments reflected the effectiveness of the learning for the jury participants such as: “the mock trial was thought provoking” “the speakers were inspirational and validated nursing as a scientific profession” “the mock trial was a well planned and thought out presentation” “this reminded me that practice can always be improved by utilizing my ideas or perspective and moving further to research and implementation” Other statements concentrated on what was most valuable to the participants such as learning the relationship between patient care, safety, quality – critical aims of the IOM report (Institute of Medicine, 2003), and the importance of connecting the documentation that reflects evidence of the care that was given as well as the importance of lifelong learning through research. (QSEN, 2012) (American Nurses Association, 2010) These results also reinforce the Learning Pyramid model that affords the case for active, participatory learning involving every part of the senses. (NTL Institute, 2012) Outcomes are summarized through the PDSA model for rapid cycle improvement. During the ‘Plan’ part of the cycle, the focus of the learning was centered on improvement in the early identification of advancing sedation and interventions to decrease sedation levels. The main ‘target’ audience was acute care nurses and the subject matter was the reinforcement of the POSS sedation scale, current process and standards of care, practice, and documentation. MOCK TRIAL METHOD 47 Identification of the root causes for advancing sedation was lack of standardized tools and evidence-based practices along with the increased rates of reversal agents administered was also discussed and debated in the role-play scenario. Pre and post measures used trial scenario content related to the POSS scale and the value of evidence-based practice and showed a positive relationship in achievement of learning. The aim in the seminar and trial content was to help nurses identify the root cause of advancing sedation with EBP and best practice protocols, standards of care, and enable early detection and intervention through use of the POSS scale tool; this was accomplished. The ‘Do’ phase of the cycle was the implementation of the all day education seminar using the mock trial method. This included content that outlined the scope and standards of professional nursing, the value and legitimacy of evidence-based practice, legal documentation, and the basics of trial proceedings. The ‘Study’ phase included both written and ARS survey evaluations and polling results– immediately pre and post program that validated enhanced learning. The ‘Act’ phase of the cycle included a process to monitor the gains. Retention of learning was measured at six months using a survey that included the same questions used in the pre/post program, and an audit of the incidence of reversal agents administered for respiratory depression from advancing sedation. (Figure 5) There was a five-fold reduction in use of reversal agents during the 12-month period following the mock trial. 48 Number of Incidents MOCK TRIAL METHOD Incidents of Narcan Sedation 15 10 5 0 NARCAN/SEDATION 2010 11 2011 2 Figure 5. Incidents of Narcan Reversal Agents Given for Advanced Sedation of Medical/Surgical Patients The gains in knowledge were sustained with subsequent practice change as evidenced by reduction in use of narcan reversal agent for advanced sedation in medical/surgical agents. Level 1 Hierarchy for Evidence-based Medicine Teaching and Learning Experiences (Table 1) was operationalized in the interactive and clinically integrated mock trial approach. Sustainability over time was realized as evidenced by improved patient safety and quality outcomes through organizational efforts in continuous monitoring of patient safety and quality outcomes. SECTION V Discussion The aim of this project was centered around enhanced education that would provide nurses with information to identify advancing patient sedation using the POSS sedation scale as a best practice and standard of care, thereby enabling early detection and intervention. Project goals were geared toward 1) establishing a fun, innovative, and engaging educational day for nurse participants, 2) designing an integrated practice, documentation, legal implications, and patient outcomes scenario, and 3) reinforcing previous learning of the POSS sedation scale. Outcome results obtained through pre and post survey polling support the case for realization of MOCK TRIAL METHOD 49 these goals through the mock trial experience and aligns with the grounding and theoretical framework in the following ways: Quality and Safety Education for Nurses (QSEN): addresses the challenge of preparing future nurses with the knowledge, skills, and attitudes (KSA) necessary to continuously improve healthcare quality and safety. Kolb’s four-stage learning cycle illustrates how this experience is translated through reflection into concepts, which in turn are used as guides for active experimentation and the choice of new experiences. (Kolb, 1984) o The Do It or Concrete Experience stage, where the learner actively experiences an activity such as a lab session or fieldwork – accomplished in this project via the mock trial courtroom simulated role-play experience. o The What Happened or Reflective Observation stage, when the learner consciously reflects back on that experience – this occurred through the ‘deliberation’ phase of the trial where the participants engaged in active learning through reflection on key points brought out during the trial. o The So What or Abstract Conceptualization stage is where the learner attempts to conceptualize a theory or model of what is observed – this was via the staff development continuing education program focused on the foundations of nursing scope of practice in order to establish the basis from which to critically evaluate it. o The Now What or Active Experimentation stage, where the learner is trying to plan how to test a model or theory or plan for a forthcoming MOCK TRIAL METHOD 50 experience – accomplished at the end of the trial when participants engaged in deliberations and ‘open microphone’ sessions to articulate their intellectual reasoning and decision making, nursing theories, and assumptions drawn from the trial case and application to daily practice. The additional measure of success was the enrichment of the participants desire to learn and value their practice through reflection, critical thinking, and clinical inquiry that was articulated through verbal and written evaluation. The need to supplant traditional instructor-centered efforts for more non-traditional, interactive approaches centered on the learners, not the educators, has been demonstrated and validated through historic and current literature. The teaching of evidence-based practice requires a specific approach to learner engagement through values-driven, intrinsic motivation as expressed in Wlodkowskis’ work (1999) – the inclusion environment or courtroom experience to connect the instructor with the learner; the attitude or disposition to establish relevance otherwise known as the ‘routine’ nursing practice issue; the meaning that challenges the learners existing values or the ‘doubt’ and ‘controversy’ expressed in the role-play; and finally the competence of the experience that engages learners to connect the content as added value to their practice through the foundational didactic content: standards of practice, evidence-based practice, documentation, and legal implications in relationship to the experiential role-play associations. These associations reinforce that instructional strategies can be designed to invite the learner ‘in’ to the learning environment in order to enhance the value of the learning experience. Effectiveness of the learning experience begins with the instructors understanding that all students have different strengths and needs. The design of this program was based on best educational practices and the assessed needs of the nurse participants with the understanding that MOCK TRIAL METHOD 51 there are some basic learning needs that are shared by all students as evidenced by adult learning theory, learning pyramid, and socio-cultural based teaching strategies (Table 4) (Bonk, 1998) used in the role-play. This approach provided the platform for the adult nurse learners to not only engage with the subject matter and experience it, but to also engage with their colleagues regarding their shared values in nursing practices. Adult learning theory submits that learners have a desire to become better at what they do and this becomes more apparent when it has relevance to their profession. Nurses and all adult learners can experience professional and academic growth given the right guidance, information, and tools in order to improve. Even if the platform is not well managed, effective learning can still take place. A simulated role-play environment cannot be fully scripted when learners are expected to respond in real time to the experience, both failures and successes must be allowed to unfold. Doing so creates opportunity for instructors to model patience, calm and logical thinking to resolve difficult situations demonstrating that mistakes are not disasters; they are opportunities for discovery and redirection. The limitations of this teaching and learning methodology are long-range sustainability. New knowledge and skills are difficult to maintain and have a tendency to erode over time. Thus, instructor and learner vigilance to the KSA of the learner is essential. There are limited comparative studies specific in teaching evidence-based practice to nurses using the mock trial method. Additional studies such as this are needed to further develop this body of knowledge. Generalizability to the nursing population at large is cautionary due to the study’s fairly homogenous sample size (80% employees are from the same organization) and the inherent lack of design rigor. Transferability can occur as the elements of national standards and grounding frameworks of the project design have been widely used, accepted, and validated. MOCK TRIAL METHOD 52 Studies have demonstrated positive benefits of using a mock trial approach, including enhanced critical thinking and reasoning, team building, understanding of standards of care in everyday practice settings, along with an awareness of the legal implications of clinical documentation. Transferability is cautionary as well, since not all organizations operate from the same type of patient safety and quality structures, processes, and outcomes monitoring, management, and enforcement of best practices that were inherent to this environment. Implications for nursing practice The mock trial approach provided an opportunity for practical appraisal of complex concepts more readily than other types of pedagogical approaches that had been used previously within this organization. It accelerated the learning process in a short period of time. It assisted participants to link theory with practice, encouraged discovery of new knowledge, allowed for participant self-reflection and created the environment for participants to understand the content and then synthesize, analyze and incorporate such into a scholarly context. Innovative teaching and learning strategies can be adopted and adapted to deliver education that effectively supports best practice and influences practice performance. Regardless of the subject matter taught, incorporating innovative, interactive, and engaging educational programs is effective in achieving learner engagement, knowledge retention, and real-time application of learned concepts. Active learning stimulated interest and inquiry leading to a better understanding of the requisite content. Instructor and students became partners in approach rather than the learner being ‘captive’ at the hands of the teaching experience in and of itself. Other critical success factors were support from nursing leadership, enthusiasm and engagement of the Shared Governance Council, adoption of the role-play concept by ancillary staff players, and preprogram marketing through positive word of mouth and creative newsletter MOCK TRIAL METHOD 53 advertising. Subsequently, this approach has been integrated into the organizations’ transition program for new graduate nurses, was presented in another organization, and this author was selected as ‘finalist’ for the California region of the 2012 Gannett Healthcare Group Nursing Excellence Awards , in the Education and Mentorship category. (Nurse.com, 2012) The reader can benefit from the strategies discussed within the body of this paper to design an educational experience with unique and inherent qualities that will engage nurses in transforming care at the bedside in a participatory learning environment. Conclusion Many factors contributed to the success of an innovative method to address learning needs on multiple levels and transference of learning to actual nursing practice. On the day of the educational experience, the laying of the groundwork early in the day with the essential foundations of practice obligations, nurse participants were prepared to evaluate the unfolding courtroom drama in the afternoon. Through the trial enactment and ensuing juror deliberations, participant jurors became involved in a fun, challenging, and engaging way of learning to substantiate their practice through a tangible application of complex and abstract principles of law applied to healthcare. There was an increase in knowledge as evidenced by the percentage of correct responses post trial on questions related to the new sedation scale and critical elements of assessing and monitoring patients receiving high alert medications. There was unanimous agreement that new learning took place with a level of understanding that could not have been achieved apart from this lived experience. Through a transformed participant centered classroom use of relevant nursing practice concerns along with some fun and entertainment, participants’ initiative to learn improved, retention of knowledge occurred and nursing practice subsequently changed. The mock trial MOCK TRIAL METHOD 54 approach successfully challenged nurses to examine their practice and gather evidence to support changes to clinical practice. At the end of the day, nurses left feeling “inspired” about their practice and challenged to examine their own practice at a closer level. Role-play simulation through a mock trial methodology approach has roots deeply embedded in adult learning engagement that enhances instructor teaching and facilitates student participants’ learning how to evaluate best evidence and then change the practice environment. All facets of adult learning can be actualized with the mock trial approach. MOCK TRIAL METHOD 55 REFERENCES American Nurses Association. (2010). Nursing: Scope and Standards of Practice. Silver Spring, MD: American Nurses Association. ANCC. (2012). American Nurses Credentialing Center. Retrieved September 1, 2012, from ANCC web site: http://www.nursecredentialing.org/Magnet/ProgramOverview Armola, R. B. (2009). AACN levels of evidence: What's new? Critical Care Nurse , 70-73. Biddinger, L. (1999). A mock trial at nursing grand rounds. Journal for Nurses in Staff Development , 15 (3), 111-115. Billings, D. H. (2005). Teaching in nursing: A guide for faculty. St. Louis, MO: Elsevier Saunders. Bonk, C. K. (1998). Extending Socio-Cultural Theory to Adult Learning. Malwah, NJ: Lawrence Erlbaum. Brown, D. M. (2005). Developing post-operative pain management: Utilising the promoting action on research implementation in health services (PARIHS) framework. Worldviews on Evidence-Based Nursing , 2 (3), 131-140. Cronenwett, L. S. Quality and safety education for advanced nursing practice. Nursing Outlook , 57 (6), 338-348. DeYoung, S. (2008). Teaching Strategies for Nurse Educators. Upper Saddle River, N.J.: Prentice Hall. Doody, C. D. (2001). Introducing evidence into nursing practice: using the IOWA model. British Journal of Nursing , 661-664. Editors of the American Heritage Dictionary. (2009). The American Heritage Dictionary of the English Language. Boston, MA: Houghton Mifflin Company. MOCK TRIAL METHOD 56 Gerrish, K. G. (2011). Factors influencing the contribution of advanced practice nurses to promoting evidence-based practice among front-line nurses: Findings from a crosssectional survey.g . Journal of Advanced Nursing , 1079-1090. Institute of Medicine. (2003). Health professions education: A bridge to quality. Washington DC: National Academies Press. ISMP. (2012). Institute for Safe Medication Practices. Retrieved August 29, 2012, from http://www.ismp.org/Tools/highalertmedications.pdf Jenkins, R. L. (2009). A malpractice lawsuit simulation: critical care providers learn as participants in a mock trial. Critical Care Nurse , 52-60. Khan, K. C. (2006, December 15). A hierarchy of effective teaching and learning to acquire competence in evidence-based medicine. Birmingham, U.K. Kolb, D. (1984). Experiential Learning: Experience as the Source of Learning & Development. Englewood Cliffs, N.J.: Prentice-Hall, Inc. Kruszewski, A. B. (2009). Collaborative strategies for teaching evidence-based practice in accelerated second-degree programs. Journal of Nursing Education , 340-342. Langley, G. N. (2009). The Improvement Guide: A Practical Approach to Improving Organizational Performance. San Francisco: Jossey-Bass Publishers. Learning Forward. (2011). Retrieved October 14, 2012, from Learning Forward: www.learningforward.org Lisko, S. O. (2010). Integration of theory and practice: Experiential learning theory and nursing education. Nursing Education Perspectives , 106-108. Mareno, N. B. (2010, July 1). The use of audience response systems in nursing education: Best practice guidelines. Berkeley, CA, USA. MOCK TRIAL METHOD 57 Martyn, M. (2007, January 1). Clickers in the classroom: An active learning approach. Retrieved October 4, 2012, from EDUCAUSE Review Online: www.educause.edu/ero/article/clickers-classroom-active-learning-approach Melnyk, B. F.-O. (2004). Evidence based practice in nursing and healthcare: A guide to best practice. Philadelphia: Lippincott, Williams, & Wilkins. Merriam, S. C. (2007). Learning in adulthood. San Francisco, CA: Jossey-Bass. Mock Trial Academy. (2011). Mock Trial Academy. Retrieved August 29, 2012, from American Mock Trial Association: www.mocktrialacademy.com/about_what_is.asp Mosby. (2009). Mosby's Dictionary of Medicine, Nursing, & Health Professions (8th Edition ed.). Elsevier. National Staff Development Council. (2012). Learning Forward. Retrieved August 4, 2012, from www.learningforward.org: http://www.learningforward.org/standards/standards.cfm Nisbet, A. M.-C. (2009). Comparison of selected sedation scales for reporting opioid-induced sedation assessment. Pain Management Nursing , 154-164. NTL Institute. (2012). NTL Institute . Retrieved September 15, 2012, from NTL Institute web site: www.ntl.org Nurse.com. (2012, August). Retrieved October 26, 2012, from A Gannett Company; Nurse.com: http://www.nurse.com/galleries/public/index.html?galleryID=716003 Pasero, C. (2009). Assessment of sedation during opioid adminstration for pain management. Journal of PeriAnesthesia Nursing , 186-190. Patrick, S. (2007). A mock trial approach: Nursing competency program. Journal for Nurses in Staff Development. , 289-292. Patterson, B. K. (2010). Evidence for teaching practice: The impact of clickers in a large MOCK TRIAL METHOD 58 classroom environment. Nursing Education Today , 603-607. Pennington, K. M. (2010, April). EBP partnerships: Building bridges between education and practice. Nursing Management , 19-23. Phillips, J. V. (2010). Why clinical nurse educators adopt innovative teaching strategies: A pilot study. Nursing Education Perspectives , 226-229. Pravikoff, D. T. (2005). Readiness of U.S. nurses for evidence-based practice: Many don't understand or value research and have had little or no training to help them find evidence on which to base your practice. American Journal of Nursing , 105 (9), 40-51. QSEN. (2012). Quality and Safety Education for Nurses. Retrieved September 1, 2012, from QSEN: http://www.qsen.org/definition.php?id=3 Rogers, E. (2003). Diffusion of Innovation (5th ed.). New York: Free Press. Rutherford-Hemming, T. (2012). Simulation methodology in nursing education and adult learning theory. Adult Learning. , 129-137. Sogunro, O. (2004). Efficacy of role playing pedagogy in training leaders: Some reflections. Journal of Management Development , 23, 355-371. SSIH. (2012). Society for Simulation in Healthcare. Retrieved September 3, 2012, from SSIH web site: http://www.ssih.org/about-simulation Staffileno, B. M. (2010). Utilzing a mock trial to demonstrate evidence-based nursing practice: A staff development process. Journal for Nurses in Staff Development , 73-76. Swihart, D. (2006). Shared Governance: A Practical Approach to Reshaping Professional Nursing Practice. Marblehead, MA: HC Pro, Inc. Titler, M. (2008). The Evidence for Evidence Based Practice Implementation. In M. Titler, & R. Hughes (Ed.), Patient Safety & Quality: An Evidence-Based Handbook for Nurses MOCK TRIAL METHOD (p. Chapter 7). Rockville, MD: Agency for Healthcare Research and Quality. U.S. Legal Definitions. (2012). U.S. Legal Definitions. Retrieved October 19, 2012, from U.S. Legal.com: definitions.uslegal.com/m/medical-negligence/ Waxman, K. (2010). The development of evidence-based clinical simulation scenarios: Guidelines for nurse educators. Journal of Nursing Education , 29-35. Wlodkowski, R. (1999). Enhancing adult motivation to learn: A comprehensive guide for teaching all adults. San Francisco: Jossey-Bass, Inc. 59 Running head: MOCK TRIAL METHOD 60 APPENDIX A Tally Sheet of Quality Ratings Author Year Relevance Questions 1 2 3 4 Validity Questions 1 2 3 4 5 6 7 8 9 10 Quality Rating (+ or -) Sample Size Relevance to Target Population Level of Evidence Phillips 2010 Gerrish 2011 Kruszewski 2009 Jenkins 2009 Staffileno 2010 Patterson 2010 n/a + + + n/a + + + n/a + + + n/a + + + n/a + + + n/a + + + + + + + + + + + n/a + + + + + + + + + n/a + + + + + + + + + + n/a + + + + + + + + n/a - + + + + + + + n/a - + + + + + + + + n/a + 71 + 855 + 24 + 20 + 100 + 70 + C C B C C B Running head: MOCK TRIAL METHOD 61 APPENDIX B Rating the Quality of the Evidence + Positive: Indicates that the report has clearly addressed issues of inclusion/exclusion, bias, generalizability, and data collection and analysis. -- Negative: Indicates that these issues have not been adequately addressed. ∅ _Neutral: Indicates that the report is neither exceptionally strong nor exceptionally weak. NA Indicates that the report is not a primary reference and therefore the quality has not been assessed. Quality Criteria Checklist REVIEW ARTICLES RELEVANCE QUESTIONS YES NO UNCLEAR N/A 1. Will the answer, if true, have a direct effect on the health of patients? 2. Is the outcome or topic something that patients/clients/population groups would care about? 3. Is the problem addressed in the review one that is relevant to practice? 4. Will the information, if true, require a change in practice? If the answers to all of the above relevance questions are “yes”, the report is eligible for designation with a plus (+) on the Evidence Quality Worksheet, depending on answers to the following validity questions. YES NO UNN/A VALIDITY QUESTIONS CLEAR 1. Was the question for the review clearly focused and appropriate? 2. Was the search strategy used to locate relevant studies 3. 4. 5. 6. 7. comprehensive? Were the databases searched and the search terms used described? Were explicit methods used to select studies to include in the review? Were inclusion/exclusion criteria specified and appropriate? Were selection methods unbiased? Was there an appraisal of the quality and validity of the studies in the review? Were appraisal methods specified, appropriate, and reproducible? Were specific treatments/interventions/exposures described? Were treatment similar enough to be combined? Was the outcome of interest clearly indicated? Were other potential harms and benefits clearly considered? Were processes for data abstraction, synthesis, and analysis described? Were they applied consistently across studies and groups? Was there appropriate use of MOCK TRIAL METHOD qualitative and/or quantitative synthesis? Was variation in findings among studies analyzed? Were heterogeneity issues considered? If data from studies were aggregated for meta-analysis, was the procedure described? 8. Are the results clearly presented in narrative and/or qualitative terms? If summary statistics are used, are levels of significance and/or confidence intervals discussed? 9. Are the conclusions supported by results with biases and limitations taken into consideration? Are limitations of the review taken into consideration? Are limitations of the review identified and discussed? 10. Was bias due to the review’s funding or sponsorship unlikely? Negative (-) If most (six or more) of the answers to the above validity questions are “No” the review should be designated as a minus on the quality of the evidence. Neutral (Ø) If the answers to the first four (1-4) validity questions is “No” but other criteria include strengths, the review should be designated as neutral on the quality of the evidence. Positive (+) If most of the answers to the above validity questions are “Yes” (must include criteria 1,2,3, &4) the report should be designated with a plus on the quality of the evidence. Levels of Evidence (Armola, 2009)ntre for Evidence-based Medicine - Levels of A. Meta-analysis of multiple controlled studies or meta-synthesis of qualitative studies with results that consistently support a specific action, intervention, or treatment. B. Well designed controlled studies, both randomized and non-randomized, with results that consistently support a specific action, intervention, or treatment. C. Qualitative studies, descriptive or correlational studies, integrative reviews, systematic reviews, or randomized controlled trials with inconsistent results. D. Peer-reviewed professional organizational standards, with clinical studies to support recommendations. Theory-based evidence from expert opinion. E. Theory-based evidence from expert opinion or multiple case reports. F. Manufacturer’s recommendations only. 62 MOCK TRIAL METHOD 63 APPENDIX C IRC Application NURSING CLINICAL PROJECT/RESEARCH REVIEW APPLICATION Complete * Parts before initial review of application by Clinical Research or Nursing Council Chair *PART 1: ADMINISTRATIVE INFORMATION Principal Investigator(at our site): Name and Degree: Department/specialty: Manager Nursing Education Cindy T. White RN,MA, Address: Phone: 1610 Ygnacio Valley Road 925-947-3246 Walnut Creek, CA 94598 Email: cindy.white@johnmuirhealth.com Co- Investigator:(PI from other site, plus anyone else who will be helping you oversee the study) Name and Degree: Department/specialty Address: N/A Phone: Email: Study Coordinator(Research Contact) Name: Cindy T. White RN, MA Address: 1601 Ygnacio Valley Road Walnut Creek, CA 94598 Department Phone: 925-947-3246 Email: cindy.white@johnmuirhealth.com Project/Study Title: Title: Evidence Based Practice on Trial….YOU Be The Judge Version Date: Sites: (Check all that apply) JMCC JMWC MD office: Specific unit or department: Study Sponsor: Name: Cindy T. White RN, DNPc, MA, CNML Brentwood Other: Address: 1601 Ygnacio Valley Road Walnut Creek, CA 94598 Phone: 925-947-3246 Email: cindy.white@johnmuirhealth.com Does the sponsor of the activity require submission to the IRB? yes no Comments: MOCK TRIAL METHOD 64 Is funding being provided by the sponsor? yes no Attach funding information Will the study require resources be allocated by John Muir Health? yes no If yes, the research department and/or your assigned research mentor will assist you as needed to develop a budget to be submitted. Budget for the Professional Development Seminar (PDS) are provided in full by Education Dept. as a part of their annual programming. *PART 2A: STUDY SUMMARY A. Briefly state the question that this study will answer or describe the clinical issue that you want to address. What are the aims or objectives of the study? The aim was to create a dramatic and engaging courtroom drama where the nurse defendant was challenged in providing testimony to substantiate decision making and documentation related to: • scope and standards of practice • evidence based practice vs. expert opinion B. Briefly describe the background and rationale for the proposed project. Provide a summary of prior experience important to understand the proposed project. Include any relevant research literature. Why is this issue important? The background: Teaching evidence-based practice provides a challenge to the nurse educator as it compels a strong relationship between education and practice. (Pennington, 2010) Traditional teaching methodologies that are teacher-centered or passive learning instead of learner-centered or active learning can present challenges to adult learners. Traditional approaches to teaching and training methodologies such as instructor-centered lectures and learner centered self-study modules do not produce the change in knowledge, skills, and attitudes (KSA) that is essential for change in practice performance and translation to the improvement of patient outcomes at the bedside. In fact, traditional teaching methods often deter learning and practice change due to the passive exchange of knowledge. (Biddinger, 1999) There is therefore a need to supplant the traditional self-learning module efforts for more non-traditional, interactive approaches centered on the learners not the educators. Concomitant with training methodology is the attitude or inherent values of the learner. Intrinsic motivation or value of the learning experience may be inherent within and significant to the learner and/or MOCK TRIAL METHOD 65 conveyed during instruction. Whichever the case, the value or belief in what is being taught is key to adoption and application of essential learning components. Instructional strategies then must be intentional to elicit intrinsic value for adoption and application of learned principles to practice. Instructional strategies can be designed to invite the learner to value the learning. Certain conditions can be ascribed to the learning in order to enhance intrinsic motivation as noted below: (Wlodkowski, 1999): Inclusion – creating an environment of respect and connectedness between learner and instructor. Attitude – creating a favorable environment and disposition for the learner by establishing relevance. Meaning – creating thought provoking and challenging experiences that include the learner perspectives and values. Competence – creating an environment for learner understanding and engagement of content value to practice. Inclusion of these principles in instructional design helps to keep attention focused on the learning and the learner. Collectively, all these issues combined present challenges to Nurse Educators as they strive to convey the significance of clinical practice concerns, achieving optimal outcomes through applying the best evidence to guide their practice, and defending all of this through clinical documentation. The basis for crafting effective teaching methods for evidence-based practice and impacting change in the learner to affect performance at the point of service remains an area to be explored and validated. The clinical concern: Through examination of the existing process to assess patients following opioid infusion for pain management, it was determined that there were inconsistencies in nursing practice standard of performance and inadequate tools to inform early detection and intervention of increasing patient sedation and ensuing respiratory MOCK TRIAL METHOD 66 depression. Upon review and evaluation of current variation in practice along with a rise in the administration of reversal agents given for advanced respiratory depression in patients, it was determined that there was a need for a systematic way to monitor sedation levels to prevent, monitor and manage patients with intravenous infusion of high alert opioid medications. The Post Anesthesia Care Unit (PACU) nursing staff conducted a literature search to investigate current best practices in assessing and monitoring sedation levels for patients receiving opioid infusions for pain management. What they found is that gradual increases in sedation are early warning signs of ensuing respiratory depression, thus leading pain experts recommend that the level of sedation must be monitored routinely along with the management of and accompanying decrease in opioid administration until the patient demonstrates an acceptable level of sedation. (Pasero, 2009) In addition, they learned that according to a study done by Nisbet and Mooney-Cotter, (Nisbet, 2009) the Pasero Opioid Sedation Scale (POSS) was found to be the most valid and reliable tool, particularly for informing the nursing process and decision-making. The POSS tool scored even higher in ease of use with clear guidelines for nursing and confidence in making clinical decisions for patient care management. The POSS scale links the interventions to the level of sedation. The PACU nurses presented their findings to various nursing practice committees and received approval for implementation. The traditional approach to education through a self-study learning module was developed by the Nursing Education Department and assigned to all clinical nursing staff. Nurse Educators believed that additional reinforcement of educational efforts were required post implementation based upon the fact that this was a change in nursing practice. The shared governance nursing Education Council (Council) along with the Nursing Education Department was subsequently challenged was to design an effective learning approach that would have a direct impact on the nurses learning and adoption for practice performance. Discussion with the Council resulted in a unanimous decision to employ a mock trial experiential approach to educating the staff. The design would be an all day staff development continuing education program to engage nurses in a role-play courtroom drama where the nurse ‘defendant’ would be challenged to substantiate their practice based on the value and adoption MOCK TRIAL METHOD 67 of the best ‘evidence.’ References Biddinger, L. (1999). A mock trial at nursing grand rounds. Journal for Nurses in Staff Development , 15 (3), 111-115. Nisbet, A. M.-C. (2009). Comparison of selected sedation scales for reporting opioid-induced sedation assessment. Pain Management Nursing , 154-164. Pasero, C. (2009). Assessment of sedation during opioid adminstration for pain management. Journal of PeriAnesthesia Nursing , 186-190. Pennington, K. M. (2010, April). EBP partnerships: Building bridges between education and practice. Nursing Management , 19-23. Wlodkowski, R. (1999). Enhancing adult motivation to learn: A comprehensive guide for teaching all adults. San Francisco: Jossey-Bass, Inc. C. Describe the study/project design and procedures. Provide a complete description of all study procedures, assessments in a logical sequential format. Include the expected duration of subject participation. This program will be conducted as an all day seminar. Pre and post survey polling questions will be queried using an anonymous electronic ‘audience response system’ (ARS) immediately prior to and after the daylong program. These same questions will be polled via survey-monkey and tallied anonymously electronically at 6 months post seminar for sustainability measurement. Pre and post seminar incidents of narcan administration for advancing sedation will also be collected through retrospective chart audits. Describe risks or benefits of the study. There are no risks to this study. All information is retrieved electronically and un-identifiable. Survey outcomes will be reported as aggregate data for purposes of teaching and learning methodology value. Describe how the data will be analyzed. Be specific in naming any instruments you will be using in your data collection. A copy of any tools or questionnaires to be used will need submitted. Survey questions are designed to provide demographic data and measure learning effectiveness of teaching strategy and include content directly provided in the seminar and are provided below. MOCK TRIAL METHOD 1. What is your current role? a. RN b. CNA c. Social Worker d. P.T. e. Student f. Clinical Faculty - Academia g. Other 2. Where do you work? a. Acute Care Facility b. Skilled Nursing Facility c. Outpatient Clinic d. Home Health e. Academia f. Other 3. If you work in an acute care setting, what department do you work in? a. Medical - Surgical b. Critical Care c. Surgery d. Case Management e. Emergency Department f. Obstetrics (Antepartum/L&D/PP) g. Nursery (NICU & Well Baby) h. Other 4. How many years have you worked in the health care field? a. 0-2 b. 2-5 c. 6-10 d. 11-15 e. 16-20 f. Over 20 5. What was your entry into practice education? a. Diploma b. Associates Degree in Nursing c. Bachelors Degree in Nursing d. Masters Degree in Nursing 6. What is your current highest level of education? a. Diploma b. Associates Degree c. Bachelors Degree d. Masters Degree e. Doctoral Degree 7. Do you currently hold a national certification in your area of specialty? a. Yes b. No 8. The four elements of negligence that must be proven in a court of law include: a. Contract, Breach of Contract, Harm, Cost b. Duty, Breach of Duty, Harm, Causation c. Responsibility, Violation, Cause, Penalty 68 MOCK TRIAL METHOD 69 d. Duty, Violation, Testimony, Penalty e. Duty, Breach of Faith, Investigation, Cost 9. An opioid naïve patient is defined as a patient who has been: a. previously uninformed about use of Opioids b. taking less than 60mg/day of oral morphine or the equivalent for less than 7 days c. taking more than 60mg/day of oral morphine or the equivalent for less than 7 days d. taking less than 60mg/day of IV morphine or the equivalent for less than 7 days 10. For an opioid naïve patient, the recommended starting dose of Dilaudid is: a. 0.1 to 0.3mg IV every 2 hours as needed for pain b. 0.2 to 0.6mg IV every 2 hours as needed for pain c. 2 to 6 mg orally every 2 hours as needed for pain d. 1 to 3 mg orally every 4 hours as needed for pain 11. Are PCA administered opioid medications more or less likely to cause respiratory depression than other means of administering these medications? a. More likely b. Less likely 12. A decrease in respiratory rate is a reliable indicator of the presence or absence of respiratory depression for patients on opioid IV infusions? a. Yes b. No 13. Patients with the following conditions may be at higher risk for respiratory depression when placed on an IV opioid infusion: a. Greater than 70 years of age b. Opioid naïve c. Renal or hepatic impairment d. Pulmonary impairment (such as sleep apnea or COPD) e. Cardiac impairment f. Concurrent use of CNS depressants g. Abdominal or Thoracic surgical patients h. Obesity i. All of the above Retrospective chart audits will be reported out through aggregate number of incidents. D. Describe what is current standard practice: Educational standards are traditional instructor led classes. Teaching evidence-based practice is typically more traditional in approach. The current standard for the practice change conveyed in the educational seminar is the Pasero Opioid Sedation Scale which was recently implemented. The design of this seminar was initially to reinforce this education and also to teach the value of evidence-based practice at the bedside. E. What significance will the new information gained from this project have? Describe and answer questions below. What is the intent of this activity? performance improvement in our institutions Evidence based practice change: research MOCK TRIAL METHOD Are you planning to publish the activity? 70 yes no Comments: Is it anticipated the results may be applicable to another population or setting? yes no Comments: F. Will subjects be withdrawn from or denied usual therapy in order to participate in the study? N/A G. Describe alternatives to study participation that are available to subjects: N/A PART 2B: SUBJECT INFORMATION C. Identify the population being evaluated for the study. Number of subjects to be enrolled: _______ Age range of eligible subjects:__________ List all the inclusion/exclusion criteria for the study. Provide data and/or statistics to support your sample size. All participants registered for the all day seminar will be included in the study. No exclusions. Age range of subjects is unknown. Sample size will be the 160 participants who are in attendance. B. Are there any inclusion/exclusion criteria based on race, gender or ethnicity? yes no If yes, please explain rationale for the restrictions. C. How will subjects be recruited for the study? Provide detail below. (i.e. how, when, and where potential subjects will be approached) NOTE: all advertisements, whether posted of broadcast and all correspondence used for purposes of subject recruitment will need to be submitted for IRC review. Flyer attached. PART 3: Risks and Benefits A. Are there potential direct benefits to study subjects? yes no If yes, describe below. Increased learning effectiveness. B. What are the potential benefits to others(society)? Same as ‘C’ below C. How do the benefits of the study outweigh the risks? Benefits of the study will provide credence to the growing body of literature specific to the applicability for the mock trial approach to teaching evidence-based practice in nursing and healthcare. D. Does the research present more than minimal risk to human subjects? yes no Minimal risk means that the probability and magnitude of harm anticipated in the research are not greater in and of themselves than those ordinarily encountered in daily life or during the performance of routine physical or psychological tests. E. Describe any risks or discomforts and measures to minimize risks to the subject from study procedures. There are no risks associated with this study. MOCK TRIAL METHOD 71 PART 4: Data Collection Identifiers: Will you collect or receive any of the following identifiers as part of the study data? Check all that apply. none of the 18 identifiers listed social security number device identifiers/serial number dates medical record number web URLs postal address health plan numbers IP address numbers fax numbers account numbers biometric identifiers email address license/certificate numbers photos/comparable images name vehicle id numbers any other unique identifier B. Is any of the study data: derived from medical record added to medical record created or collected as part of health care used to make health care Other sources of study data: decisions C. With whom will the identifiable data be shared? A. Data will be shared through educational venues to support the value of the learning through the mock trial teaching and learning methodology. A. PART 5: Privacy and Confidentiality Describe procedures for maintaining confidentiality of the data you collect or receive. Describe how you will protect the data from access by those not authorized. All data will be collected electronically through polling and survey monkey un-identifiable tracking systems. PART 6: Informed Consent A. Will signed consent be obtained from subjects? yes no If no, explain rationale: B. Describe how, when and by whom informed consent will be obtained. No informed consent obtained as all data is for evaluation of the teaching methodology and learning effectiveness. No individual identifiable data will be known. PART 7: Financial Considerations A. Payments to subjects: 1. Will subjects receive payments or gifts for study participation? yes no If yes, describe. B. Costs to subjects: 1. Will subjects or their insurance be charged for any study procedures? yes no If yes, describe those costs and how they compare to subjects’ costs with alternative care off-study C. Cost to John Muir Health: 1. Are there costs that John Muir Health will incur in participating in this study? yes no If yes, work with your mentor to develop a budget for these costs and submit with application Running head: MOCK TRIAL METHOD 72 APPENDIX D STEPS IN MOCK TRIALS 1. The Opening of the Court Either the clerk of the court, the judge's sheriff, or the tournament official will ask all in the courtroom to rise and will call the court to order. When the judge enters, all participants should remain standing until the judge is seated. The case will be announced...i.e., "The court will now hear the case of (case name)." The judge will then ask the attorneys for each side if they are ready. 2. Opening Statements Before proceeding with its opening arguments, each team of attorneys should have one of its members introduce the team to the presiding judge. Witnesses should not be introduced. "Your Honor. My name is _______. My colleagues are Mr. _______ and Ms. _______." The presiding judge may interrupt an attorney's opening and closing statements to ask questions. a. Prosecution/Plaintiff After introducing her/himself and her/his colleagues to the judge, an attorney for the prosecution/plaintiff summarizes the evidence which will be presented to prove the case. An opening statement blends the pertinent facts of the case into a brief presentation of the legal basis for the prosecution's/plaintiff's case. However, this is not the time to argue or discuss the law. The opening statement also may establish a theme around which the presentation will revolve. b. Defense After introducing her/himself and her/his colleagues to the judge, an attorney for the defense summarizes the evidence that will be presented to the court to rebut the charges against the defendant. A theme may also be established. Defense attorneys present their opening statements MOCK TRIAL METHOD 73 immediately after the prosecution's/plaintiff's opening statement. If the trial judge allows, the defense may defer its opening statement until later in the trial Note: In general, the opening statement outlines the case. The case is not argued here. 3. Direct Examination OF WITNESSES Each side conducts the direct examination (questioning) of each of its witnesses. At this time, testimony and other evidence to establish its case will be presented. The purpose of direct examination is to allow the witness to supply the facts in support of the case. Teams should strive to present their cases in this portion of the trial in as direct and concise a manner as possible. Only those questions which are clearly relevant to the points the team wishes to make should be asked. Avoid extraneous and irrelevant questions. Note: The attorneys for both sides, on direct, cross, redirect, and re-cross, should remember that their only function is to ask questions; attorneys themselves may not testify or give evidence, and they must avoid phrasing questions in a way that might violate this rule. 4. Cross examination OF WITNESSES After an attorney has completed the direct questioning of a witness, the judge allows an opposing attorney to cross examine the witness. The cross examiner seeks to clarify or cast doubt upon the testimony of opposing witnesses. Inconsistency in stories, bias, and other damaging facts may be pointed out to the court through cross examination. Again, teams should strive to make their line of questioning in this portion of the trial as concise and to the point as possible. Don't ask irrelevant questions. 5. Redirect (Optional) Redirect provides a chance to repair damage done during cross-examination. It is not a time to introduce new evidence or to ask questions that there wasn't time for during direct. MOCK TRIAL METHOD 74 6. Re-cross (Optional) The last word, re-cross permits clarification of a brief but important point that was raised in the redirect. Note: Redirect and re-cross are optional and not scored separately from direct/cross. 7. Closing Arguments Closing arguments must be based on evidence and testimony presented during the trial. They are opportunities to summarize the case and to emphasize evidence that supports one's position and damages the opponent's. Closing statements can be high drama and should not be boring. Asking the judge/jury to put themselves in a client's position, or overt appeals to sympathy and prejudice are improper. Parties should indicate how the evidence does or does not satisfy the elements of the charge or claim as required by law and should ask for a favorable judgment. SIMPLIFIED RULES OF EVIDENCE AND PROCEDURE In trials conducted in the United States, elaborate rules are used to regulate the admission of proof (i.e., oral or physical evidence). These rules are designed to insure that both parties receive a fair hearing and to exclude any evidence deemed irrelevant, incompetent, untrustworthy, or unduly prejudicial. If it appears that a rule of evidence is being violated, an attorney may raise an objection to the judge. The judge then decides whether the rule has been violated and whether the evidence must be excluded from the record of the trial. Judges rarely interrupt to rule on evidence or testimony unless clear injustices are being committed: objections are the job of the attorneys. Attorneys develop an intuition for objections and it is common to hear, "Objection," from an attorney, followed by a ruling from the judge ("Sustained," meaning, "You're right; the question may not be asked," or "Overruled," meaning, "It's okay to ask that.") However, in the MOCK TRIAL METHOD 75 mock trial, it is critical that the lawyers be able to express the reason for an objection, such as "Objection, your honor, it's hearsay!" WITNESS EXAMINATION 1. Direct Examination (attorneys call and question witnesses) a. Leading Questions Witnesses may not be asked leading questions by the attorney who calls them. A leading question is one that suggests to the witness the answer desired by the examiner, and often suggests a "yes" or "no" answer. Acceptable direct questions are generally phrased to evoke a set of facts from the witness. Example of a direct question: "Dr. Isaac, what is your background in the study and analysis of alcohol and drug intoxication?" Example of a leading question: "Detective, did you find the defendant to be a common drunk?" b. Narration While the purpose of direct examination is to get the witness to tell a story, the questions must ask for specific information. The questions must not be so broad that the witness is allowed to wander or "narrate" a whole story. Narrative questions and narrative answers are objectionable. At times, a direct question may be appropriate, but the witness' answer may go beyond the facts for which the question asked. Such answers are subject to objection on the ground of narration. Example of a narrative question: "So, Mr. Witness, what happened in September 1993?" c. Scope of Witness Examination Direct examination may cover all facts relevant to the case of which the witness has firsthand knowledge. In addition, expert witnesses who qualify as such are allowed to give opinions about MOCK TRIAL METHOD 76 circumstances they have not actually witnessed. Any factual areas examined on direct examination may be subject to cross examination, and expert opinions are also subject to attack. d. Character For mock trial purposes, evidence about the character of a party may not be introduced unless the person's character is an issue in the case. For example, whether one spouse has been unfaithful to another is a relevant issue in a civil trial for divorce but might not be in a criminal trial for larceny. Similarly, a person's violent temper may be relevant in a criminal trial for assault but might not be in a civil trial for breach of contract. e. Refreshing Recollection If a witness is unable to recall a statement made in the affidavit, or if the witness contradicts the affidavit, the attorney on direct may seek to introduce into evidence that portion of the affidavit that will help the witness to remember. (The same method may be employed on cross examination to attack a witness' ability to remember events.) f. Redirect Examination If the witness' credibility or reputation for truthfulness has been attacked on cross examination, the attorney whose witness has been damaged may wish to ask a few more questions. These questions should be limited to the damage the attorney thinks was done by the opposing attorney on cross examination and should be phrased so as to try to save or "rehabilitate" the witness's credibility. Redirect is not the time to try to address matters that have not been raised previously by either side. 2. Cross examination (questioning of the other side's witnesses) a. Form of Questions MOCK TRIAL METHOD 77 Cross examination of witnesses is a fundamental right that can rarely be abridged. In cross examining a witness, attorneys should use leading questions that are aimed at getting "yes" or "no" responses. [Note: This does not mean that witnesses necessarily are limited to these responses. There are times when witnesses will be permitted to explain their answer, provided they have first answered the question.] In general, attorneys should avoid asking questions to which they do not already know the answers. Examples of the proper phrasing of questions would be, "Isn't it a fact that..." or "On (date), when you made a statement in your attorney's office, you said that...didn't you?" b. Scope of Witness Cross Examination The scope of cross examination is fairly broad and may cover the subject matter of the direct examination, matters affecting the credibility of the witness, and additional matters, otherwise admissible, that were not covered on direct examination. The objectives of cross examination fall into two broad categories: 1) reducing the effect of direct examination (for example, by discrediting a witness); and, 2) developing independent evidence on behalf of your side. Note: Many judges allow a broad interpretation of this rule. c. Impeachment During cross examination the attorney may want to show the court that the witness should not be believed. This process is called impeaching the witness and may be accomplished in three ways: 1. By asking the witness questions about prior conduct that lessen his or her credibility Example: "Is it true that the defendant once denied you a promotion?" 2. By asking the witness about evidence of certain types of criminal convictions of the witness MOCK TRIAL METHOD 78 3. By introducing the witness' statement, and asking the witness whether s/he has contradicted some portion of it Example: "Is this your written statement here, the one in which you stated that you were indifferent to people's social conduct?" Note: These types of questions may be used only when the questioning attorney has information that indicates that the conduct actually happened. d. Re-cross Examination If the opposing attorney has exercised her/his option for redirection of her/his witness, an attorney who has cross examined the witness may chose to recross that witness. The scope of the recross is limited to the area(s) covered during the redirect examination. ADDITIONAL RULES OF EVIDENCE 1. Hearsay a. Hearsay is defined as any evidence of an out-of-court statement made by someone other than the witness testifying, which is offered to provide the truth of a fact, to verify the testimony of any witness, or to authenticate a piece of evidence. Simply put, the court does not want to rely on second-hand statements, and hearsay is often a statement where the witness says, "I heard soand-so say..." Hearsay is not permitted. Example: Ms. Witness says, "Someone told me that Kevin likes to date older women." b. Though hearsay is not allowed at a trial, a judge may sometimes allow it if: 1. It was said by a party in the case and contains evidence which goes against his side (i.e., in a burglary case, the defendant bragged to someone that he stole the money). This is sometimes called the "admission against interest exception"; it is MOCK TRIAL METHOD 79 allowed because people do not usually say things that might be damaging to themselves unless they are true. 2. A person's state of mind is an important part of the case and the hearsay consists of evidence which described that particular person's state of mind. This is sometimes called the "state of mind exception". Example: John said he knew he could push the speedometer past its limit, which substantiates his intention to speed. 2. Opinions of Witnesses a. As a general rule, witnesses may not give opinions. Certain witnesses who have special knowledge or qualifications may be qualified as "experts"; an expert must be qualified by the attorney for the party for which the expert is testifying; this means that before an expert can be asked an expert opinion, the questioning attorney must bring out the expert's qualifications and experience. Note: For mock trial purposes, opposing counsel may not voire dire the potential expert. b. All witnesses may offer opinions based on the common experience of laypersons in the community and of which the witnesses have firsthand knowledge. Example: "I know she partied a lot." (allowed) "I don't think she could handle the liquor." (This is not allowed unless made by an expert in the field of psychology or mental health.) c. No witness may give an opinion about how the case should be decided. This is called the "ultimate issue" question. Example: "Ms. Witness, would you say that the defendant was unable to tell the truth?" (Not allowed.) 3. Lack of Personal Knowledge MOCK TRIAL METHOD 80 a. A witness may not testify to any matter of which the witness has no personal knowledge, unless the witness asked for an opinion is an expert who has been qualified as such. Example: If a teacher never supervised a student, she cannot testify that the student was not well prepared when she went into school. 4. Relevance of Evidence a. Generally, only relevant testimony and evidence may be presented. This means that the only physical evidence and testimony allowed is that which tends to make a fact which is important to the case more or less probable than the fact would be without the evidence. However, if the relevant evidence is unfairly prejudicial, may confuse the issues, or is a waste of time, the court may exclude it. This may include testimony, pieces of evidence, and demonstrations that have no direct bearing on the issues of the case or have nothing to do with making the issues clearer. Example: The defense asks, "Mr. Police Officer, to your knowledge, was the defendant dating anyone during the time in question?" (This is irrelevant unless the status of her social life is relevant to the case at issue.) 5. Introduction of Physical Evidence a. Physical evidence (objects/documents) must be relevant and authentic (shown to be what they appear to be) in order to be admissible. This year, for mock trial purposes, all exhibits contained in the case materials have been stipulated as authentic and should not be altered to give either side an unfair advantage. This means that the document is what it claims to be and need not be authenticated through witness testimony. However, exhibits are generally presented to the court through witness testimony and may be objected to on grounds other than authenticity. Example: MOCK TRIAL METHOD 81 Attorney: Your Honor, we have marked this one-page document as Prosecution/Plaintiff Exhibit 1 (or Defense Exhibit A). Let the record reflect that I am showing Prosecution's/ Plaintiff's Exhibit 1 (or Defense's Exhibit A) to opposing counsel. (Exhibit is shown to opposing counsel.) Your Honor, may I Approach the witness? The Court: You may. Attorney: Witness X, I am showing you what has been marked as Prosecution's/Plaintiff's Exhibit 1. Do you recognize that exhibit? Witness: Yes. Attorney: Could you explain for the court what it is? Witness: It is a map of the accident scene. (At this point the attorney may ask the witness any additional relevant questions about the exhibit, and then give it to the judge.) Note: Generally, no attorney or witness may read from an exhibit until it is identified and admitted into evidence by the court. However, on cross examination only, any document made or prepared by the witness who is being examined may be used for purposes of impeachment or cross examination without having been admitted into evidence. Even here, though, the attorney should solicit identification information from the witness (i.e. "Do you recall making a statement to the police?" "Is this your signature?" "Were you under oath to tell the truth when you made this statement?"). Also show the document to opposing counsel. OBJECTIONS 1. VIOLATING THE RULES OF EVIDENCE MOCK TRIAL METHOD 82 a. An attorney can object at any time that opposing attorneys have violated the rules of evidence. The attorney wishing to object should stand up and do so at the time of violation, before the witness has a chance to respond. Note: Timing is important here. You want to allow the opposing attorney to complete her/his question but prevent the witness from responding. It is important to stand as you address the court to make your objection. b. If a witness responds to an objectionable question, or if the question is appropriate but the response is objectionable, make a motion to "strike the testimony". When an objection is made, the judge sometimes will ask the reason for it. Then the judge will turn to the attorney who asked the question, and that attorney usually will have a chance to explain why the judge should overrule the objection. The judge will then decide whether a question or answer must be discarded, because it has violated a rule of evidence ("Objection sustained"), or whether to allow the question or answer to remain on the trial record ("Objection overruled"). 2. STANDARD OBJECTIONS a. Irrelevant evidence: "I object, your Honor. This testimony is irrelevant to the facts of this case." b. Leading question: "Objection, counsel is leading the witness." (Only on direct examination.) c. Improper character testimony: "Objection. The witness' character or reputation has not been put at issue." "Objection. Only the witness' reputation/character for truthfulness is at issue." d. Narration: "I move to strike, your Honor. The witness is responding in a narrative manner." e. Beyond the scope of direct examination: "Objection. Counsel is asking the witness about matters that did not come up in direct examination." (Remember, judges often broadly interpret this rule.) MOCK TRIAL METHOD 83 f. Hearsay: "Objection. Counsel's question (or the witness' answer) is based on hearsay." (If the witness makes a statement of hearsay, the attorney should also say, "...and I ask that the statement be stricken from the record.") g. Opinion: "Objection. Counsel is asking the witness to give an opinion." h. Lack of personal knowledge: "Objection. The witness has no personal knowledge that would enable her/him to answer this question." i. Non-Responsive Answer: A witness' answer is objectionable if it fails to respond to the question asked. "Your Honor, I move to strike the witness' answer as non-responsive and ask that s/he be instructed to answer the question asked." j. Assuming Facts Not in Evidence: An attorney shall not ask questions that assume unproved or unentered facts. Remember, just because something is in the Handbook doesn’t mean that it is known to the court or that it is usable as evidence. "Objection. Counsel’s question assumes facts not in evidence." MOCK TRIAL METHOD 84 APPENDIX E Cast of Characters Cast of Characters (in order of appearance) Judge …….. Jonathan Stewart, RN, MS, JD, CPHRM Bailif ………. David Fernandez (Coordinator, Patient Relations and Safety) Jury Box ……. Nancy Gibbs, RN, MSN, Holly Gaines, RN, Eloise Thiesen, RN (Manager Med/Surg), Jane Bartholic, RN, BSN (Clinical Analyst),et al Plaintiff’s Attorney, Elle Woods, RN, J.D. ……. Jennifer Chislett, RN (ICU), CCRN Ms. Woods graduated top of her class from Harvard Law School in 2002. She was president of her sorority Glamour, Elle, & Vogue and is well respected throughout the Harvard community. She is a senior partner of the prestigious law firm of Handley, Tucker and Woods, of which her father is co-founder. Ms Woods has covered many medical negligence cases for her the Firm with a success rate of 99% final verdicts in favor of the Plaintiff. Although her methods may be considered "unconventional" by legal Bar standards, such as bringing her toy poodle, "mitsy" to each court room appearance, Ms Woods continues to hold an excellent standing within national legal associations and communities and is well respected amongst her courtroom peers. Plaintiff’s Expert Witness, Tam Aflu, Pharmacist …… Tammie Masamori, PharmD Ms. Aflu has been a licensed Pharmacist for the past 25 years. During that time she has worked for a major medical center, served on the Pharmacy and Therapeutics Committee, written several MOCK TRIAL METHOD 85 policies regarding safe medication administration practices and implemented several components of the Medication Error Reduction Program at a University teaching hospital, and also served on the board for the Institute for Safe Medication Practices (ISMP), for the past 5 years. She has recently been promoted to the position of Director of Pharmacy Operations. Defense Attorney, Karen Cantor, RN, J.D. …… Linda Jones, RN, MSN Karen Cantor, J.D., is a Senior partner in the law firm: Hanson, Cantor, and Lewis, specializing in health care related litigation. Representing "EBP Medical Center" for over 10 years, she has successfully defended the organization from multiple law suits. Ms. Cantor consults on risk reduction management for the hospital and has been involved in annual policy review and revisions. Ms. Cantor is a 1984 graduate of Boalt Law School in Berkeley and is the author of over 15 articles on risk management and reduction of patient harm in the health care industry. Plaintiff Expert witness, Rebecca Slate …… Lorelle Lefler, RN (Med/Surg) Rebecca Slate, RN has a total of 10 years experience working in an acute care hospital setting and has been working as a Nurse Educator for the hospital for the past 5 years. She has trained directly under the guidance of Chris Pasero- MS, RN-BC, FAAN who is co-founder of the American Society of Pain Management Nurses. Ms. Slate also presently serves on the national committee: American Society for Pain Management Nursing of which she has been a member for the past 7 years. She is certified in medical/surgical nursing by the Medical-Surgical Nursing Certification Board of the Academy of MOCK TRIAL METHOD 86 Medical-Surgical Nurses and Board Certified in Pain Management nursing by the American Nurses Credentialing Center. Rebecca has long recognized the value of research in informing nursing practice. She understands that evidence-based practice is crucial to nursing’s legitimacy as a modern profession. She has often had to overcome resistance from nurses to practice standardization projects that she knows will improve the safety and quality of nursing care. Her logic is that ‘following proven recipes maximizes the likelihood of a good outcome and minimizes the risk of a bad outcome – no matter who the chef is. Defendant, Audrey Hagan, RN …… Roxanne Holm, RN, MSN (Nurse Educator) Audrey Hagan, RN, has been a Registered Nurse for 18 years in acute care medical / surgical nursing. She is certified in Orthopedic Nursing and has worked on the Orthopedic unit at EBP Medical Center for the past 12 years. Audrey serves on multiple patient care committees, including the Pain Management task force. She also served as a part of the group of resource trainers for the new PCA infusion pump inservice education for staff nurses. MOCK TRIAL METHOD 87 Plaintiff, Sarah Connor, Wife of patient …… Denean Hanson, RNC (NICU) Sarah Connor is a 42 years old stay at home mom with 3 children ages 2 years, 4 years, 7 years, and a baby on the way (the late John Connor’s child). She is finding it difficult to adjust to her husband’s death and to provide for her growing family in the absence of her husband’s income along with his physical presence and emotional support. Sarah and her husband were of the belief that this was supposed to be a ‘simple’ surgery that would put him back into action quickly so that he could ski with his kids and coach their soccer teams. Sarah was with her husband in the hospital the day that he died. She watched him as he became very uncomfortable following surgery. He played football in high school and college and had multiple injuries to his knee over the years. Sarah was with her husband as he self-medicated with a PCA infusion pump and rang the call light for the nurse 2 times for unrelieved pain around 7:30pm. At around 7:45pm he had fallen asleep and was snoring loudly. Sarah left quietly to grab some dinner in the cafeteria before it closed. When she returned to his room around 8:35pm she realized he wasn't snoring anymore. She sat down by his bedside and held his hand. She then noticed that his hand was limp and there was no response. As her eyes adjusted to the dim light in the room, she glanced over at his chest and did not see it moving. She pushed the nurse call button and at the same time she yelled for help. A code was called and she stood at the edge of the room as people rushed in.... Expert Witness for Defendant, Mary Sharp, RN …… Nazreen Celestial, RN (Clinical Coordinator) MOCK TRIAL METHOD 88 Mary Sharp has been a Registered Nurse for approximately 20 years. She has worked 7 of those years as a critical care / trauma nurse at a very busy county hospital and 10 years as a medical surgical nurse at the same facility. Mary is considered to be an expert nurse by her nursing peers and physician colleagues. She currently works as a charge nurse and preceptor for nursing students and new graduate nurses. Mary is also a member of her hospital’s Nurse Quality Council. She is a past member of the National Advisory Committee for the Food and Drug Administration, and 10 years ago was certified as a Legal Nurse Consultant and since has served as an expert witness in many cases. Mary is quite confident in her clinical knowledge and judgment but has not been that impressed with some of the work that is presented in nursing journals related to professional bedside nursing practice. She does not believe in “cookbook” nursing but believes instead that nurses who are experienced generally make little mistakes and that errors are almost always the result of careless or inexperienced nurses. APPENDIX MOCK TRIAL METHOD 89 APPENDIX F Mock Trial Script The value and legitimacy of evidence based professional standards of practice is on trial. Line of questioning need to add relevance in understanding the key issues in the case. The Case Case – 42 year old obese male patient, John Connor, 24 hours post op right total knee arthroplasty surgery. He is married to his beautiful wife, Sarah Connor, and they have 3 children ages 2 years, 4 years, and 7 years, and a baby on the way. In the handoff report the 12 hr day nurse reported off to the 12 hr evening nurse that the patient is doing well , very comfortable and pain was ‘controlled’ throughout the day. He is currently using his PCA pump to control his pain and is just now having breakthrough pain. The Issues Hourly Rounding SBAR handoff communication PCA infusion pump policy / high alert medications Independent Verification / Signature Opiate naïve assessment Narcan use / non use Adherence to Nursing Scope and Standards of Care / Practice Adherence to Nursing Practice Act MOCK TRIAL METHOD 90 Cast of Characters Judge Jonathan Stewart Baliff David Fernandez Plaintiff Attorney ( Jennifer Chislett, RN) Defense Expert Pharmacist Witness, (Tammie Iseri) Expert Nurse Witness #1 ( Lorelle Lefler) Defendant, nurse caring for the patient (Roxanne Holm) Plaintiff, wife of the patient ( Denean Hanson) Attorney (Linda Jones, RN) Expert Nurse Witness #2 (Nazrene Celestial) Defendant, nurse caring for the patient (Roxanne Holm) Jury Box audience Nancy Gibbs, Holly Gaines, Jane Bartholic, and 9 other members from the MOCK TRIAL METHOD 91 Character Roles Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) Karen Cantor, J.D., is a Senior partner in the law firm: Hanson, Cantor, and Lewis, specializing in health care related litigation. Representing "EBP Medical Center" for over 10 years, she has successfully defended the organization from multiple law suits. Ms. Cantor consults on risk reduction management for the hospital and has been involved in annual policy review and revisions. Ms. Cantor is a 1984 graduate of Boalt Law School in Berkeley and is the author of over 15 articles on risk management and reduction of patient harm in the health care industry. Defendant, Audrey Hagan, RN (Roxanne Holm) Audrey Hagan, RN, has been a Registered Nurse for 18 years in acute care medical / surgical nursing. She is certified in Orthopedic Nursing and has worked on the Orthopedic unit at EBP Medical Center for the past 12 years. Audrey serves on multiple patient care committees, including the Pain Management task force. She also served as a part of the group of resource trainers for the new PCA infusion pump inservice education for staff nurses. Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) Mary Sharp has been a Registered Nurse for approximately 20 years. She has worked 7 of those years as a critical care / trauma nurse at a very busy county hospital and 10 years as a medical surgical nurse at the same facility. She is considered an expert nurse by her peers and physician colleagues. She currently works as a charge nurse and clinical preceptor for nursing students and new graduate nurses. Mary is also a member of her hospital’s Nurse Quality Council. She is a past member of the National Advisory Committee for the Food and Drug Administration, and 10 years ago was certified as a Legal Nurse Consultant and since has served as an expert witness in many cases. <Mary is quite confident in her clinical knowledge and judgment but has not been that impressed with some of the work that is presented in nursing journals related to professional bedside nursing practice. She does not believe in “cookbook” nursing but believes instead that nurses who are experienced MOCK TRIAL METHOD 92 generally make little mistakes and that errors are almost always the result of careless or inexperienced nurses. > Plaintiff’s Attorney, Elle Woods, RN, J.D. (Jennifer Chislett) Ms. Woods graduated top of her class from Harvard Law School in 2002. She was president of her sorority Glamour, Elle, & Vogue and is well respected throughout the Harvard community. She is a senior partner of the prestigious law firm of Handley, Tucker and Woods, of which her father is co-founder. Ms Woods has covered many medical negligence cases for her the Firm with a success rate of 99% final verdicts in favor of the Plaintiff. Although her methods may be considered "unconventional" by legal Bar standards, such as bringing her toy poodle, "mitsy" to each court room appearance, Ms Woods continues to hold an excellent standing within national legal associations and communities and is well respected amongst her courtroom peers. Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) Ms. Tam has been a licensed Pharmacist for the past 25 years. During that time she has worked for a major medical center, served on the Pharmacy and Therapeutics Committee, written several policies regarding safe medication administration practices and implemented several components of the Medication Error Reduction Program at a University teaching hospital, and also served on the board for the Institute for Safe Medication Practices (ISMP), for the past 5 years. She has recently been promoted to the position of Director of Pharmacy Operations. Plaintiff, Sarah Connor, Wife of patient (Denean Hanson) Sarah Connor is a 42 years old stay at home mom with 3 children ages 2 years, 4 years, 7 years, and a baby on the way (the late John Connor’s child). She is finding it difficult to adjust to her husband’s death and to provide for her growing family in the absence of her husband’s income along with his physical presence and emotional support. Sarah and her husband were of the belief that this was supposed to be a ‘simple’ surgery that would put him back into action quickly so that he could ski with his kids and coach their soccer teams. Sarah was with her husband in the hospital the day that he died. She watched him as he became very uncomfortable following surgery. He played football in high school and college and had multiple injuries to his knee over the years. MOCK TRIAL METHOD 93 Sarah was with her husband as he self-medicated with a PCA infusion pump and rang the call light for the nurse 2 times for unrelieved pain around 7:30pm. At around 7:45pm he had fallen asleep and was snoring loudly. Sarah left quietly to grab some dinner in the cafeteria before it closed. When she returned to his room around 8:35pm she realized he wasn't snoring anymore. She sat down by his bedside and held his hand. She then noticed that his hand was limp and there was no response. As her eyes adjusted to the dim light in the room, she glanced over at his chest and did not see it moving. She pushed the nurse call button and at the same time she yelled for help. A code was called and she stood at the edge of the room as people rushed in.... Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) Rebecca Slate, RN has a total of 10 years experience working in an acute care hospital setting and has been working as a Nurse Educator for the hospital for the past 5 years. She has trained directly under the guidance of Chris PaseroMS, RN-BC, FAAN who is co-founder of the American Society of Pain Management Nurses. <C. Pasero is author of numerous articles is well known for her research based valid and reliable pain assessment and management tools in clinical practice. She also serves as a Nurse Educator and Clinical Consultant.> Ms. Slate also presently serves on the national committee: American Society for Pain Management Nursing of which she has been a member for the past 7 years. She is certified in medical/surgical nursing by the Medical-Surgical Nursing Certification Board of the Academy of Medical-Surgical Nurses and Board Certified in Pain Management nursing by the American Nurses Credentialing Center. <Rebecca has long recognized the value of research in informing nursing practice. She understands that evidence-based practice is crucial to nursing’s legitimacy as a modern profession. She has often had to overcome resistance from nurses like Mary to practice standardization projects that she knows will improve the safety and quality of nursing care. Her logic is that ‘following proven recipes maximizes the likelihood of a good outcome and minimizes the risk of a bad outcome – no matter who the chef is.> MOCK TRIAL METHOD 94 Cindy White “Equal Justice Under Law” are the words carved deep into stone above the entrance to the Supreme Court of the United States. This reflects the primary purpose of the law – to ensure that every person living in this country is afforded equal protection. Whenever an event occurs and circumstances are called into question, the justice system can take up that case through process of judge and jury to determine guilt or innocence, negligence or non-negligence. The court case today, although fictional, depicts events not uncommon in healthcare today. Within the healthcare system, nurses in particular play an integral part as lead care coordinators on the team overseeing quality and safe patient care through their scope and standards of practice in daily care based in scientific evidence and research. The purpose of this trial is to create an innovative, engaging, and stimulating program where you, the jury participants can experience and weigh the knowledge and evidence related to your practice. Our purpose is not to teach you the law it is to have you engage in the process of traveling down the road to scholarly inquiry through listening, evaluating, and decision making. Pay close attention to the evidence presented today and make notes on your “Deliberation Worksheets” as the outcome will depend upon you, the jury, after carefully weighing the information presented to influence your final verdict. COURT IS NOW IN SESSION MOCK TRIAL METHOD 95 The Courtroom Proceedings Calling of the Case Bailiff (David Fernandez) “All Rise. The District Court of the State of Confusion is now in session. The Honorable Judge Stewart is presiding.” Judge (Jonathan Stewart) <The judge will then be seated and will call the court to order by striking the gavel 3 times and stating to the courtroom> “You may be seated.” <To Bailiff> “What is today’s case?” Bailiff (David Fernandez) “Today’s case is 10-262010, Sarah Connor vs. EBP Medical Center and Audrey Hagan” Judge (Jonathan Stewart) “Are the Plaintiff and Defense Attorneys ready to present their cases?” Plaintiff and Defense Attorneys <Both rise and face the judge.> “Yes, your Honor.” <Both attorneys are then seated and await while Judge give instructions to the Jury.> Jury Instructions <Reviews instructions about what the jury needs to look for in this case.> “Let me review the instructions to the jurors:” “Members of the jury, the Plaintiff has the ‘burden of proof’ to prove all elements of the claim by a preponderance of evidence. This means that more than 50% of the evidence presented in court must weigh in favor of the Plaintiff.” MOCK TRIAL METHOD 96 “In this case the elements to be proven must show ‘negligence’ on the part of the Defendant, that is: conduct that is culpable because it falls short of what a reasonable person (in this case this is a NURSE) would do to protect another individual from foreseeable risks of harm. This might be through an act of omission or commission of the healthcare provider which deviates from the accepted standards of care and practice. It must further be proved that this act of negligence was the cause of the harm.” “These FOUR elements MUST be proved:” 1. Duty to Treat – this is the legal ‘duty’ of a hospital or healthcare provider to undertake care or treatment of a patient. 2. Breach of Duty – the hospital or healthcare provider failed to conform to the relevant standards of care. The standard of care is proven by the expert testimony or by obvious errors. 3. Causation - the breach of duty is considered to be the proximate cause of the harm. 4. Harm – negligence must be the proximate cause of the harm. “The verdict to be determined is ‘NEGLIGENT or ‘NOT NEGLIGENT’.” “Be patient, listen carefully, and keep everything in mind that you hear throughout the trial until the entire case is presented. You’ll be given time to discuss all the evidence and consider your verdict at the conclusion of the day.” <turns to address the attorneys> “The attorneys may now present their opening statements.” MOCK TRIAL METHOD 97 Opening Statements <Trying to prove: Breach of duty – did not perform to the standard of care and evidence based professional standards of practice – the nurse should know these and follow these.> <<Note that I made some intentional word choices here: (1) calling the decedent “John”; (2) referring to the defendant nurse simply as “the nurse”. The idea is to personalize the victim and de-personalize the defendant in order to influence the jury’s sympathies. –JDS >> Plaintiff’s Attorney (Jennifer Chislett) “Your honor, members of the jury, my name is Elle Woods, and I represent the estate of John Connor and his widow, Sarah. “The facts of this case are fairly clear. What you – the jury – are here to decide is whether everything was done right and John just happened to die, or whether his unexpected and unnecessary death was the result of negligence on the part of his nurse and the hospital. “This afternoon, you will learn the following facts: John Connor was a 42-year-old husband and father who had knee replacement surgery; After surgery, he had a Dilaudid PCA; When he told his nurse he had breakthrough pain, she bolused him with what ended up being a lethal dose of Dilaudid by IV push, then left him unattended and unmonitored; And he DIED. “John died alone, in a hospital, just a few yards from a nurse who could have saved him if she’d known or even suspected that she had overdosed him. “If you listen closely to the testimony you’ll hear, you’ll also learn some other things about this nurse: The nurse failed to recognize that John was opioid-naïve and all the safety implications that go with that; Even though John had only reported moderate pain, the nurse recklessly gave the maximum dose of PRN Dilaudid instead of starting with the lowest dose and titrating up; MOCK TRIAL METHOD 98 Although she was responsible for John’s safety, she took no precautions to protect him from the risk of accidental overdose. “Ladies and gentlemen, John’s death was not ‘just an accident’; it was not just ‘one of those things’. It was the predictable result of choices made by a reckless, negligent nurse. “Money cannot bring John back to life, give Sarah her husband back, or give their children a chance to grow up with their father. But it can pay their bills. John had 23 more productive years of work ahead of him – income that his wife and children will not have now. Why shouldn’t the one responsible for cutting John’s life short be accountable to those who will suffer as a result? “And money will send a message: that as members of the community – and past and future patients yourselves – you expect nurses to protect you from medical injuries and to do their jobs with knowledge, skill, and good judgment. “As you listen to the testimony this afternoon, please think on these things. Thank you.” MOCK TRIAL METHOD 99 Opening Statements Defendant’s Attorney (Linda Jones) <Trying to prove: Non breach of duty – did perform to the standard of care and EBP (minimize the legitimacy of EBP)> “Your honor, members of the jury, my name is Karen Cantor and I represent Nurse Audrey Hagan. “This afternoon, you will see that Nurse Hagan did indeed meet the standard of care, using sound judgment and evidence based practice in her assessment and care of Mr. Connor. Consistent with her record of safe and quality patient care over the course of her 18 year career in nursing, she did what any reasonable and prudent nurse caring for this patient would have done. “It’s important to understand here at the beginning that not every medical injury is caused by an error. There are risks to every procedure, every treatment, and every medication. A bad outcome alone is not evidence of negligence. “It’s human nature to try to find someone to blame when things don’t go as we hoped they would – especially when other people seem to be involved. But in today’s case, a conscientious, professional nurse did everything she was supposed to do and there was a bad outcome anyway. As hard as it may be to accept, that’s nobody’s fault. “Shortly, you will hear expert testimony that will make it clear that, far from being negligent, Nurse Hagan adhered to the standard of care. Mr. Connor’s death was a tragic and unexpected response to a common medication. “If she had known that Mr. Connor was unusually sensitive to Dilaudid, of course Nurse Hagan would have done everything in her power to protect him. But she had no way of knowing that this patient – who seemed healthy and robust just like so many others that she had taken care of safely – was going to have an adverse drug reaction. “As you listen to testimony this afternoon, no doubt your heart will go out to Mrs. Connor. But don’t forget to put yourselves in Nurse Hagan’s shoes and you will see that instead of being negligent, she met the standard of care and practiced appropriately based upon the standards of practice and information available to her while Mr. Connor was in her care. Thank you.” MOCK TRIAL METHOD 100 Plaintiff’s case Judge (Jonathan Stewart) “The Plaintiff’s attorney may call their first witness.” Plaintiff’s Attorney (Jennifer Chislett) <stands facing the judge> “I would like to call Pharmacist, Tam Aflu, to the witness stand.” <Witness stands and approaches the bench where she is met by the Bailiff.> Oath Bailiff (David Fernandez) “Please raise you right hand. Do you swear to tell the truth, the whole truth and nothing but the truth? If so, please say “I will.” Witness #1 “I will” Bailiff (David Fernandez) “You may be seated.” Plaintiff’s Attorney (Jennifer Chislett) “Please state your full name and your occupation.” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “My name is Tam Aflu, and I am a licensed Pharmacist in the state of Callifornia.” Plaintiff’s Attorney (Jennifer Chislett) “How long have you been a licensed Pharmacist?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “I have been a licensed Pharmacist for approximately 25 years now.” Plaintiff’s Attorney (Jennifer Chislett) “And in your years of practicing as a Pharmacist, what qualifies you as an expert in the field?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “I have been working a licensed Pharmacist in an acute care hospital my entire career. Currently I am the Director of Pharmacy Operations, and in this role, I provide monthly literature reviews of current and best evidence with the Pharmacy staff as it relates to quality and safe medication administration and MOCK TRIAL METHOD 101 patient care. We then review our policies and procedures and update as needed. This practice has enhanced the level of knowledge and expertise of our clinical Pharmacy staff and provided support for the nursing staff. Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Please explain for the jury: are unintentional overdoses of opiates going up, down, or staying the same in the United States?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “According to the Food and Drug Administration, the accidental overdose of opioids has increased over the past decade.” Plaintiff’s Attorney (Jennifer Chislett) “And in your expert opinion why do you think that is?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) There are multiple reasons for this including constantly changing approaches to pain management and a relatively recent change in the recommended IV Dilaudid dosing, and an increasing risk for respiratory depression due to associated factors that can go unrecognized if not reported by the patient or family. Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Can you please tell the jury what a high alert medication is?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Sure. A high alert medication is a drug that bears a heightened risk of causing significant patient harm when they are used in error and not prescribed, administered or monitored carefully.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Is the drug Dilaudid considered a high-alert medication?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Yes” Plaintiff’s Attorney (Jennifer Chislett) “What are strategies that are believed to prevent errors associated with highalert medications, specifically dilaudid IV infusions?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) MOCK TRIAL METHOD 102 “Standardized ordering, preparation, and administration, use of bar-coding, SMART pump technology, and independent double checks or independent verification of medication ‘five rights’ by two RN’s. Plaintiff’s Attorney (Jennifer Chislett) “What is important to know about an independent ‘double check’ or ‘verification as related to an opioid infusion on a pump?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) A double check or verification requires signatures by two independent RN’s to confirm that for a high alert medication such as an opioid infusion, that the rate of the settings on the pump are correct and that the infusion is not on the patient’s primary intravenous line.” Plaintiff’s Attorney (Jennifer Chislett) “Can you please tell the jury about what the current literature has to say about the drug Dilaudid, and what it is used for in the hospital setting?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Sure. Dilaudid is a drug which is referred to as an ‘opioid’ analgesic. Plaintiff’s Attorney (Jennifer Chislett) “What exactly is that?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Analgesics are classified into two types: anti-inflammatory drugs, which alleviate pain by reducing local inflammatory responses; and the opioids, which have a direct mechanism of action on the brain. Opioid analgesics can be used for either short or long term relief of severe pain and can induce sleep.” Plaintiff’s Attorney (Jennifer Chislett) “Please explain to the jury what an opioid naïve patient is.” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “According to the Food and Drug Administration, an opiate naïve patient is one who has been taking <60mg/day of oral morphine or the equivalent for < 7 consecutive days. So it is both the amount of the opiate AND the duration of use which are factors in the definition.” Plaintiff’s Attorney (Jennifer Chislett) “Hypothetically, let’s say, if a patient received Dilaudid 2mg IV, how much morphine is that equivalent to?” MOCK TRIAL METHOD 103 Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “That is equivalent to Morphine 13mg IV” Plaintiff’s Attorney (Jennifer Chislett) “What is a standard dose of Morphine for IV administration?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “A standard dose of Morphine for IV administration is 2-8mg.” Plaintiff’s Attorney (Jennifer Chislett) “So the dosage of Dilaudid 2mg IV is equivalent to Morphine 13mg IV which, by definition far exceeds the ‘standard’ dose limits?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Please take a look up at the screen and tell us what this chart is.” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “This chart categorizes other medications that are equivalent to 60mg of Morphine which is part of the opioid assessment process.” Plaintiff’s Attorney (Jennifer Chislett) “What is the significance of knowing all of these medications, their dosages, and what their equivalency to the opioid naïve patient is?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “The dosages and equivalencies give us a point of reference from which we can determine if the patient is opioid naïve based upon their recent medication history.” Plaintiff’s Attorney (Jennifer Chislett) “So for an opioid naïve patient, what is the recommended starting dose of Dilaudid IV?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) For opiate naïve patients, the recommended starting dose of Dilaudid IV is 0.2 to 0.6mg IV every 2hr as needed for pain.” Plaintiff’s Attorney (Jennifer Chislett) MOCK TRIAL METHOD 104 “What if the physician’s order is written in a range from a lower dose to a higher dose as needed for pain. How is it determined which dose to give the patient?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “When a range order is given, dosing must start at the lower end and titrate up based on patient response in specified increments”. Plaintiff’s Attorney (Jennifer Chislett) “Thank you. No further questions, your Honor.” MOCK TRIAL METHOD 105 Cross Examination – Defense Attorney Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) <stands up and approaches witness stand> “Isn’t it a fact, Ms. Aflu, that some opioid naïve patients can be very tolerant of opioid medications and not have any adverse effects such as respiratory depression?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Some patients, yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Are Patient Controlled Analgesia medications more or less likely to cause respiratory depression than other means of administering opiates?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Well, more likely, but that is a complicated question. Let me try to explain: An article in the British Journal of Anesthesia reported that it is harder to compare the incidence of respiratory depression between PCA and conventional methods of opioid analgesia. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “And why is that?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “This is partly because the risk is small therefore most studies would have inadequate numbers of patients in each group to be able to show a significant difference. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. Now, could you help to define respiratory depression for the jury?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Yes, however, the definitions of respiratory depression vary widely. Many authors choose to define respiratory depression as a respiratory rate of less than 8 or 10 breaths a minute, even though a decrease in respiratory rate is known to be an unreliable indicator of the presence or absence of respiratory depression. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “I see. In your opinion, then, how would you define respiratory depression?” MOCK TRIAL METHOD 106 Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) A better clinical indicator of early respiratory depression is sedation, and many medical centers routinely monitor patient sedation scores.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. Now, Ms. Aflu, what about studies that correlate a risk of respiratory depression specifically with PCA use?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Better estimates of the risk of respiratory depression with PCA can be obtained from the results of larger audits but unfortunately this is a difficult and daunting task for researchers to produce.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So basically, for the reasons stated, the studies which look at respiratory depression with PCA opioid use are inconclusive and represent too small of a sample size in order to draw generalized conclusions from these findings?” Plaintiff’s Expert Witness, Tam Aflu, Pharmacist (Tammie Iseri, PharmD) “Yes” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. No further questions, your Honor.” Plaintiff’s Attorney (Jennifer Chislett) <Stands up> “ No further questions for this witness, your Honor.” MOCK TRIAL METHOD 107 Witness #2 Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) Plaintiff’s Attorney (Jennifer Chislett) <stands facing the judge> “I would like to call my expert nurse witness, Rebecca Slate, to the witness stand.” <Witness stands and approaches the bench where she is met by the Bailiff.> Oath Bailiff (David Fernandez) “Please raise you right hand. Do you swear to tell the truth, the whole truth and nothing but the truth? If so, please say “I will.” Witness #2 “I will” Bailiff (David Fernandez) “You may be seated.” Plaintiff’s Attorney (Jennifer Chislett) <stands up and approaches witness stand> “Please state your full name and occupation.” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “My name is Rebecca Slate. I’m a Registered Nurse.” Plaintiff’s Attorney (Jennifer Chislett) “How long have you been a Registered Nurse? Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “I have been a Registered Nurse for approximately 10 years now.” Plaintiff’s Attorney (Jennifer Chislett) “What qualifies you as an expert nurse in the field?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “I have been working in an acute care hospital for the entire 10 years I’ve been licensed. Within the past 5 years I have taken on the role of Nurse Educator. In MOCK TRIAL METHOD 108 addition, I have done some of my training directly with Chris Pasero, MS, RN-BC, FAAN, who is co-founder of the American Society of Pain Management Nurses.” “I am also currently serving on the national committee: American Society for Pain Management Nursing, of which I have been a member for the past 7 years, and I am certified in both Medical - Surgical and Pain Management nursing.” Plaintiff’s Attorney (Jennifer Chislett) “Who exactly is Ms. Chris Pasero?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Chris Pasero is author of numerous articles and is most well known in the healthcare industry as a leading authority for her research based, valid and reliable pain assessment and management tools for clinical practice. She also serves as a Nurse Educator and Clinical Consultant for pain management issues.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Now lets talk about the ‘five rights’ of medication administration please explain to the jury what these are.” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Sure. The ‘five rights’ of medication administration are making sure that: the right medication and the right dose is given to the right patient through the right route at the right time.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Now please explain a ‘double check’ for a ‘high alert’ medication.” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “A double check is an independent verification by another RN – other than the one administering the medication. The second RN must verify the same things that the first RN does – that the medication matches the ‘five rights’ as compared to the original doctors order.” Plaintiff’s Attorney (Jennifer Chislett) “When should a ‘double check’ occur for a high alert infusion medication?” MOCK TRIAL METHOD 109 Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Double checks must occur during the following times: With each and any dose or injection With each cartridge or bag change With the initiation of therapy With any patient handoff Plaintiff’s Attorney (Jennifer Chislett) “Are there any additional verifications that must take place?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes. During the ‘double checks’ the infusion pump settings must also be independently verified by two RN’s which includes the medication, dose, lockout interval, continuous/basal rates, and 4 hour dose limits, at the beginning of each shift.” Plaintiff’s Attorney (Jennifer Chislett) “Please tell us what is the purpose of the assessment made by a nurse when monitoring a patient’s sedation level after opioid medication administration?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “The purpose or goal would be to identify advancing sedation before it is compounded by continued opioid administration and results in clinically significant respiratory depression, apnea episodes, and/or respiratory failure.” Plaintiff’s Attorney (Jennifer Chislett) “I imagine that there are many side effects to medications. What would you say is the number one side effect of greatest concern when administering an opioid medication?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “The primary concern is respiratory depression.” Plaintiff’s Attorney (Jennifer Chislett) “Your honor, I would like to offer into evidence Exhibit A, B, and C: the hospital’s PCA Order Set that was used with this patient, the hospital’s Patient Controlled Analgesia (PCA) policy, and the hospital’s Pain Management policy. “ <Brings documents up to the judge’s bench> MOCK TRIAL METHOD 110 Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “We’ll stipulate to that, your honor.” Judge (Jonathan Stewart) <addressing the jury> “That means the defense agrees to accept these documents as evidence in this trial.” Plaintiff’s Attorney (Jennifer Chislett) “According to this order and based on the patient’s history and nursing assessment, in your expert opinion, should he have been placed automatically on respiratory risk precautions?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Patient’s identified with even one of the risk factors for respiratory depression will require special consideration for dosing and possible increased monitoring.” Plaintiff’s Attorney (Jennifer Chislett) “I see that a basal rate was ordered. Was this appropriate, based upon current research that you are aware of?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Current studies have shown that patients receiving a basal opioid infusion dose are five times as likely to experience respiratory depression. Basal opioid infusions are NOT recommended for opioid naïve patients.” Plaintiff’s Attorney (Jennifer Chislett) “So which of these patient risk factors do you believe may have contributed to John Connor’s death?” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Objection, your honor! Calls for speculation and assumes that the patient’s death was caused by sedation which has not been proven.” Judge (Jonathan Stewart) “Overruled. The witness may answer but I want the jury to understand that this is just one opinion – not a proven fact.” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Based on my expert opinion, I would say that the patient’s risk factors were the fact that he was obese and opioid naïve – two conditions which call specifically for respiratory risk assessment and monitoring.” MOCK TRIAL METHOD 111 Plaintiff’s Attorney (Jennifer Chislett) “How do you determine adequate assessment and monitoring of a patient with ‘respiratory risk’ such as in this case?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “It is all referenced on the Pasero Opioid Sedation Scale.” Plaintiff’s Attorney (Jennifer Chislett) “Please look up at the screen. Is this the Pasero Opioid Sedation Scale?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes it is.” Plaintiff’s Attorney (Jennifer Chislett) “Would you please explain the scale to the jury?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Sure. This is an evidence-based scale that was proven in a 2009 research study to be a valid and reliable scale to determine sedation with opioid administration for pain management. The scale includes the attributes for assessing opioidinduced sedation AND instructs the clinician what action, if any, is needed based upon the level of sedation.” Plaintiff’s Attorney (Jennifer Chislett) “Is that the only reliable opioid sedation scale available to choose from?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “No. There are a few to choose from but this one is proven to be the best and most reliable.” Plaintiff’s Attorney (Jennifer Chislett) “What is the evidence to substantiate that?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “A robust study was done comparing three commonly used sedation scales to test their validity and reliability. The study reported that the POSS scale yielded the highest percentage of agreement with the scoring attributes and the nursing interventions chosen by the nurse.” Plaintiff’s Attorney (Jennifer Chislett) “What is the significance of this?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) MOCK TRIAL METHOD 112 “Study results have clinical significance for accuracy of clinical assessments and subsequent actions on behalf of patients experiencing advancing sedation during opioid analgesia. Thus, the POSS can be recommended as a superior sedation scale for the measurement of sedation during opioid administration for pain management.” Plaintiff’s Attorney (Jennifer Chislett) “Why is it necessary to monitor sedation levels instead of decreasing respiratory rate as an indicator of impending distress?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Life threatening respiratory depression is the most serious of the opioid adverse effects and NURSES are key to prevention and early recognition of clinically significant changes in the patient’s condition. Less opioid is required to produce sedation than to produce respiratory depression so sedation is a particularly sensitive indicator of impending respiratory depression. “ Plaintiff’s Attorney (Jennifer Chislett) “So you’re telling us that sedation is a red flag that respiratory depression may be coming?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Right. A gradual increase in sedation is an early warning sign.” Plaintiff’s Attorney (Jennifer Chislett) “How should the prudent nurse respond if her patient is becoming oversedated?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “By promptly reducing the amount of the opioid dosage or stopping the infusion and provide more frequent monitoring until the patient demonstrates an acceptable level of sedation.” Plaintiff’s Attorney (Jennifer Chislett) “Can’t a sedation assessment just be informal, like seeing if the patient will wake up when you touch their foot or call their name?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) Even sedated patients may rouse when the nurse enters the room, stands by the bed, or simply touches the patient. A proper sedation assessment requires the MOCK TRIAL METHOD 113 nurse to observe how quickly the patient rouses when stimulated by the presence of the nurse, a touch, or conversation. The patient’s ability to stay awake once aroused is a critical indicator of the level of sedation.” Plaintiff’s Attorney (Jennifer Chislett) “Using the POSS scale, what is the nurse supposed to do to in response to the different levels of sedation?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “As you can see on the scale, the POSS scale links nursing interventions to the various levels of sedation. As I mentioned earlier, the research validates that the use of this scale helps the nurse in making the appropriate decisions about how to proceed with opioid treatment. Plaintiff’s Attorney (Jennifer Chislett) “What would a proper respiratory assessment look like? What should the nurse be looking for?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “A proper respiratory assessment during opioid treatment requires the following: 1. Watching the rise and fall of the patient’s chest to determine the rate, depth, and regularity of respirations. 2. Listening to the sound of the patient’s lungs is also critical. Snoring indicates airway obstruction and must be attended to promptly with repositioning, a request for a Respiratory Therapy consultation, and further evaluation for the presence of obstructive sleep apnea. Even subtle snoring can evolve into a complete obstruction and so must be addressed. Plaintiff’s Attorney (Jennifer Chislett) “So thinking that snoring is ‘normal’ can lead to fatal consequences.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “OBJECTION!” Judge (Jonathan Stewart) “Objection Sustained.” Plaintiff’s Attorney (Jennifer Chislett) “Please disregard my previous statement.” MOCK TRIAL METHOD 114 “Ms. Slate can you please tell the jury if there are any nationally recognized Patient Safety organizations that offer some guidelines on this subject. If so, what are they?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes – the main one is the Institute for Safe Medication Practices (ISMP). They have compiled recommendations to help reduce patient harm from receiving narcotics. Plaintiff’s Attorney (Jennifer Chislett) “And what are those recommendations?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) ISMP recommendations state to: 1. Avoid a higher initial dose in opioid-naïve patients – especially with Dilaudid and Fentanyl. 2. Understand the correct oral to IV conversion rates. 3. Avoid the use of basal rates with patient controlled analgesia (PCA) for pain controlled of an opiate-naïve patient. Plaintiff’s Attorney (Jennifer Chislett) “Thank you. No further questions, your honor.” MOCK TRIAL METHOD 115 Cross Examination – Defense Attorney Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) <stands up and approaches witness stand> Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Ms. Slate, you seem to know quite a bit about the theoretical aspects of opioid medication and administration. But isn’t it true that everything you just discussed are merely guidelines and suggestions for nursing practice?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes, but that’s how the standard of care is determined.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “We’ll see if the jury agrees with that statement or not, Ms. Slate.” “Now, isn’t it true, Ms. Slate, that there are guidelines set forth from the California State Board of Registered Nursing (BRN) related to pain management?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes there are.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Please take a look up at the screen and read for the jury exactly what those guidelines are.” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “The California Health and Safety Code states that: ‘It is the intent (of the Legislature) that pain be assessed and treated promptly, effectively, and as for as long as pain persists.’ Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Hasn’t the BRN also issued a white paper on this subject as well?” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes, the BRN issued a white paper titled: Pain Assessment: The Fifth Vital Sign. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Ms. Slate, please look up at the screen. Printed up there is a segment of the BRN white paper. Does this look familiar to you?” MOCK TRIAL METHOD 116 Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes it does. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Please read what it states on the slide as it references the nursing judgment in the management of the patient’s pain all the way through the end of the slide.” Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) <reads the entire slide> Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. So per the California State Board of Nursing’s approved recommendations for effective pain management, the Registered Nurse is encouraged to use their nursing judgment and give patients routine and consistent pain medication within the first 24-48 hours after surgery." Plaintiff Expert witness, Rebecca Slate (Lorelle Leffler) “Yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. No further questions, your Honor.” Plaintiff’s Attorney (Jennifer Chislett) <Stands up> “ No further questions for this witness, your Honor.” MOCK TRIAL METHOD 117 Witness #3 (Plaintiff’s witness) Defendant, Audrey Hagan, RN (Roxanne Holm) Plaintiff’s Attorney (Jennifer Chislett) <stands facing the judge> “I would like to call the Defendant, Audrey Hagan, to the witness stand.” <Witness stands and approaches the bench where she is met by the Bailiff.> Oath Bailiff (David Fernandez) “Please raise you right hand. Do you swear to tell the truth, the whole truth and nothing but the truth? If so, please say “I will.” Witness #3 “I will” Bailiff (David Fernandez) “You may be seated.” Plaintiff’s Attorney (Jennifer Chislett) <stands up and approaches witness stand> “Please state your full name and your occupation.” Defendant, Audrey Hagan, RN (Roxanne Holm) “My name is Audrey Hagan, and I am a Registered Nurse.” Plaintiff’s Attorney (Jennifer Chislett) “How long have you been licensed as a Registered Nurse?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I’ve been licensed as a Registered Nurse for approximately 18 years now.” Plaintiff’s Attorney (Jennifer Chislett) “Where are you currently employed.” Defendant, Audrey Hagan, RN (Roxanne Holm) “I currently work at EBP Medical Center in a medical / surgical unit where I’ve been employed for the past 12 years.” MOCK TRIAL METHOD 118 Plaintiff’s Attorney (Jennifer Chislett) “What state are you” licensed to practice in? Defendant, Audrey Hagan, RN (Roxanne Holm) “I’m licensed in the state of California.” Plaintiff’s Attorney (Jennifer Chislett) “Do you understand your role and responsibility to your patients when you carry an RN license in the state of California?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “And for the jury, please state just what is that role and responsibility?” Defendant, Audrey Hagan, RN (Roxanne Holm) “To provide the best care possible for my patients. Plaintiff’s Attorney (Jennifer Chislett) “Please look up at the screen. This is a section of the Nurse Practice Act. Under California law, according to the Nurse Practice Act, Business and Professions Code, Chapter 6 Nursing, Section 2725, please read what it states on the first slide as to the INTENT of the legislation: Defendant, Audrey Hagan, RN (Roxanne Holm) “It states the intent of this legislation is…… ……to provide clear legal authority for functions and procedures that have common acceptance and usage. It is the legislative intent also to recognize the existence of overlapping functions between physicians and registered nurses and to permit additional sharing of functions within organized health care systems that provide for collaboration between physicians and registered nurses. Plaintiff’s Attorney (Jennifer Chislett) “Please continue reading through the second slide which begins with ‘the practice of nursing’.” Defendant, Audrey Hagan, RN (Roxanne Holm) ….the practice of nursing within the meaning of this chapter means those functions, including basic health care, that help people cope with difficulties in daily living that are associated with their actual or potential health or illness MOCK TRIAL METHOD 119 problems or the treatment thereof, and that require a substantial amount of scientific knowledge or technical skill…. Plaintiff’s Attorney (Jennifer Chislett) “Please continue reading through the third slide which begins with ‘ongoing comprehensive assessments’.” ……ongoing comprehensive assessments, diagnosis, planning, implementation, evaluation, teaching, determining stability and instability, delegation of care when appropriate, prioritization and coordination of care. This involves an ongoing comprehensive and collaborative decision making processes and activities based on dependent and independent responsibilities.” Plaintiff’s Attorney (Jennifer Chislett) “So according to what you just read which is from the California Nurse Practice Act, the practice of nursing role and responsibility is clearly spelled out in legislation to include, collaboration between physicians and nurses, a substantial amount of scientific knowledge, and an ONGOING, COLLABORATIVE DECISION MAKING process. “This is in fact the role and responsibility of the Registered Nurse as codified in law – is it not, Ms. Hagan?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Were you the nurse responsible for the care of Mr. John Connor the night he died?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes I was.” Plaintiff’s Attorney (Jennifer Chislett) Now, let’s discuss the night that you were RESPONSIBLE for the care of the patient, John Connor. “What shift do you work at the hospital, that is, what are the hours you usually work? Defendant, Audrey Hagan, RN (Roxanne Holm) “My hours are 7pm to 7am” MOCK TRIAL METHOD 120 Plaintiff’s Attorney (Jennifer Chislett) “Were those the hours you were working the night that the plaintiffs’ husband, John Connor, died?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “And please inform the jury how you start your shift, that is, how do you get information about the patients you will care for before you actually go in to see them?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I receive my patient assignment from the nurse in charge and then I review the information on each of my assigned patients’ charts. I then receive the handoff report from the off going nurse before I go in to see my patients.” Plaintiff’s Attorney (Jennifer Chislett) “Did you receive information about your patient, John Connor, that night, in the same way that you just described?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “This is a copy of the physician’s PCA order sheet. <hands her a copy> Do you remember seeing this on the chart?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “Did you think that this was a high starting dose of dilaudid?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “Did you call the doctor to question the order?” MOCK TRIAL METHOD 121 Defendant, Audrey Hagan, RN (Roxanne Holm) “No.” Plaintiff’s Attorney (Jennifer Chislett) “Why not?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Based on my experience with these type of post operative patients it did not seem like an unsafe dose.” Plaintiff’s Attorney (Jennifer Chislett) “Ok. Can you please explain which types of patients are considered at higher risk for respiratory depression from the use of opioid medications?” Defendant, Audrey Hagan, RN (Roxanne Holm) “The patients at highest risk are opioid naïve patients.” Plaintiff’s Attorney (Jennifer Chislett) “What about patients who are obese? Are they considered at higher risk for respiratory depression as well?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I believe so.” Plaintiff’s Attorney (Jennifer Chislett) “Did you assess the deceased patient, John Connor, as being at risk due to any of these previously stated risk factors?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I was not aware initially when I started my shift if that assessment had been made already. My goal at the time I came in to see Mr. Connor was to help him get relief from his pain. He was in a lot of discomfort and so pain relief was my top priority for him.” Plaintiff’s Attorney (Jennifer Chislett) “Did you use a Sedation Scale to determine Mr. Connor’s sedation level? Defendant, Audrey Hagan, RN (Roxanne Holm) “No I did not.” Plaintiff’s Attorney (Jennifer Chislett) “And why was that?” MOCK TRIAL METHOD 122 Defendant, Audrey Hagan, RN (Roxanne Holm) “Initially when I checked on him he was awake and alert and he rated his pain as a 6/10 and he stated it was “severe”. He was so uncomfortable that I knew I needed to get his pain under control so I medicated him. When I went back to check on him he was snoring and his wife said that he had just fallen asleep and to not wake him up. She also said that he snores at home so this was normal for him.” Plaintiff’s Attorney (Jennifer Chislett) “So when was it that you realized your patient, Mr. Connor , was over-sedated?” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Objection! Assumes facts not in evidence!” Judge (Jonathan Stewart) “Sustained.” Plaintiff’s Attorney (Jennifer Chislett) “I withdraw the question, your honor. “Let me ask another question, do you remember what time(s) you checked on Mr. Connor after you started your shift?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I first checked on him about half an hour after the start of my shift.” Plaintiff’s Attorney (Jennifer Chislett) “When did you realize he wasn’t breathing?” Defendant, Audrey Hagan, RN (Roxanne Holm) “When Mrs. Connor yelled for help. I came into the room and when I couldn’t arouse him I called a code.” Plaintiff’s Attorney (Jennifer Chislett) “Please take a look up at the screen. This is a copy of the electronic medical record for Mr. Connor. Does this look like what you charted on Mr. Connor?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) MOCK TRIAL METHOD 123 “So you did not perform resuscitative measures FIRST before calling a code?” Defendant, Audrey Hagan, RN (Roxanne Holm) “No” Plaintiff’s Attorney (Jennifer Chislett) “At the time that you called the code did you also immediately turn off the opioid infusion?” Defendant, Audrey Hagan, RN (Roxanne Holm) “No.” Plaintiff’s Attorney (Jennifer Chislett) “Okay. Let’s talk about something different. Is this a copy of your hospital’s pain management policy?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “Please take a look up at the screen, Ms. Hagan. Please read aloud what your hospital’s pain management policy states about the indicators of pain, in order of importance.” Defendant, Audrey Hagan, RN (Roxanne Holm) 1. Patient’s self report. 2. Pathological conditions or procedures known to be painful. 3. Pain related behaviors such as grimacing, restlessness, and vocalization. 4. Physiological measures – such as vital signs - only when none of the other alternatives exists. Plaintiff’s Attorney (Jennifer Chislett) “And which of these measures led you to over-medicate Mr. Connor?” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “OBJECTION - ARGUMENTATIVE!” Judge (Jonathan Stewart) “Sustained.” MOCK TRIAL METHOD 124 Plaintiff’s Attorney (Jennifer Chislett) “I withdraw the question. Please see section II G of the policy reflected on the screen. These two slides denote the required documentation and the interventions based upon the patients’ level of pain according to the policy. Are you familiar with this policy from your hospital?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. Now please look up at the screen again. “Please read aloud to the jury where you see in your documentation the required pain elements that you just read from section IIG of the policy.” Plaintiff’s Attorney (Jennifer Chislett) Defendant, Audrey Hagan, RN (Roxanne Holm) “I don’t see it there.” Plaintiff’s Attorney (Jennifer Chislett) “Please also read the section of your charting where a second RN verified the double check of the medication you administered.” Defendant, Audrey Hagan, RN (Roxanne Holm) “I don’t see it there.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. No further questions, your honor.” MOCK TRIAL METHOD 125 Cross Examination – Defendant, Audrey Hagan, RN (Roxanne Holm) Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) <stands up and approaches witness stand> “Ms. Hagan, please look up at the screen. This is section II E of the pain policy at EBP Medical Center. Please read aloud the top paragraph beginning with the word Analgesics.” Defendant, Audrey Hagan, RN (Roxanne Holm) “Analgesics will be provided, and the clinician will assess and document the presence or absence of any sign that may indicate ineffectiveness of the analgesic treatment.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “And from the 10 signs listed here, what were the signs that you noted in your patient, Mr. Connor, that indicated “ineffectiveness” of treatment? Defendant, Audrey Hagan, RN (Roxanne Holm) “Let’s see: from the handoff report I received, he was fairly comfortable throughout the day so based on history this was not his ‘usual’ – he was perspiring, pale, grimacing, holding his incision site – guarding / cautious and tense, stiff, frowning, vocalizing pain, restlessness, and agitated.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “That’s a very long list of indicators and from your report he had at least 8 out of the 10. I can see that pain assessment is very complex. Now please continue reading what the policy states to do if treatment is ineffective. Read the very last paragraph on the slide beginning with, If these signs are present.” Defendant, Audrey Hagan, RN (Roxanne Holm) “Sure. If these signs are present, changes in the analgesic treatment plan (increased dose, addition of other analgesics) will be considered. In the absence of ineffectiveness, the current analgesic treatment will continue.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Isn’t it a fact that you indeed provided pain relief to Mr. Connor according to the approved statements you just read to us in the policy?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes I did. < breaks down crying> I did what I was supposed to do and I took good care of my patient.” MOCK TRIAL METHOD Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So you were well within not only your standard of practice as a Registered Nurse but also within the approved policy and procedure practice guidelines that are well defined at your hospital?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. You can step down now.” Plaintiff’s Attorney (Jennifer Chislett) <Stands up> “ No further questions for this witness, your Honor.” 126 MOCK TRIAL METHOD 127 Witness #4 Sarah Connor, Wife of patient (Denean Hanson) Plaintiff’s Attorney (Jennifer Chislett) <stands facing the judge> “I would like to call the Plaintiff, Sarah Connor, to the witness stand.” <Witness stands and approaches the bench where she is met by the Bailiff.> Bailiff (David Fernandez) “Please raise you right hand. Do you swear to tell the truth, the whole truth and nothing but the truth? If so, please say “I will.” Witness “I will” Bailiff (David Fernandez) “You may be seated.” Plaintiff’s Attorney (Jennifer Chislett) “Please state your full name and your relationship to the deceased, John Connor.” Sarah Connor, Wife of patient (Denean Hanson) “My name is Sarah Connor, and I am the widow of John Connor.” Plaintiff’s Attorney (Jennifer Chislett) “Sarah, please tell the court a little bit about your relationship with your husband.” Sarah Connor, Wife of patient (Denean Hanson) “John and I were high school sweethearts and married shortly after graduation. We have 3 children together and one on the way as you can see. <shows her obviously pregnant tummy> When John and I married we decided that I would stay at home and care for the children and that is what I’ve done all these years. He has been the breadwinner and I don’t know what I’m going to do without him.” <breaks down crying> We thought that this was going to be a ‘simple’ surgery like we were told by his doctor. We thought that this would give MOCK TRIAL METHOD 128 him the chance to get back coaching the kids’ soccer games again. We just didn’t know that it would end up this way.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. I know this is very difficult for you but can you please describe the events the best that you can remember them the night that your husband, John Connor, died in the hospital.” Sarah Connor, Wife of patient (Denean Hanson) “I was with my husband in the hospital room when he was lying in the bed after surgery. He had been in pain off and on that day. We kept pushing the button on the pump to make the medication work. He even rang for the nurse two times before she came into the room. Plaintiff’s Attorney (Jennifer Chislett) “Do you remember what time that was?” Sarah Connor, Wife of patient (Denean Hanson) “I think it was sometime after 7:00pm.” Plaintiff’s Attorney (Jennifer Chislett) “Ok. Please continue.” Sarah Connor, Wife of patient (Denean Hanson) “The nurse came in and then gave him more medication sometime I think after 7:30pm. A few minutes after she medicated him he fell asleep. I thought he was finally comfortable and was so happy to see him relaxed. After he went into a deeper sleep and began snoring I went to go to the cafeteria to get some dinner. When I came back to the room I thought he was resting quietly. Plaintiff’s Attorney (Jennifer Chislett) “Then what did you do?” Sarah Connor, Wife of patient (Denean Hanson) I sat down by his bedside and held his hand. The minute I touched his hand I knew something was wrong - his hand was limp and he wasn’t responding at all. I then looked over to see if he was breathing. I got so scared – I pushed the nurse call button and at the same time yelled for help. The next thing I knew I was standing at the edge of the room while people rushed in....the rest is just a blur – a nightmare….I still can’t believe he’s gone. <breaks down crying again> Plaintiff’s Attorney (Jennifer Chislett) MOCK TRIAL METHOD 129 “Thank you. I’m so sorry – I know this must be very difficult for you. Sarah, think back a little bit and do you remember what Nurse Hagan taught you and John about using the pain pump that he was receiving? Sarah Connor, Wife of patient (Denean Hanson) “She did not teach us anything. We barely saw her.” Plaintiff’s Attorney (Jennifer Chislett) “Ok. Thank you. Did you think that your husband could DIE as a result of the medication he was receiving?” Sarah Connor, Wife of patient (Denean Hanson) “Not at all. We thought we were safe because we were in a hospital. We trusted the nurses and did not know that the medicine that was supposed to help him would kill him.” Plaintiff’s Attorney (Jennifer Chislett) “Thank you. No further questions, your honor.” Cross Examination – Defense Attorney Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “No questions for this witness, your honor.” Plaintiff’s Attorney (Jennifer Chislett) “The Plaintiff rests.” MOCK TRIAL METHOD 130 Witness #5 Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) <stands facing the judge> “I would like to call the Defenses expert nurse, Mary Sharp, to the witness stand.” <Witness stands and approaches the bench where she is met by the Bailiff.> Oath Bailiff (David Fernandez) “Please raise you right hand. Do you swear to tell the truth, the whole truth and nothing but the truth? If so, please say “I will.” Witness #5 “I will” Bailiff (David Fernandez) “You may be seated.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Please tell the jury your name, occupation, and qualifications.” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “My name is Mary Sharp and I am a Registered Nurse. I have been licensed for approximately 20 years now. For 7 of those years I worked as a critical care / trauma nurse and 10 years as a medical/surgical nurse. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you, Ms. Sharp. Please tell the jury what your current role is in the hospital where you are currently employed.” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “ I am currently a charge nurse and clinical preceptor for nursing students and new graduate nurses. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Ok. Do you have any other related affiliations?” MOCK TRIAL METHOD 131 Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “Yes. I am a member of the hospital’s Nurse Quality Council and recent past member of the National Advisory Committee for the Food and Drug Administration. I became a certified Legal Nurse Consultant about 10 years ago and have since served as an expert nurse witness on many healthcare related legal cases.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. Please explain for the jury: Does individual patient physiology affect the way that medications are processed in the body?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) Yes – individual patient’s physiological make up affects the way that medications are absorbed, processed, and excreted in the body. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Interesting. With this in mind, how does a nurse determine the appropriate dosing for a medication from a physician’s order when it is ordered ‘as needed?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “The nurse needs to evaluate each individual patient. Some basic things to consider that are: how the drug works in the body possible effects of other medications or food with the medication patient allergies to medications Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “I see. Are there any other considerations which would make an ‘as needed’ medication order inappropriate for an individual patient?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “Yes. There are contraindications such as: if the patient has any other medical conditions that preclude the use of the ordered drug or tolerance to certain drugs that may require increasing doses over time to achieve the same effect, the age, sex, size, and physical condition may alter how a drug is processed in the body. A patient’s diet and nutritional state may alter the drug's effect on the body.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So there are a lot of variables to consider – every situation is different, correct?” MOCK TRIAL METHOD Expert Witness for Defendant, Mary Sharp, RN “Right. 132 (Nazreen Celestial) Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So with so much individual patient variance, how can a nurse best provide appropriate analgesia to the patient in pain?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “This is the reason that practice guidelines, policies and procedures are just recommendations and not firm rules. For example, some opiate naïve patients are actually very tolerant of the drug Dilaudid – every case is different.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. Is it common nursing practice to question a physician’s order for prescribing medications?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “It is not common practice but can be done. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “What do you typically see in the hospital?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) Typically what we see is that the physician orders include consideration of the individual patient’s diagnosis and pre-existing medical problems, along with any other pertinent history, and other factors which the nurse may or may not know about such as drug abuse issues for example. Besides, it would be impossible to question every order so the nurse has to consider what is happening with their patient based on the known information and the patient’s stability.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Is there a standard on how to monitor patients who are using a PCA infusion pump for pain medication administration and does that standard provide guidelines to recognize signs and symptoms of opioid toxicity?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “Well, there’s a policy if that is what you are asking, but this should be adjusted to individual cases.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Well, wait – I thought we just heard from the Plaintiff’s witness that there was only one right way to monitor these patients.” MOCK TRIAL METHOD 133 Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “Every patient should receive individualized care, therefore, even with a ‘standard’, monitoring & assessment of the patient’s condition should be ultimately based upon their stability level and not a ‘canned policy’. This takes into account the nurses’ clinical reasoning based upon their assessment of the data, comprehensive assessment of the patient’s condition, along with diagnosis, planning, implementation, evaluation, teaching, and coordination of all these activities. It cannot be based upon a ‘canned’ approach – nursing is much more than that.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So – are the signs of opiate toxicity exactly the same for every patient?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “Of course not. The signs of opiate toxicity may vary from patient to patient – some may snore and it does not mean anything – others may not snore and this may be a warning sign for them. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So what exactly is the responsibility of the nurse in caring for these types of patients?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) Nurses are not expected to react to every symptom the patient has but they are expected to think critically about the symptoms which will inform their clinical reasoning and decision-making on an individualized basis. This kind of practice more directly benefits the patient than any kind of ‘canned’ practice guidelines which does not address individual patient conditions and responses to care.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. Now with regard to the PCA infusion pump, are nurses required to teach every visitor who comes in to see the patient that they should not push the PCA button for the patient?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “Of course not – that would be unrealistic. Nurses are required to teach the patient and if there are any family members in the room they would also hear the same information. MOCK TRIAL METHOD 134 Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Is it possible to teach and monitor every visitor that comes into the room about the PCA pump button?” Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “This is an impossible task. There is just no way that nurses have time or resources to monitor this. When the patient is in pain, family or friends may decide to push the button thinking they are helping the patient by doing this. They are also sometimes not forthcoming in admitting that they have done this. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. That is VERY enlightening. No further questions, your honor.” MOCK TRIAL METHOD 135 Cross Examination Plaintiff’s Attorney (Jennifer Chislett) “Ms. Sharp, is any of your testimony based upon current research and/or evidence based practice guidelines and/or expert opinion? Expert Witness for Defendant, Mary Sharp, RN (Nazreen Celestial) “My testimony is NOT based on theoretical research studies and cookbook nursing, if that’s what you’re asking. My testimony is based upon my 20 years experience as a practicing Registered Nurse. I have seen a lot of different types of patients with various diagnosis and diverse treatment options throughout the years. This has led me to better understand individualized care within the within the practice of nursing. I have gained knowledge of certain trends in patient conditions and knowledge of outliers in care and treatment so I have a very good understanding of how this is applied to the individual care my patients need to receive without having to quote the latest research studies which may or may not apply to my patients. Besides, literature reviews are based on anecdotal, personal experiences, and expert opinions as well as collected research studies. Expert nursing is more trustworthy than anyone’s academic research.” Plaintiff’s Attorney (Jennifer Chislett) “That will be for the jury to decide, Ms. Sharp. No further questions, your honor.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) <stands up> “I have no further questions for this witness, your honor.” MOCK TRIAL METHOD 136 Witness #6 Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) <stands facing the judge> “I would like to call the Defendant, Nurse Audrey Hagan, back to the witness stand.” <Witness stands and is seated on the witness stand> Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Ms. Hagan, are you familiar with your hospital’s policy on independent verification and co-signature for high alert medications?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes I am.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So you are aware that when you gave Mr. Connor the dose of IV Dilaudid for pain that this needed to be verified with another nurse AND have a co-signature on the electronic medical record?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Was this process followed in this case?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Would you please explain to the members of the jury why this was not documented at the time that you gave the medication?” Defendant, Audrey Hagan, RN (Roxanne Holm) “It was the start of my shift so I had to get another nurse who was also just starting the shift as well and it took her away from her patient to do this. She did verify but just didn’t document it at the exact moment – her intention was to come back after she assessed all of her patients and document at that time.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. What about your assessment of the patient’s opioid naïve status? Did you make this assessment and identify him as being at risk for respiratory depression?” MOCK TRIAL METHOD 137 Defendant, Audrey Hagan, RN (Roxanne Holm) “Initially I just made a quick assessment due to his increased pain agitation. I knew I needed to address this immediately.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “And, of course, you had a good reason for not documenting that first assessment at the exact time that you did it, right?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I was in the process of making assessments on all of my patient assignments so I don’t typically chart that until I’ve completed my first rounds to make sure that my patients are stable”. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Nurse Hagan, what exactly did you teach Mr. Connor and his wife about the medication that he was receiving and about the use of the PCA pump?” Defendant, Audrey Hagan, RN (Roxanne Holm) “To call me if he wasn’t getting good pain relief.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “And what did you teach Mr. Connor and his wife about the use of the PCA pump, specifically about pushing the button for pain relief?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I taught Mr. Connor to push the button if he was in pain and told Mrs. Connor to make sure that he was the ONLY one to push the button as a safety precaution.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Is there any other way a patient, family, or visitor would know without being told specifically by the nurse that they were to NOT push the PCA button?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes. There is a label posted right on the PCA button that reads: For patient use only” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So even though this is not specifically documented anywhere in the charting, it is something that you practice AND it is clearly labeled on the PCA button itself.” MOCK TRIAL METHOD 138 Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So if let’s say for instance, hypothetically, if someone was sitting beside the patient and watching him grimace in pain and wanted to help out the patient and push the button for him, they would also have been alerted to the ‘warning’ label you just described?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Thank you. Now please describe for the jury what steps you took to ensure the patient’s safety knowing that he would be receiving a high alert medication?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Either I or my nursing assistant were checking on the patient frequently, checking his comfort status to see if he received pain relief.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “What specific monitoring did you do?” Defendant, Audrey Hagan, RN (Roxanne Holm) “I checked him to see if he received pain relief first and foremost, which meant the absence of the specific signs and symptoms of pain that he was having earlier. I also monitored his respirations and sedation level.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “And of course you had a good reason for not documenting this within the first hour that you assessed the patient and responded immediately to his request for pain?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes. My intention was to come back and chart once I checked on the rest of my patients. I knew that he was comfortable and stable so I went ahead and rounded on my other patients first before charting.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Well, that certainly makes sense. Now if you would, please explain to the jury the actions you took when you learned that your patient was in trouble, that is, not breathing?” MOCK TRIAL METHOD 139 Defendant, Audrey Hagan, RN (Roxanne Holm) “I immediately pushed the ‘code’ button, yelled for help and for someone to call a ‘code’ and dialed the code number on the patient’s bedside phone.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “What was involved in your decision to not use Narcan right away and to call the Code Team before you initiated CPR?” Defendant, Audrey Hagan, RN (Roxanne Holm) “The first action taught in Basic Life Support per the American Heart Association guidelines is to get HELP first for an adult patient, THEN begin CPR – in that order and that is what I did.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “And what about your decision when to give the Narcan – why was it given after the time the code team arrived and not before then?” Defendant, Audrey Hagan, RN (Roxanne Holm) “When any patient is in distress it is important to stay with the patient so that is what I did. Once I called the code it was then that I shut off the PCA infusion and began CPR. Narcan was in the Pyxis machine outside at the nurses’ station and I could not have left him at the time to go and get it. Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So you were practicing what you knew to be best practice guidelines – calling the code FIRST, then turning off the PCA, STAYING WITH the patient and THEN performing CPR?” Defendant, Audrey Hagan, RN (Roxanne Holm) “Yes.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “So you tried valiantly to rescue him, didn’t you?” “You did everything that you could possibly do to save him, according to your scope and standards of practice as a Registered Nurse in the state of California, but he died from an unfortunate medication side effect, not because of carelessness, isn’t that correct?” Defendant, Audrey Hagan, RN (Roxanne Holm) MOCK TRIAL METHOD 140 <puts her head down, crying> “Yes. I believe I did everything I was supposed to do – just as I’ve been trained to do.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) No further questions, your honor. Cross Examination Plaintiff’s Attorney (Jennifer Chislett) “No further questions for this witness, your honor.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Your honor, the defense rests its case.” Judge (Jonathan Stewart) “You can step down now, Ms. Hagan. MOCK TRIAL METHOD 141 Closing Arguments Both attorneys verbally review the testimony and evidence presented, and ask the jury to deliberate and then come up with a final decision. After closing arguments, the jury will deliberate and determine a verdict as NEGLIGENT or NOT NEGLIGENT. Judge (Jonathan Stewart) “The attorneys may now present their closing statements, beginning with the Plaintiffs’.” Plaintiff Plaintiff’s Attorney (Jennifer Chislett) “Ladies and gentlemen, this afternoon you heard testimony that should have made it clear to you that John Connor’s death was not just a random personal tragedy, but rather the predictable outcome of nursing negligence. “Let me review all the different breaches of the standard of care you heard about. The defendant: Did not assess whether John was opiate-naïve or tolerant, and so she did not know how much danger she put him in; Did not question the physician’s inappropriate order for high-dose Dilaudid Did not assess John’s response to the Dilaudid in a timely manner and so didn’t even know the dose she’d given him was killing him; And generally failed to practice nursing at the minimum safe level because she didn’t know what the standard of care or best practices for opiate safety even were. “You can’t turn back the clock. But you can see that justice is done here today. Buy acknowledging the negligence of this nurse and awarding compensation to Sarah and her children, you can do right by them and send a message that you demand safety. “Thank you.” MOCK TRIAL METHOD 142 Defense Judge (Jonathan Stewart) “The Defense may begin their closing statement.” Defense Attorney, Karen Cantor, RN, J.D. (Linda Jones) “Your Honor and members of the jury, you have just heard testimony from an expert nurse witness and the Defendant, Audrey Hagan, herself. You have heard that Nurse Hagan did what she has been trained and licensed to do. She stayed within her scope of practice and within the policies, procedures, and customary practices of her hospital. As I stand before you today I ask you to consider the key supporting facts which were presented in testimony today. “Nurse Hagan was NOT negligent, but instead met the standard of care: · By providing an individualized plan of care for her patient. · By attending to her patient’s priority needs and concerns without delaying his care in order to document. · By practicing to the policies and procedures set forth by the institution Nurse Hagan is employed by. · By practicing to the best available evidence and utilizing individual patient care and judgment as an autonomous, thinking nurse. · By practicing to the guidelines set forth by the state and national nursing regulatory bodies. “Every death is a tragedy, but not every death requires that someone be blamed. Everyone who goes into a hospital for surgery hopes that everything will go smoothly, without complications. But it’s well known that all medical care has risks and that complications are common. If you acknowledge the evidence that you have heard today – evidence that Nurse Audrey Hagan understood and met the standard of care – you will find that she was not negligent and you will prevent the awful tragedy of Mr. Connor’s death from needlessly destroying yet another life. “Thank you.” MOCK TRIAL METHOD 143 Jury Instructions Judge (Jonathan Stewart) “Members of the jury, you have heard all of the testimony concerning this case. It is now up to you.” <Reviews instructions about what the jury needs to look for in this case.> “Let me review the instructions to the jurors:” “The Plaintiff has the ‘burden of proof’ to prove all elements of the claim by a preponderance of evidence. This means that more than 50% of the evidence presented in court must weigh in favor of the Plaintiff.” As you have listened carefully to the facts that have been presented in this case, consider the integration of the best evidence presented, the clinical experts testimony, and the individualized care of the patient. “In this case the elements to be proven must show ‘negligence’ on the part of the Defendant, that is: conduct that is culpable because it falls short of what a reasonable person (in this case this is a NURSE) would do to protect another individual from foreseeable risks of harm. This might be through an act of omission or commission of the healthcare provider which deviates from the accepted standards of care and practice. It must further be proved that this act of negligence was the cause of the harm.” “These FOUR elements MUST be proved:” 1. Duty to Treat – this is the legal ‘duty’ of a hospital or healthcare provider to undertake care or treatment of a patient. 2. Breach of Duty – the hospital or healthcare provider failed to conform to the relevant standards of care. The standard of care is proven by the expert testimony or by obvious errors. 3. Causation - the breach of duty is considered to be the proximate cause of the harm. 4. Harm – negligence must be the proximate cause of the harm. “Consider all the testimony that you heard today, the opening and closing statements and all the evidence for both sides before you determine “The verdict of ‘NEGLIGENT’ or ‘NOT NEGLIGENT’.” MOCK TRIAL METHOD 144 I will retreat to my chambers while you will be given 30 minutes to deliberate and then I will return for your final verdict.” <judge gets up and exits> Cindy – “further instructions are posted on the projection screen. There are ‘evidence’ binders at your tables for you to review should you need them. There is also a ‘Deliberation Worksheet’ for you to jot down the main points of the FOUR elements that must be proven. Once the deliberation time is up you will be asked to register your vote. For now you will begin deliberations in one of 12 groups – each group represents one juror.” After 30 minutes <judge returns to the bench> Judge (Jonathan Stewart) “Members of the jury, have you reached a verdict?” JURY FOREMAN (Nancy Gibbs) “Yes we have your honor.” Judge (Jonathan Stewart) “Please hand over the document to the Bailiff.” Bailiff (David Fernandez) <walks over to collect document from Jury Foreman and hands over to Judge> Judge (Jonathan Stewart) “You the jury, have returned a verdict of……” Wrap up for the day Cindy - Through inquiry, demonstration, and reflection on practice……the mock trial method is an innovative approach to nursing education which combines trial procedure with nursing practice and standards of care, regulatory requirements, policies, procedures, documentation standards, and the legal implication of this practice. MOCK TRIAL METHOD 145 This trial was an example of a patient safety event that has occurred across the country. This case was a representation of that. In an effort to affect quality and safe patient care this story was reproduced to help you define, clarify, enhance, and promote your nursing role in order to impact the daily care you give your patients as a well informed practicing nurse. Nurses take a leadership role in the care of their patients and in prevention of such avoidable incidents as depicted in this fictional account. Nurses are increasingly required to integrate nursing research and scientific evidence into their daily practice. This emphasis requires staff nurses to critically examine research findings and incorporate research knowledge into practice by asking questions such as: Should we change the current standard based on the evidence or support further investigation of the issue via a formal EBP research study? Evidence-based practice looks at research findings, quality improvement data and other forms of evaluation data, and expert opinion to identify methods of improvement. This is where expert opinion can sometimes trump the best evidence and available research.” At the JMMC , WC Campus, as a result of the PACU nurses influence in practice and delving into the issue of sedation scales – they determined that changes needed to happen based upon literature review and brought forth the recommendations. Staff education was planned and implemented, and practice changes resulted. Mock trial is a problem solving, systematic approach to addressing an issue – similar to EBP. The PACU nurses put research into practice. EBP is a road with many avenues that allows each staff nurse an opportunity to make a difference in his or her practice and patient care. We hope that this influences your part in practice to raise the standard of care. Ask yourself: How does this demonstration of the evidence and standards of care impact the nursing care that you give each day? How will you take this information forward to deliver safe and quality care to your patients? You are at a crossroads – you decide which road you will take – Research Road, Evidence Based Practice Road – Expert Opinion road – one, two, all three? What will you decide? Court is now Adjourned. Thank you and Good Day. Running head: MOCK TRIAL METHOD 146 APPENDIX G PowerPoint MOCK TRIAL METHOD 147 MOCK TRIAL METHOD 148 MOCK TRIAL METHOD 149 MOCK TRIAL METHOD 150 MOCK TRIAL METHOD 151 MOCK TRIAL METHOD 152 MOCK TRIAL METHOD 153 MOCK TRIAL METHOD 154 MOCK TRIAL METHOD 155 MOCK TRIAL METHOD 156 MOCK TRIAL METHOD 157 MOCK TRIAL METHOD 158 MOCK TRIAL METHOD 159 MOCK TRIAL METHOD 160 MOCK TRIAL METHOD 161 MOCK TRIAL METHOD 162 Running head: MOCK TRIAL METHOD 163 APPENDIX H Mock Trial Agenda EVIDENCE BASED PRACTICE ON TRIAL – YOU BE THE JUDGE Tuesday, October 26, 2010 0800-1630 Ball Auditorium Conference Agenda 0800-0830 Registration 0830-0840 Introduction and Overview – Cindy White, RN, MA Nursing Education Coordinator, JMMC 0840-0940 Professional Role and RN Scope of Practice – Maria O’Rourke, RN, DNSc, FAAN, AAHC, President & CEO Role Based Practice Solutions. 0940-0950 BREAK 0950-1050 Evidence Based Practice – Lynn Forsey, RN, PhD, Program Director – Nurse Scientist, Patient Care Services, Stanford 1050-1150 The Anatomy of a Lawsuit – Annie Herlik, RN, JD, CPHRM, Vice President, Risk Management, Beta Healthcare Group 1150-1250 LUNCH 1250-1330 Trial Proceedings 101 – Jonathan Stewart, RN, MS, JD, CPHRM JMMC 1330-1340 BREAK 1340-1630 Mock Trial – Education Council, et al Running head: MOCK TRIAL METHOD 164 APPENDIX I Elements Of Negligence Deliberation Worksheet FOUR ELEMENTS OF NEGLIGENCE DELIBERATION WORKSHEET 1. Duty – Did the health care provider owe the Plaintiff a duty of care? A. B. C. D. 2. Breach of Duty – Did the healthcare provider conform to the relevant standards of care? The standard of care is usually proven by expert testimony. A. B. C. D. E. F. G. 3. Causation – Was the breach of duty the proximate cause of harm? A. B. C. D. 4. Harm – Was there an actual injury? A. B. C. Running head: MOCK TRIAL METHOD APPENDIX J Pre and Post Survey Questions 1. What is your current role? a. RN b. CNA c. Social Worker d. P.T. e. Student f. Clinical Faculty - Academia g. Other 2. Where do you work? a. Acute Care Facility b. Skilled Nursing Facility c. Outpatient Clinic d. Home Health e. Academia f. Other 3. If you work in an acute care setting, what department do you work in? a. Medical - Surgical b. Critical Care c. Surgery d. Case Management e. Emergency Department f. Obstetrics (Antepartum/L&D/PP) g. Nursery (NICU & Well Baby) h. Other 4. How many years have you worked in the health care field? a. 0-2 b. 2-5 c. 6-10 d. 11-15 e. 16-20 f. Over 20 5. What was your entry into practice education? a. Diploma b. Associates Degree in Nursing c. Bachelors Degree in Nursing d. Masters Degree in Nursing 6. What is your current highest level of education? a. Diploma b. Associates Degree c. Bachelors Degree 165 MOCK TRIAL METHOD 166 d. Masters Degree e. Doctoral Degree 7. Do you currently hold a national certification in your area of specialty? a. Yes b. No 8. The four elements of negligence that must be proven in a court of law include: a. Contract, Breach of Contract, Harm, Cost b. Duty, Breach of Duty, Harm, Causation c. Responsibility, Violation, Cause, Penalty d. Duty, Violation, Testimony, Penalty e. Duty, Breach of Faith, Investigation, Cost 9. An opioid naïve patient is defined as a patient who has been: a. previously uninformed about use of Opioids b. taking less than 60mg/day of oral morphine or the equivalent for less than 7 days c. taking more than 60mg/day of oral morphine or the equivalent for less than 7 days d. taking less than 60mg/day of IV morphine or the equivalent for less than 7 days 10. For an opioid naïve patient, the recommended starting dose of Dilaudid is: a. 0.1 to 0.3mg IV every 2 hours as needed for pain b. 0.2 to 0.6mg IV every 2 hours as needed for pain c. 2 to 6 mg orally every 2 hours as needed for pain d. 1 to 3 mg orally every 4 hours as needed for pain 11. Are PCA administered opioid medications more or less likely to cause respiratory depression than other means of administering these medications? a. More likely b. Less likely 12. A decrease in respiratory rate is a reliable indicator of the presence or absence of respiratory depression for patients on opioid IV infusions? a. Yes b. No 13. Patients with the following conditions may be at higher risk for respiratory depression when placed on an IV opioid infusion: a. Greater than 70 years of age b. Opioid naïve c. Renal or hepatic impairment d. Pulmonary impairment (such as sleep apnea or COPD) e. Cardiac impairment f. Concurrent use of CNS depressants g. Abdominal or Thoracic surgical patients h. Obesity i. All of the above Running head: MOCK TRIAL METHOD 167 APPENDIX K Polling Outcomes Demographics Number of Responses Number of Responses Where do you work? 100 80 60 40 20 0 Acute Care Facility Skiled Nursing Facility Outpatient Clinic Home Health Academia Other Seminar 79 0 3 2 3 11 6 Months Post 35 0 0 0 1 2 What is your current role? 120 100 80 60 40 20 0 RN LVN Student FacultyAcademia Other Seminar 108 0 0 2 1 6 Months Post 37 0 0 0 0 Number of Responses Of those in acute care, how many work in the following departments? 40 35 30 25 20 15 10 5 0 Emerge Obstetri Nursery Medical Case Critical ncy cs (AP, (NICU & Surgery Manage Care Depart L&D, Well Surgical ment ment PP) Baby) Other Seminar 35 22 10 3 5 6 2 22 6 Months Post 11 9 4 0 2 1 2 9 MOCK TRIAL METHOD 168 Number of Responses Gender 120 100 80 60 40 20 0 Female Male Seminar 114 2 6 Months Post 31 5 Number of Responses How many years have you worked in health care field? 80 60 40 20 0 0-2 2-5 6-10 11-15 16-20 Over 20 Seminar 0 7 8 12 14 69 6 Months Post 0 3 3 6 2 23 Number of Responses What was your entry into practice education? 70 60 50 40 30 20 10 0 Diploma Associates Degree in Nursing Bachelors Degree in Nursing Masters Degree in Nursing Seminar 21 38 59 4 6 Months Post 6 14 17 0 MOCK TRIAL METHOD 169 Number of Responses What is your highest level of education? 90 80 70 60 50 40 30 20 10 0 Associates Degree Bachelors Degree Masters Degree Doctoral Degree Seminar 5 20 79 18 0 6 Months Post 3 4 21 9 0 Number of Responses Diploma Do you currently hold a national certification in your area of specialty? 80 70 60 50 40 30 20 10 0 Yes No Seminar 73 40 6 Months Post 25 12 MOCK TRIAL METHOD 170 Evidence Based Practice The Four Elements of Negligence that must be proven in a court of law include: 120 100 Number of Responses 80 60 40 20 0 Contract, Breach of Contract, Harm, Cost Duty, Breach of Duty, Harm, Causation Responsibilit y, Violation, Cause, Penalty Duty, Violation, Testimony, Penalty Duty, Breach of Faith, Investigation , Cost Pre Seminar 17 69 19 6 3 Post Seminar 0 103 2 1 0 6 Months Post 4 30 2 0 0 Number of Responses An Opioid Naïve Patient is defined as a patient who has been : 100 90 80 70 60 50 40 30 20 10 0 previously uninformed about use of Opioids taking less than 60mg/day of oral morphine or the equivalent for less than 7 days taking more than 60mg/day of oral morphine or the equivalent for less than 7 days taking less than 60mg/day of IV morphine or the equivalent for less than 7 days Pre Seminar 26 70 11 12 Post Seminar 3 91 4 9 6 Months Post 3 31 2 1 MOCK TRIAL METHOD 171 For an opioid naïve patient, the recommended starting dose of Dilaudid IV is: Number of Responses 80 70 60 50 40 30 20 10 0 0.2 to 0.6mg IV every 2 hours as needed for pain 2 to 6 mg orally every 2 hours as needed for pain 1 to 3 mg orally every 4 hours as needed for pain Pre Seminar 54 42 2 22 Post Seminar 26 76 5 0 6 Months Post 1 Number of Responses 0.1 to 0.3mg IV every 2 hours as needed for pain Are PCA administered opioid medications more or less likely to cause respiratory depression than other means of administering these… 80 60 40 20 0 More likely Less likely Pre Seminar 55 74 Post Seminar 59 47 6 Months Post 17 20 Number of Responses MOCK TRIAL METHOD 172 A decrease in respiratory rate is a reliable indicator of the presence or absence of respiratory depression for patients on opioid IV infusions. 100 80 60 40 20 0 Yes No Pre Seminar 87 41 Post Seminar 42 65 6 Months Post 21 16 MOCK TRIAL METHOD 173 Patients with the following conditions may be at higher risk for respiratory depression when placed on an IV opioid infusion: Number of Responses 140 120 100 80 60 40 20 0 Pulmo nary Abdom Renal impair Concur inal or Greate or ment Cardia rent Thorac r than Opioid hepati (such c use of ic Obesit 70 naïve c as impair CNS surgica y years impair sleep ment depres l of age ment apnea sants patient or s COPD) All of the above Pre Seminar 0 0 5 3 0 0 0 1 120 Post Seminar 0 2 0 1 0 0 0 0 100 6 Months Post 0 0 0 0 0 0 0 0 37