MMR - Measles, Mumps & Rubella
advertisement

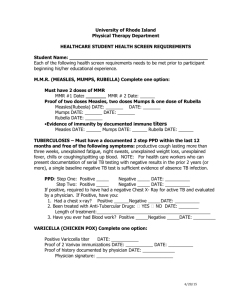
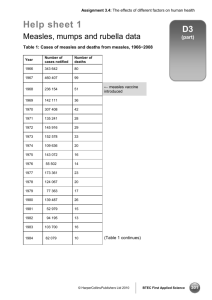
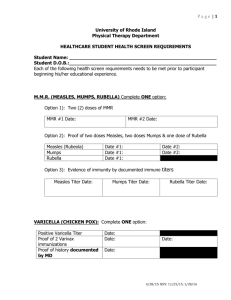
MMR Measles, Mumps &Rubella By DR.I.SELVARAJ B. Sc., M.D., D.P.H., D.I.H., PGCH&FW( NIHFW, New Delhi) Indian Railways Medical Service (Rtd) Assistant Professor • This PowerPoint presentation will be an additional resources for Para medical people Public health nurses, MBBS students and MD Post graduate students around the world. • This droplet infections has to be eradicated. As we are having effective vaccine against this infections, no carriers & no animal reservoir and paramedical people can easily identify the signs & symptoms • The public health institution has to give more importance for this infectious diseases to control • My best wishes to the Supercourse team Dr.I.Selvaraj Indian railways Medical service (Rtd) Measles (English Measles) Agent • Agent- RNA virus ( Paramyxo virus family, genus Morbillivirus ) • Source of infection-cases of measles, but not carriers. • No animal reservoir • Infective material- Nasal secretion ,Respiratory tract &Throat • Communicability- Highly infectious during prodromal period and at the time of eruption. • Secondary attack rate- > 80% Host factors • Age- 6 months to 3 years even up to 10 years • Incidence equal in both sexes • Immunity – life long immunity • Malnourished children are susceptible Environmental factor • Winter season, over crowding • Transmission – Droplet infection • 4 days before and 4 days after rash • Incubation period- 7 days Courtesy : Adapted from Mims et al. Medical Microbiology, 1993, Mosby Clinical features • Prodromal stage • Eruptive stage • Post-measles stage Clinical features • • • • 3 Cs (Cough, Coryza & Conjunctivitis) Koplik spots Four days fever (400c) Generalized, maculopapular,erythematous rash. Courtesy : This media comes from the Centers for Disease Control and Prevention's Public Health Image Library (PHIL), with identification number #3168 KOPLIK SPOT Source: http://phil.cdc.gov/PHIL_Images/20040908/4f54ee8f0e5f49f58aaa30c1bc6413ba/6111_lo res.jpg Complication • Diarrhea, • Pneumonia • Otitis media • Convulsions, • SSPE (sub acute sclerosing panencephalitis) WHO strategy for control and prevention of Measles 1) Catch up 2) Keep up 3) Follow up Mumps The name comes from the British word "to mump", that is grimace or grin. The appearance of the patient as a result of parotid gland swelling seems to be in grin Courtesey: This media comes from the Centers for Disease Control and Prevention's Public Health Image Library (PHIL), with identification number #130 Content Providers: CDC/NIP/Barbara Rice Agent • Myxovirus parotidis –RNA virus • Source of infection – Respiratory, milk • Period of communicability – 4-6 days of onset of symptoms • Secondary attack rate – 86% • Age & sex 5-15 yrs and girls common • Immunity - life long • Environmental factor – winter and spring season favors • Mode of transmission – droplet • I.P - 2 to 3 weeks Clinical features • Parotid swelling • Ovaritis • Pancreatitis • Ear ache • Orchitis Courtesy : Adapted from Mims et al. Medical Microbiology, 1993, Mosby Complications • • • • • • • Orchitis Epididymitis Oophoiritis Spontaneous abortion Sensori neural hearing loss, (uni- or bilateral). Mild form of meningitis Encephalitis Rubella (German measles) • The name rubella is derived from a Latin term meaning "little red." • Rubella is sometime called German Measles or 3-day Measles. • The synonym "3-day measles" derives from the typical course of rubella exanthema that starts initially on the face and neck and spreads centrifugally to the trunk and extremities within 24 hours. • It then begins to fade on the face on the second day and disappears throughout the body by the end of the third day. • It is a generally mild disease caused by the rubella virus. • Agent – RNA virus (Togo virus family), Genus Rubivirus. • Source of infection – Respiratory secretion • Host -3-10 yrs • Immunity –life long • Environmental factors –winter and spring season • Transmission – droplet, vertical transmission • I.P – 2-3 weeks average 18 days • Eye pain on lateral and upward eye movement (a particularly troublesome complaint) • Conjunctivitis • Sore throat • Headache • General body aches • Low-grade fever • Chills • Anorexia • Nausea • Tender lymphadenopathy (particularly posterior auricular and suboccipital lymph nodes) • Forchheimer sign (an enanthem observed in 20% of patients with rubella during the prodromal period; can be present in some patients during the initial phase of the exanthem; consists of pinpoint or larger petechiae that usually occur on the soft palate) Temperature • Fever is usually not higher than 38.5°C (101.5°F). Lymph nodes • Enlarged posterior auricular and suboccipital lymph nodes are usually found on physical examination. Mouth • The Forchheimer sign may still be present on the soft palate. Image in a 4-year-old girl with a 4-day history of low-grade fever, symptoms of an upper respiratory tract infection, and rash. Courtesy of Pamela L. Dyne, MD. • 0–28 days before conception - 43% chance • 0–12 weeks after conception - 51% chance • 13–26 weeks after conception - 23% chance • Infants are not generally affected if rubella is contracted during the third trimester Photo source: U.S. Centers for Disease Control and Prevention Salt and pepper retinopathy http://www.kellogg.umich.edu/theeyeshave it/congenital/retinopathy.html Courtesy http://phil.cdc.gov/phil_images/2003072 4/28/PHIL_4284_lores.jpg Content Providers(s): CDC Creation Date: 1976 Courtesy: Jonathan Trobe, M.D. - University of Michigan Kellogg Eye Center • Sensorineural hearing loss – 58% • Ocular abnormalities including cataract, infantile glaucoma, Micro ophthalmia and pigmentary retinopathy occur in approximately 43% • Congenital heart disease including patent ductus arteriosus (PDA) and pulmonary artery stenosis - 50% Measles vaccine • Live attenuated measles virus (Edmonston-zagreb strain) Propagated on human diploid cell (MRC-5) • 0.5 ml of vaccine • Not less than 1000 CCID50 of measles virus • 2.5% of gelatin • 5% of sorbitol as stabilizers • 0.5 ml of sterile water • Dose – 0.5 ml • Route of administration: Sub-cutaneously • 3 to 5 weeks antibody level – 200mLU/ml Mumps Vaccine • 10 strains of the mumps virus are in use throughout the world for the preparation of live attenuated vaccine. • Jeryl Lynn strain which was named after the child from whom the virus was isolated. • Leningrad-3 strain • Urabe strain • Hoshino, Torii and NKM - 46 strains • L-Zagreb MMR Vaccine • Live attenuated strains of Edmonston-Zagreb Measles virus propagated on human diploid cell culture, • L-Zagreb Mumps virus propagated on chick embryo fibroblast cells • Wistar RA 27/3 Rubella virus propagated on human diploid cell culture. • The reconstituted vaccine contains, in single dose of 0.5 ml. not less than 1000 CCID50 of Measles virus 5000 CCID50 of Mumps virus 1000 CCID50 of Rubella virus. Diluent : Sterile water for injection. The vaccine meets the requirements of USP and WHO when tested by the methods outlined in USP and WHO, TRS 840 (1994). • For active immunization in children of 12 months to 12 years of age against Measles, Mumps and Rubella infections –MMR Vaccine to be given • For immunisation of susceptible non pregnant, adolescent and adult females, we have to use Rubella Vaccine) • Measles vaccine has to be given at 9 months, • If Measles vaccine is given ,a 3 months gap is advisable to give MMR vaccine • MMR vaccine may be given between 12-15 months of age. • If Measles vaccine was missed , MMR dose replaces it, when given at or after 12 months. • • The vaccine should be reconstituted with the diluent supplied (Sterile water for injection) using a sterile Auto disabled syringe with needle. • After reconstitution the vaccine should be used immediately. • A single dose of 0.5 ml should be administered by deep subcutaneous injection into the upper arm. • If the vaccine is not used immediately then it should be stored in the dark at 2° - 8°C for no longer than 8 hours. Age Vaccines Note 9 months Measles Deep subcutaneous injection into the upper arm. 12-15 months MMR -1 Deep subcutaneous injection into the upper arm. MMR -2 Deep subcutaneous injection into the upper arm. 5 years • Murray et al., Microbiology 5th Ed., Chapters 56, 59, 63 (pp. 645-648) • Mims et al. Medical Microbiology, 1993 • K. Park 21st edition • Text book of community medicine by Sundarlal, Adarsh, Pankaj