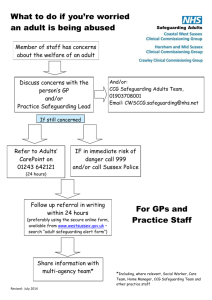
150722 GP Safeguarding Procedures Children June 2015 Final For
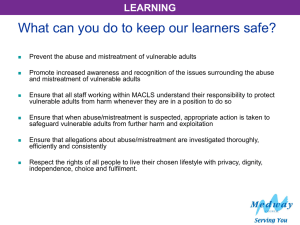
advertisement

Practice Logo SAFEGUARDING CHILDREN: SAMPLE POLICY, PROCEDURES AND GUIDANCE FOR GENERAL PRACTICE JUNE 2015 PLEASE READ THESE PROCEDURES IN CONJUCTION WITH THE LANCASHIRE SAFEGUARDING CHILDREN BOARD MULTI-AGENCY PROCEDURES (LSCB): http://panlancashirescb.proceduresonline.com/ YOUR PRACTICE SAFEGUARDING CHILDREN LEAD IS: YOUR PRACTICE DEPUTY SAFEGUARDING CHILDREN LEAD IS: This document was correct at the date of publication. It is the responsibility of the GP practice to check the contents and ensure that they are updated as necessary in accordance with national and local guidance. 1 Title Safeguarding Children: SAMPLE Policy and Procedures for General Practice Replaces Safeguarding Children Sample Policy for General Practice 2011. Author/originator Pan – Lancashire Document – reviewed and revised by C Turner, BCCG Designated safeguarding children’s’ leads pan Lancashire Recommended Version 1.0 Equality Analysis Completed November 2014 Circulation All GP Practices Review June 2017 Acknowledgements Jean Rollinson, Designated Nurse, CSR CCG Sue Clarke, Designated Nurse BwD CCG Julie Adesanya, Designated Nurse, Trafford CCG (Appendix One) This sample safeguarding children guidance and procedures has been based on the GP Toolkit: Safeguarding Children and Young People in Practice (NSPCC & RCGP 2014). It has been adapted to reflect the Guidance and Procedures of Lancashire Safeguarding Children Board. It has been updated to reflect local and national developments. Page 2 of 51 CONTENTS Section 1.0 Introduction Page 5 2.0 Safeguarding Children Policy Statement 6 3.0 What is Safeguarding? 7 Definitions of child protection, children in need and significant harm 4.0 Role and Responsibilities of : The LSCB, Children’s Social Care GP Practice (including implementation of policy) All Doctors GP Practice Safeguarding Children Lead Designated Professionals Individual staff members including all partners etc 8 8 8 10 11 11 12 12 5.0 Recognition of Abuse Definitions 13 6.0 Safeguarding in Special Circumstances Children who are ‘Looked After’ by the Local Authority Child Sexual Exploitation Fabricated and Induced Illness Domestic Abuse (including MARAC) Honour Based Abuse/Violence Forced Marriage Female Genital Mutilation (FGM) MAPPA Private Fostering PREVENT Children who are not in school 14 14 15 16 17 18 18 18 19 19 19 21 7.0 What to do if you have concerns about a child’s welfare. Acting on current concerns Responding to a child who tells you about abuse What to do if a member of the public raises concerns 22 22 23 23 8.0 Barriers to Safeguarding 24 9.0 Information Sharing 25 10.0 GP Attendance at Child Protection Case Conferences 25 11.0 Recording information Identifying potential safeguarding concerns 25 27 Page 3 of 51 CONTENTS 12.0 13.0 Creating a safe environment Safer employment Staff behaviour and professional boundaries Use of Internet, Mobile Phones and Electronic Equipment Inappropriate types of sites Managing allegations against staff/workers who have contact with children Whistleblowing Complaints Consent Serious Untoward Incidents Training Supervision 27 27 27 28 29 29 Safeguarding Processes Common Assessment Framework (CAF) 31 Domestic Homicide Reviews Serious Case Reviews Child Death Overview Panel (CDOP) 31 31 31 Practices Safeguarding 30 30 30 30 30 30 14.0 Reviewing the Arrangements Governance 32 15.0 CQC Guidance 33 16.0 Equality Impact Assessment 34 17.0 References and Bibliography (including useful web links) 34 18.0 Appendices Appendix One: Equality Impact Initial Assessment Appendix Two: Safeguarding Children Training Guidance to meet statutory requirements Appendix Three: Useful Contact Numbers Appendix Four: Signs of Abuse Appendix Five: What to do if you are concerned about a child – flowchart Appendix Six: Information Sharing – Seven Golden rules and flowchart Page 4 of 51 1.0 INTRODUCTION Effective safeguarding depends on a culture of zero tolerance of harm, where concerns can be raised with confidence so that action will be timely, effective, proportionate and sensitive to the needs of those involved. Public awareness continues to improve and there is an increasing expectation that service providers have systems in place to identify early indicators of abuse, prevent harm and that they act quickly and effectively in partnership with other relevant agencies to safeguard children when it is discovered that they are experiencing harm, exploitation, coercion, neglect or abuse. Children and young people are part of the general population – most are registered with a GP. GP’s often see multiple family and household members and are well placed to identify risk factors in parents and carers such as domestic abuse, substance misuse and mental health issues. GPs remain the first point of contact for most health problems. This sometimes includes families who are not registered but seek medical attention. A GP may be the first to recognise parental and/ or carer health problems, or someone whose behaviour may pose a risk to children. The primary health care team may be the only professionals to have contact with infants and pre-school children and young people. Lack of sensitive responsive care from care givers in infancy can seriously impact on the developing infant. The long-term effects of abuse are widely documented and include a range of physical, psychological, emotional and social effects. In order to achieve optimum life chances for children and young people, early detection and intervention is paramount. Depending on the circumstances of a particular case, intervention may be an assessment of further support needed for a child and family/carers (for example, a child or family in need of services), or a child in need of protection. It is crucial that a holistic approach is taken with families when treating a parent/carer who may be experiencing domestic abuse, mental health or learning difficulties or where there is substance misuse (including alcohol) – professionals should always give thought as to how these parental factors may impact on their ability to parent a child. PREVENT (anti-terrorism and radicalisation), Domestic abuse, so called “Honour Based Violence”, Forced Marriage, Human Trafficking and Female Genital Mutilation fall within the scope of safeguarding children and young people. These cases will often be co-worked with the Children’s Designated and Named Professionals for Safeguarding, social care and police service colleagues. GP practices have a duty of care for children and young people to whom they provide care and services. This includes ensuring their safety on GP premises and minimising any risk presented by practice staff, including GPs, by having in place safe recruitment practices and procedures for managing allegations against workers. Page 5 of 51 This local policy should be read in conjunction with the Lancashire Safeguarding Children Board multi-agency procedures (LSCB): http://panlancashirescb.proceduresonline.com/ This policy addresses the responsibilities of all members of the practice team and those outside the immediate primary care team with whom we work. For employees of the practice, failure to adhere to this policy and procedures could lead to dismissal and/or constitute gross misconduct. 2.0 SAFEGUARDING CHILDREN POLICY STATEMENT This policy and associated procedures demonstrate the commitment of the practice to ensure that throughout our work we will safeguard and promote the welfare of children. We aim to do this by ensuring that we comply with statutory and local guidance for safeguarding and promoting the welfare of children, and by creating a child-safe practice. The practice acknowledges its duty to respond appropriately to any suspicions, allegations or reports of harm, exploitation, coercion and/or neglect and abuse and to ensure that all employees; including, volunteers, students and contractors / temporary /locum workers, engaged in work at the practice know what to do if they have concerns about a child or young person. The practice is committed to implementing this procedure and the practices it sets out for all staff and partners and will provide learning opportunities and make provision for appropriate safeguarding children training to all staff and partners. This policy and procedure sets out for employees, volunteers, students and contractors/temporary/locum workers what to do in the event of identifying harm, exploitation, coercion and/or abuse. The term abuse includes Domestic Abuse, which is both a children and adult safeguarding concern. The practice recognise that safeguarding children is a shared responsibility with the need for effective joint working between agencies and professionals that have different roles and expertise if children are to be protected from harm. In order to achieve effective joint working there must be constructive relationships at all levels, promoted and supported by: the commitment of all staff, at all levels within the practice to safeguarding and promoting the welfare of children; clear lines of accountability within the practice for work on safeguarding; practice developments that take account of the need to safeguard and promote the welfare of children, and is informed, where appropriate, by the views of children and their families; staff training and continuing professional development so that staff have an understanding of their roles and responsibilities, and those of other professionals and organisations in relation to safeguarding children; Safer working practices including recruitment and vetting procedures; Effective interagency working, including effective information sharing. Page 6 of 51 This Policy and Procedure relates to the safeguarding of children. As defined in the Children Act 1989 and Children Act 2004, a child is anyone who has not yet reached their eighteenth birthday. There are several other key documents written specifically for doctors and General Practice including: 3.0 Safeguarding Children and Young People. A Toolkit for General Practice 2014 (Royal College of General Practitioners & NSPCC) http://www.rcgp.org.uk/clinical-and-research/clinical-resources/childrenand-young-people-toolkit.aspx Protecting children and young people. The responsibilities of all doctors. July 2012. (GMC) http://www.gmcuk.org/guidance/ethical_guidance/13257.asp Children and young people tool kit. Dec 2010. (BMA) http://bma.org.uk/practical-support-at-work/ethics/children/children-andyoung-people-tool-kit CQC registration Guidance for GPs. May 2012. (GPC, BMA). http://bma.org.uk/practical-support-at-work/gp-practices/cqc-registration WHAT IS SAFEGUARDING? A child is anyone who has not yet reached their 18th birthday. In England Safeguarding and protecting the welfare of children is defined in both The Children Act 2004 (and Section 11 Guidance) and Working Together to Safeguard Children (HM Government 2015) as: Protecting children from maltreatment Preventing impairment of children’s health and development; and Ensuring that children are growing up in circumstances consistent with the provision of safe and effective care and; Undertaking that role so as to enable those children to have optimum life chances and to enter adulthood successfully. Child Protection (Children Act 1989 Section 47) is defined as being part of safeguarding and promoting welfare. It is the term used to refer to activity taken to protect children who are suffering or at risk of suffering significant harm. Child in Need (Children Act 1989 Section 17) A child whose vulnerability is such that they are unlikely to reach or maintain a satisfactory level of health or development. A child whose health or development will be significantly impaired without the provision of services. Those who are disabled Page 7 of 51 3.1 Significant Harm Some children are in need because they are suffering, or likely to suffer, significant harm. The Children Act 1989 introduced the concept of significant harm as the threshold that justifies compulsory intervention in family life in the best interests of children, and gives local authorities a duty to make enquiries to decide whether they should take action to safeguard or promote the welfare of a child who is suffering, or likely to suffer, significant harm. 3.2 There are no absolute criteria on which to rely when judging what constitutes significant harm. Consideration of the severity of ill-treatment may include the degree and the extent of physical harm, the duration and frequency of abuse and neglect, the extent of premeditation, and the presence or degree of threat, coercion, sadism and bizarre or unusual elements as well as the protective factors in the child’s life that may promote their resilience to adverse factors. Each of these elements has been associated with more severe effects on the child, and / or relatively greater difficulty in helping the child overcome the adverse impact of the maltreatment. Sometimes, a single traumatic event may constitute significant harm (e.g. a violent assault, suffocation or poisoning). More often, significant harm is a compilation of significant events, both acute and longstanding, which interrupt, change or damage the child’s physical and psychological development. Some children live in family and social circumstances where their health and development are neglected. For them, it is the corrosiveness of long-term neglect, emotional, physical or sexual abuse that causes impairment to the extent of constituting significant harm. 4.0 ROLES AND RESPONSIBILITIES 4.1 The Local Safeguarding Children Board (LSCB) in Lancashire is responsible for developing local procedures and ensuring multi-agency training is available. It has a role in scrutinising the safeguarding arrangements of statutory agencies and promoting effective joint working. 4.2 Children’s Social Care. It is the responsibility of children’s social care to investigate cases of child protection in conjunction, and with the participation of, other agencies. They also lead the Child in Need process. Social care services work with health services, education, police, prison and probation services, district councils and other organisations such as the NSPCC, domestic violence forums, youth services and armed forces, all of whom contribute and work together to share responsibility for safeguarding children and promoting their welfare. 4.3 The Practice recognises that effective safeguarding systems are those which: Put the child’s needs first; Provide children with a voice; Promote identification of early help; Encourage multi-agency working and sharing of information. All staff in our practice recognises their responsibility to protect children and adults ‘at risk’ and keep them safe. Page 8 of 51 Simplistically this is done by following the 4 R’s Recognise – unmet needs, abuse and harm Respond – alert the safeguarding lead and/or Social Care Record – ensure records are kept up-to-date and secure Refer – share information and refer to external agencies to safeguarding and protect people from harm There is also an expectation that the practice team contribute to the ‘early help’ agenda. 4.4 Implementation of this policy It is the role of the practice manager and the practice safeguarding lead to brief staff and partners on their responsibilities under the policy, including clinical and non-clinical members of staff, sessional GP’s and new starters. In order to implement the policy and procedures the practice will: Promote the rights, freedoms and dignity of the person who has or is experiencing harm, exploitation, coercion and/or abuse. (Including Domestic Abuse). Promote the rights of all children and young people to live free from fear of harm Manage services in a way which promotes safety and prevents harm Ensure that all staff, employees, volunteers, students and others working within the practice will keep up to date with national developments relating to preventing harm, exploitation, coercion, abuse and the welfare of children and Brief the staff and partners on their responsibilities under the policy, including new starters, clinical and non-clinical members of the practice team and sessional General Practitioners. Be fully conversant with the practice safeguarding children policy, procedures and guidelines, the policies and procedures of Lancashire Safeguarding Children Board; and the integrated processes that support safeguarding including the CAF (Common Assessment Framework) process and information sharing Ensure safe recruitment practices are implemented and executed for every appointment, ensuring all necessary checks are made. For agency/locum/temporary staff the responsibility to undertake due diligence and check with the employer of the agency/locum/temporary employee remains with the practice. Ensure that safeguarding responsibilities are clearly defined in all job descriptions. Page 9 of 51 Work with other agencies and be compliant with the Lancashire Local Safeguarding Children Board procedures Be responsible for proactively determining safeguarding children training needs and facilitating meeting these needs. Appendix Two provides guidance as to the levels of training required by individual staff groups. Maintain accurate records of staff training and review it on an annual basis to provide assurances to NHS England and the CCG that practice staff are compliant with local and national policy. Act within the requirements of the Data Protection Act, 1998 and the Human Rights Act, 1998 as well as guidance issued by the GMC, NMC or HCPC regarding confidentiality Inform patients (unless it is unsafe to do so) that where a child is considered to be in danger, a child is at risk or a crime has (or may have been) committed a decision must be taken to pass any such information to another agency without the service user’s consent. Make a safeguarding referral to Children’s Social Care, using the appropriate referral mechanism, as required. Ensure that the practice team completes the practices agreed incident forms and analysis of significant events forms. [identify forms practice uses] Ensure that there is a system in place to identify children who do not attend an appointment following a referral for specialist care, so that the referrer is aware they have not attended and can take any follow up action considered appropriate to ensure the child’s needs are being met. Ensure that there is a system in place to identify children who are subject to a child protection plan or who are ‘looked after’ by the Local Authority 4.5 Responsibilities of all Doctors This GMC guidance aims to help doctors to protect children and young people who are living with their families or living away from home (e.g. children in care). It covers some areas which can be difficult and challenging for any practitioner encountering safeguarding concerns. These include: Communicating with children and young people Working jointly with other agencies Confidentiality, consent and sharing information Record keeping Child protection examinations Giving evidence in court The BMA toolkit aims to help doctors identify the key factors that need to be taken into account when facing ethical dilemmas and other complex decisions regarding children including: Assessing competence & mental capacity Parental responsibility Page 10 of 51 4.6 Role of the GP(part) 4.7 Best interests & disputes Consent and refusal Sexual activity Child protection Use of restraint Compulsory treatment for mental disorder Expected to take reasonable steps to identify the possibility of abuse and prevent it before it occurs Have a responsibility for raising concerns, sharing information and working together with statutory agencies to contribute to ‘early help’, child protection and children in need processes. Have a statutory duty to co-operate with other agencies to improve the wellbeing of children Have a duty to respond appropriately to any allegation of abuse Have a duty to refer children to social care when indicated May receive requests from other agencies such as social workers and police to share information about a child or family. Practice Safeguarding Children Lead Role Description Ensures that the Practice child protection procedures are developed, Implemented and regularly monitored and updated. Ensure that the practice meets statutory and contractual responsibilities and national and local regulatory requirements. Ensures safer recruitment procedures and working practices are followed including taking up references and Vetting and Barring checks where indicated. Act as a focus for external contacts on safeguarding children matters; Disseminate information in relation to safeguarding children to all practice members. Act as a point of contact and advice for practice members to bring any concerns that they have, to document those concerns and to take any necessary action to address concerns raised. Advise Practice members if they have concerns. Have regular meetings with others in the primary health care team including other agencies staff such as health visitors, school nurses and social workers, to discuss particular concerns about vulnerable children and families. Supports reporting and complaints procedures including ‘safe’ whistleblowing. Ensure the Practice meets medico-legal and regulatory requirements in relation to information sharing and record keeping. To seek appropriate advice and support from the local Designated professionals and/or Named GP Safeguarding Children. Lead on analysis of relevant significant events/root cause analysis. Ensures safeguarding training needs of practice staff are identified and are met in line with the intercollegiate competencies for health staff. Page 11 of 51 4.8 Facilitate access to support and supervision for staff working with vulnerable children and families and ensure they receive adequate assistance when dealing with child protection matters. Supports participation in Child Death Reviews Ensure that national and local recommendations from statutory Child Protection Case Reviews and Child Death Reviews and implemented. Have protected time and resources for appropriate training and carrying out the above duties. Designated and Named Professionals It is important that practices ensure that staff know who and how to contact the Designated and Named Professionals for Adult and Children’s Safeguarding for advice and support (see also Appendix Three for contact details of CCG safeguarding children professionals) 4.9 Individual staff members, including all partners, employed staff and volunteers. Must: Be alert to the potential indicators of abuse or neglect for children including the risk factors for abuse and be clear about how to act on concerns about a child. They must follow the referral processes in line with local guidance and be aware of and know how to access Lancashire Safeguarding Children Boards (LSCB) policies and procedures for safeguarding children which can be accessed at: http://panlancashirescb.proceduresonline.com/chapters/p_safe_recruitment .html Understand diversity, different beliefs and values and be able to treat patients fairly and equally; Take part in training, including attending regular updates so that they maintain their skills and are familiar with procedures aimed at safeguarding children; Understand the principles of confidentiality and information sharing in line with local and government guidance at: http://www.education.gov.uk/consultations/downloadableDocs/EveryChildM atters.pdf Contribute, when requested to do so, to the multi-agency meetings established to safeguard and protect children; Understand what behaviour is acceptable when working with children (see section 11); Minimise any potential risk to children. Page 12 of 51 5.0 RECOGNITION OF ABUSE Recognising child abuse is not easy and it is not our responsibility alone to decide whether abuse has taken place. However, it is our responsibility to act if we have any concerns. 5.1 Abuse and neglect: Abuse and neglect are forms of maltreatment of a child. Somebody may abuse or neglect a child by inflicting harm, or by failing to act to prevent harm. Children may be abused in a family or an institutional or community setting, by those known to them or, more rarely, by a stranger for example, via the internet. They may be abused by an adult or adults, or another child or children. (Please see the signs and indicators chart in Appendix Four. Definitions as stated within Working Together to Safeguard Children (HM Government 2010). 5.2 Physical abuse: May involve hitting, shaking, throwing, poisoning, burning or scalding, drowning, suffocating, or otherwise causing physical harm to a child. Physical harm may also be caused when a parent or carer fabricates the symptoms of, or deliberately induces, illness in a child. NB – Bruising in non-mobile babies – ‘All non-mobile children who are observed with injuries / bruises must be considered as possible subjects of non-accidental injury and referred for immediate paediatric assessment’ http://panlancashirescb.proceduresonline.com/pdfs/nspcc_bruises.pdf http://panlancashirescb.proceduresonline.com/chapters/p_recog_significant_harm.h tml#physical_abuse If a child presents with an injury it is important to note whether the injury is consistent with: The history provided The child’s developmental age (remember that developmental age is not always related to chronological age) Be alert to multiple bruises with bruising in ‘protected’ areas or unusual bruises. ‘Bruises on children’: www.nspcc.org.uk/core-info 5.3 Emotional abuse: The persistent emotional maltreatment of a child such as to cause severe and persistent adverse effects on the child’s emotional development. It may involve conveying to children that they are worthless or unloved, inadequate, or valued only insofar as they meet the needs of another person. It may include not giving the child opportunities to express their views, deliberately silencing them or ‘making fun’ of what they say or how they communicate. It may feature age or developmentally inappropriate expectations being imposed on children. These may include interactions that are beyond the child’s developmental capability, as well as overprotection and limitation of exploration and learning, or preventing the child participating in normal social interaction. It may involve seeing or hearing the ill-treatment of another. It may involve serious bullying (including cyber bullying), causing Page 13 of 51 children frequently to feel frightened or in danger, or the exploitation or corruption of children. Some level of emotional abuse is involved in all types of maltreatment of a child, though it may occur alone. 5.4 Sexual abuse: Involves forcing or enticing a child or young person to take part in sexual activities, not necessarily involving a high level of violence, whether or not the child is aware of what is happening. The activities may involve physical contact, including assault by penetration (for example, rape or oral sex) or non-penetrative acts such as masturbation, kissing, rubbing and touching outside of clothing. They may also include non-contact activities, such as involving children in looking at, or in the production of, sexual images, watching sexual activities, encouraging children to behave in sexually inappropriate ways, or grooming a child in preparation for abuse (including via the internet). Sexual abuse is not solely perpetrated by adult males. Women can also commit acts of sexual abuse, as can other children. 5.5 Neglect: Neglect is the persistent failure to meet a child’s basic physical and/or psychological needs, likely to result in the serious impairment of the child’s health or development. Neglect may occur during pregnancy as a result of maternal substance abuse. Once a child is born, neglect may involve a parent or carer failing to: Provide adequate food, clothing and shelter (including exclusion from home or abandonment); Protect a child from physical and emotional harm or danger; Ensure adequate supervision (including the use of inadequate caregivers); or Ensure access to appropriate medical care or treatment. It may also include neglect of, or unresponsiveness to, a child’s basic emotional needs. For more detailed guidance on how to recognise abuse and neglect refer to NICE guidance When to suspect child maltreatment accessed at: http://guidance.nice.org.uk/CG89 6.0 6.1 SAFEGUARDING IN SPECIAL CIRCUMSTANCES Safeguarding Children in Care (Children Looked After (CLA) by the Local Authority) It is well known that children and young people in care share the same health risks and problems as their peers, but often to a greater degree due to the impact of poverty, abuse and neglect. Children in care are among societies most vulnerable in terms of safeguarding and have poor health outcomes. The Designated Doctor and Designated Nurse for CLA hold responsibilities to improve the health and wellbeing of children in the care system and ‘on the edge of care’ e.g. care leavers. Page 14 of 51 General Practitioners and Primary Care Teams have a vital role in the identification of the healthcare needs of children and young people who are in care. The primary care record may be essential in ensuring needs are met. Practice role: 6.2 Accept any child in care as a registered patient seeking the urgent transfer of the medical records. Act as advocates for the child, contribute and provide summaries of the health history of a child who is in care, including their family history where relevant and appropriate. Ensure that referrals to specialist services are timely, taking into account the needs and high mobility of children who are looked after. Child Sexual Exploitation The recent report by the Children’s Commissioner into CSE found that over the past 20 years evidence has shown that large numbers of children are being sexually exploited in the UK. It called for urgent action to ensure practitioners recognise the many warning signs that children display when being subjected to sexual exploitation at the hands of gangs and groups and that they know how to act. Sexual exploitation of children and young people under 18 involves exploitative situations, contexts and relationships where the young person (or third person/s) receive ‘something’ (e.g., food, accommodation, drugs, alcohol, cigarettes, affection, gifts, money) as a result of them performing, and/or another or others performing on them, sexual activities. Child sexual exploitation can occur through the use of technology without the child’s immediate recognition; for example being persuaded to post images on the internet/mobile phones without immediate payment or gain. Violence, coercion and intimidation are common. Involvement in exploitative relationships is characterised by the child’s or young person’s limited availability of choice as a result of their social, economic or emotional vulnerability. A common feature of CSE is that the child or young person does not recognise the coercive nature of the relationship and does not see themselves as a victim of exploitation. Child sexual exploitation – recognised models: 1. Inappropriate relationships: Usually involving one abuser who has inappropriate power or control over a young person (physical, emotional or financial). One indicator maybe a significant age gap. The young person may believe they are in a loving relationship. 2. ‘Boyfriend’ model of exploitation and peer exploitation: The abuser befriends and grooms a young person into a ‘relationship’, then coerces or forces them to have sex with friends or associates. Sometimes this can be associated with gang activity but not always. 3. Organised/networked sexual exploitation or trafficking: Young people (often connected) are passed through networks, possibly over Page 15 of 51 geographical distances, between towns and cities where they may be forced/ coerced into sexual activity with multiple men. Often this occurs at ‘sex parties’ and young people who are involved may be used as agents to recruit others into the network. This serious organised crime and can involve the organised ‘buying and selling’ of young people by perpetrators. CSE is a form of sexual abuse. Act on your concerns in the same way as you would for other safeguarding concerns. 6.3 Fabricated or Induced Illness (FII) Fabricated or Induced Illness (previously referred to as Munchausen Syndrome by Proxy) is a rare and potentially dangerous form of child abuse in which the parent/carer fabricates symptoms in their child or induces them by a variety of means. Research has shown that the way in which a case of FII is managed can have a major impact on the outcome for the child. The key issues are to assess the impact of FII on the outcome for the child’s health and development and to consider how best to safeguard that child. This requires a clear and sound multi-agency approach, ensuring that all appropriate professionals are involved. Multi-agency guidance for managing children where FII is suspected can be found at: http://panlancashirescb.proceduresonline.com/chapters/p_fabricated_illness.html There may be a discrepancy in the clinical presentation and one or more of the following; Reported signs and symptoms only in the presence of the carer Multiple second opinions sought (other GP’s, secondary/tertiary centres) Inexplicable poor response to medication or excessive use of aids Biologically unlikely history of events even if the child has a current or past psychological condition Where a GP has concerns that a child may be subject to FII they must discuss their concerns with the Designated /Named Doctor for Safeguarding or where relevant, with the consultant providing care for the child. In all cases of suspected FII, professionals should not discuss the referral with the parents/carers until a multi-agency action plan has been agreed. A record of all discussions must be made, regardless of what action is taken, and should include an explanation as to the reasons for the decision, who is responsible for carrying out any actions agreed during the discussion and who was spoken to. Where the child is not under the care of a paediatrician, the child’s GP should make a referral to a paediatrician, preferably one with expertise in the specialism which seems most appropriate to the reported signs and symptoms. 6.4 Domestic Abuse Domestic Abuse is a complex issue. It is a serious crime that can occur across all sections of society, in all social classes and cultures and is not age specific. Although in the majority of cases it is perpetrated by men against women, men can also be victims and it can occur in same sex relationships. Page 16 of 51 The Home Office definition is: “Any incident or pattern of incidents of controlling, coercive or threatening behaviour, violence or abuse between those aged 16 or over who are or have been intimate partners or family members regardless of gender or sexuality. This can encompass but is not limited to the following types of abuse; Psychological Physical Sexual Financial, or Emotional. This definition includes issues of Forced Marriage, Honour Based Abuse and Female Genital Mutilation as well as elder abuse (Home Office, 2013). It is known that prolonged or regular exposure to domestic abuse can have a serious impact on the wellbeing and safety of children and young people. Serious Case review analysis 2005 - 2007 has shown that domestic abuse or a history of domestic abuse is a factor in 53% of serious case reviews. There is significant risk to the unborn child. 30% of domestic abuse cases start in pregnancy increasing the risk of miscarriage, stillbirth and premature birth and foetal injury. The new-born baby is at risk of injury, poor bonding and attachment and suboptimal development chances of a physical, psychological, cognitive and social nature. GP’s should be alert to the frequent inter-relationship between domestic abuse and other issues such as drug and alcohol misuse, social exclusion, homelessness, mental illness, child abuse or animal abuse. Also if signs of child abuse are evident consider if domestic abuse is occurring. Further guidance is available http://www.rcgp.org.uk/pdf/DV_practice_guidance June 2012.pdf Domestic abuse can have a devastating impact on children and young people, affecting their health, well-being and development, as well as their educational achievement. The Department of Health has undertaken significant work to promote awareness, understanding and develop evidencebased practice on domestic violence for health professionals. A comprehensive toolkit is available for frontline professionals: http://webarchive.nationalarchives.gov.uk/20130107105354/http://www.dh.gov .uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/@ps/documents/digit alasset/dh_116914.pdf 6.5 Multi-Agency Risk Assessment Conference (MARAC) This is a multi-agency meeting where information is shared about high risk victims of domestic abuse (those at risk of murder or serious harm) and has the safety of these victims at the heart. This process may give rise to safeguarding concerns for children and young people. Page 17 of 51 6.6 Honour Based Abuse/Violence In some cultural groups there may be added complexities related to domestic abuse that are termed Honour Based Abuse/Violence. Cultural issues should be recognised in situations when people from different racial groups disclose domestic abuse. Added pressures may be evident for these victims e.g. language barriers, dishonour of family, unfamiliarity with British culture, no British citizenship, no recourse to public funds and professionals should be mindful that there may be added safety factors to consider. In no circumstance should Honour Based Abuse/Violence be accepted as a cultural norm and beliefs of some people within specific groups are not an excuse for abuse. Safeguarding and protection of children and young people must still be addressed in accordance with the Lancashire Safeguarding Children procedures. http://panlancashirescb.proceduresonline.com/chapters/p_forced_marriage.ht ml 6.7 Forced Marriage Forced Marriage is not an arranged marriage. A forced marriage is a marriage where one or both parties do not give willing consent and where there is duress involved. Forced marriage is not condoned by any major religion and is considered a form of abuse. Forced marriage is recognised as an abuse of human rights and it can be categorised as domestic abuse or child abuse depending on age. Forced Marriage is not solely a problem that occurs in South Asian families and it is known to occur in families from East Asia, the Middle East, Europe and Africa. Most cases occur between the ages of 13yrs and 30 yrs. and there are as many male victims as female. Forced Marriage is abusive and when it occurs in children under the age of 18yrs it should be dealt with by following child protection procedures. However extreme caution should be exercised and expert advice sought as soon as possible by any professional dealing with cases of this nature. Forced Marriage Unit - 020 7008 0151 6.8 Female Genital Mutilation (FGM) FGM is illegal and is a form of child abuse and violates the rights of the child. FGM is the collective term for procedures which include the partial or total removal of the external female genital organs for cultural or other nontherapeutic reasons. FGM is typically performed on girls aged between 4 and 13 years of age but also at times occurs from birth or in young women before marriage or pregnancy. The Prohibition of Female Circumcision Act 1985 made this practice illegal in this country. However it was not illegal for the procedure to be performed out of the country. The Female Genital Mutilation Act 2003 replaced the 1985 Act and it is now illegal to: Perform FGM in the UK Aid, Abet, counsel or procure a non UK National to carry out FGM on girls (who are British Nationals or permanent residents of the UK) abroad. Aid, Abet, counsel or procure a girl to carry out FGM on herself Page 18 of 51 https://www.gov.uk/government/publications/female-genital-mutilation-multiagency-practice-guidelines http://www.fgmnationalgroup.org Female Genital Mutilation Prevention Programme: Requirements for NHS staff 6.9 Multi-agency Public Protection Arrangements (MAPPA) These arrangements are designed to protect the public and previous victims from serious harm by sexual and violent offenders. GP Practices may be requested to provide health information to contribute to an up-to-date risk assessment to ensure that the offender is managed appropriately. 6.10 Private Fostering Private fostering is a private arrangement made between a child’s parents and someone who is not a close relative to care for a child for 28 days or more; where the child lives with the carer. Close relatives are an aunt, uncle, brother, sister or grandparent but not a great aunt or uncle. Private fostering covers arrangements made for children aged less than 16 or less than 18 if the child is disabled. It does not mean arrangements made for children who have been placed by Children's Social Care. As private fostering is a private arrangement it can be hidden from agencies that have a responsibility to safeguard the welfare of children. Privately fostered children can be vulnerable as they may not see their families very often. It is therefore important that their needs are assessed and their situation monitored to safeguard their wellbeing. Professionals should encourage parents/carers to notify Children's Social Care of private fostering arrangements. If they feel Children's Social Care has not been made aware by parents/carers, then they should notify Children's Social Care themselves. 6.11 PREVENT ‘Prevent’ is part of the Government’s counter-terrorism strategy CONTEST, which is led by the Home Office. The health sector has a non-enforcement approach to Prevent and focuses on support for vulnerable individuals and healthcare organisations. The Department of Health and the health sector are key partners in working to prevent vulnerable individuals from being drawn into terrorist-related activities. Prevent is about recognising when vulnerable individuals are being exploited for terrorist-related activities, it follows that it is most appropriately managed within existing safeguarding structures, working closely with emergency planning. CONTEST is primarily organised around four key principles each with a specific objective: • Pursue: to stop terrorist attacks • Prevent: to stop people becoming terrorists or supporting terrorism • Protect: to strengthen our protection against a terrorist attack Page 19 of 51 • Prepare: to mitigate the impact of a terrorist attack. The Department of Health is a long-established partner in CONTEST through Prevent, Protect and Prepare. Responsibility for Pursue lies with the enforcement agencies. Prevent objectives Three national objectives have been identified for the Prevent strategy: Objective 1: respond to the ideological challenge of terrorism and the threat we face from those who promote it Objective 2: prevent people from being drawn into terrorism and ensure that they are given appropriate advice and support Objective 3: work with sectors and institutions where there are risks of radicalisation which we need to address. Prevent strategy (HM Government, 2011) www.homeoffice.gov.uk/publications/counter-terrorism/prevent/preventstrategy Vulnerability. In terms of personal vulnerability, the following factors may make individuals susceptible to exploitation. None of these are conclusive in themselves and therefore should not be considered in isolation but in conjunction with the particular circumstances and any other signs of radicalisation. Identity crisis Personal crisis Personal circumstances Unemployment or under-employment Criminality Evidence suggests that: There is no obvious profile of a person likely to become involved in terrorist related activity, or single indicator of when a person might move to support extremism Vulnerable individuals who may be susceptible to radicalisation can be patients and/or staff Radicalisers often use a persuasive rationale or narrative and are usually charismatic individuals who are able to attract people to their cause which is based on a particular interpretation or distortion of history, politics or religion Raising concerns: Should any staff member have a concern relating to an individual’s behaviour which indicates that they may be being drawn into terrorist-related activity, they will need to take into consideration how reliable or significant these indicators are. Indicators may include: Page 20 of 51 graffiti symbols, writing or artwork promoting extremist messages or images patients/staff accessing terrorist-related material online, including through social networking sites parental/family reports of changes in behaviour, friendships or actions and requests for assistance partner healthcare organisations’, local authority services’ and police reports of issues affecting patients in other healthcare organisations patients voicing opinions drawn from terrorist-related ideologies and narratives use of extremist or hate terms to exclude others or incite violence. It may be that a patient or staff member is facing multiple challenges in their life, of which exposure to terrorist-related influences is just one. Healthcare workers will need to use their judgement in determining the significance of any changes in behaviour where sufficient concerns are present. These should be reported in accordance with the Practices policies and procedures. Concerns that an individual may be vulnerable to radicalisation, does not mean that you think the person is a terrorist, it means that you are concerned they are prone to being exploited by others, and so the concern is a safeguarding concern. If a member of staff feels that they have a concern that someone is being radicalised, then they should discuss their concerns with their manager and the safeguarding lead. If staff suspect any such incidents they must discuss with their line manager/CCG designated nurse for safeguarding and make arrangements to report their suspicions accordingly: In an emergency 999 National Anti-Terrorist Hotline -0800 789 321 Crime stoppers - 0800 555 111 Lancashire Prevent HQ team – 01772 - 413366 /412604 / 412967 https://www.gov.uk/government/policies/protecting-the-uk-against-terrorism Further information (Toolkit): https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/ 215251/dh_131934.pdf 6.12 What to do if a child is not accessing education. Where it is discovered that a child is not receiving any form of education a referral must be made to the local authority in which the child lives. For children resident in Lancashire this is to the Nominated person for Children Missing Education. Page 21 of 51 7.0 WHAT TO DO IF YOU HAVE CONCERNS ABOUT A CHILD’S WELFARE 7.1 ACTING ON CURRENT CONCERNS (Please see flow chart Appendix Five.) You have a concern about a child: Is this a child protection issue? Do you suspect maltreatment? Has the child experienced or likely to experience significant harm? No: the child and family may still be in need of additional support. Consider, A referral to Children’s Social Care as a ‘child in need’ (Section 17) Initiating ‘CAF(Common Assessment Framework) process’ Not sure: Discuss with a senior practitioner, Safeguarding Lead or the Safeguarding Children Health Team. You can also discuss your concerns with Children’s Social Care. Ask for a “what if” (or ‘no name’) conversation with the duty social worker. Yes: A referral must be made to Children’s Social Care. Delay should be avoided. Referrals can be made by phone but must be followed up in writing within 48 hours. The link below provides more detail on the referral process. http://panlancashirescb.proceduresonline.com/chapters/p_referral_social_car e.html It is good practice to discuss your concerns with the parents at this stage unless there is a good reason for not doing so. Research shows that parents will find it easier to work with professionals to ensure the welfare of their child if they are dealt with openly from the outset. There are circumstances when speaking to parents about the concerns would place a child at increased risk of further harm. This includes: Suspected sexual abuse Suspected fabricated or induced illness Increased risk to the child Risk to workers own personal safety Female genital mutilation Forced marriage (under 18’s) Where a decision is taken not to seek parental permission before making a referral to Children’s Social Care the decision must be recorded in the child’s record and include reasons for that decision, and confirmed in the written referral. Page 22 of 51 It is the responsibility of social care to acknowledge the receipt of your referral and decide on the next course of action within one working day. This may include an assessment or they may decide that Children’s Social Care has no role at this stage. In either circumstance you should be informed of their decision. If you have not heard anything from social care it is your responsibility to chase this up. If you have a disagreement with another agency (e.g. Children’s Social Care), consider escalating your concerns. The CCG Safeguarding professionals can help with this. The link below takes you to the LSCB Escalation procedures. http://panlancashirescb.proceduresonline.com/chapters/p_resolving_prof_disa gree.html Other than in cases where it is immediately clear that a child is, or is likely to be, at risk of significant harm, you should consider discussing these concerns with the Health Visitor and/or School Nurse as they may have additional information about the child/family. The School Nurse or Health Visitor may be able to assist you in completing the CAF (Common Assessment Framework) process. 7.2 Responding to a child who tells you about abuse Whenever a child reports that they are experiencing abuse or neglect, or have caused or are causing physical or sexual harm to others, the initial response from all professionals should be limited to listening carefully to what the child says to: Clarify the concerns; Offer re-assurance about how the child will be kept safe; Explain what action will be taken. The child must not be pressed for information, led or cross-examined or given false assurances of absolute confidentiality, as this could prejudice police investigations, especially in cases of sexual abuse. If the child can understand the significance and consequences of making a referral to Children’s Social Care, they should be asked their view. However, it should be explained to the child that whilst their view will be taken into account, the professional has a responsibility to take whatever action is required to ensure the child’s safety and the safety of other children. It is important to remember that other children in the family should always be considered for assessment when abuse of one child is uncovered. (RCGP Toolkit p74) 7.3 What to do if members of the public raise concerns Members of the public may talk to GPs and their practice staff about the abuse of children known to them. They may specifically allege incidents or knowledge of abuse to a child or may refer to it when discussing other issues. The child may be well known to them, or may be the child of neighbours or others less well known. The type and nature of the abuse may be quite specific or it may be described only in very general terms. Page 23 of 51 It is important that all such allegations or references to abuse are taken seriously and relevant details should be referred to Children’s Social Care for further enquires to be made. In such circumstances, you should be clear with that person that you have a duty to report any alleged abuse, and encourage the person to make a direct referral to Children’s Social Care themselves: remember, safeguarding is everyone’s responsibility. If the member of public refuses to refer to Children’s Social Care, the professional to whom the disclosure was made has a responsibility to refer if a disclosure in respect of ‘significant harm’ has been made. It is essential that clear notes of any such allegation are kept within the child’s, parents or carers record if one is available and if possible, clarify details. These may be required at a later date. If possible take the name and contact details of the person alleging the abuse – it may be necessary for Children’s Social Care or the Police to talk to them further. It is important to note that the identity of the worker referring the concerns will be given to the family except in exceptional circumstances. Members of the public can remain anonymous if they wish. 8.0 BARRIERS TO SAFEGUARDING Safeguarding is a difficult area of practice which can present a range of challenges, both emotional and practical. Practitioners may fail to recognise, underestimate or even condone the problem. Stemming from a desire to help, professionals can sometimes overidentify with the abusing parent to the detriment of the child or find it hard to 'think the unthinkable', seeking more comfortable explanations for what they see (Rule of Optimism). Often the needs of the child are overshadowed by those of the parents. Parents can be very effective at deflecting the attention from the real problem or presenting a picture of change when in fact there is none (disguised compliance). Decisions to act may be hindered by perceived or actual problems in the child protection system. Disagreements can arise between agencies about the best course of action for a child. Practice staff may lack confidence that concerns will be taken seriously based on past experience. If you encounter any barriers it is important to act to resolve them, either through discussion within the team or by seeking advice. The CCG Safeguarding Team can help you. For example, escalating cases with Children's Social Care, tackling systemic problems or helping you to address a practice issue. 9.0 INFORMATION SHARING Keeping children and young people safe from harm requires professionals and others to share information about their health and development and exposure to possible harm. Often, it is only when information from a number of sources has been shared and pulled together that it becomes clear that there are concerns a child is in need of protection or services. Sharing of information is vital for early intervention to ensure that children and young people with additional needs get the services they require. It is also Page 24 of 51 essential to protect children and young people from suffering harm from abuse or neglect. It is essential that all practitioners understand when, why and how they should share information. It is important of course to keep a balance between the need to maintain confidentiality and the need to share information to protect others. Decisions to share information must always be based on professional judgement about the safety and wellbeing of the individual and in accordance with legal, ethical and professional obligations. Always consider the safety and welfare of the child or young person when making decisions on whether to share information about them. Where there is concern that the child may be suffering or is at risk of suffering significant harm the child’s safety and welfare must be the overriding consideration. Information may also be shared where an adult is at risk of serious harm, or if it would undermine the prevention, detection, or prosecution of a serious crime including where consent might lead to interference with any potential investigation. The 7 key points on information sharing and a flowchart are found in Appendix Six. Further detailed guidance please refer to Information sharing: Advice for Practitioners (HM Government 2015) accessed at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/4 19628/Information_sharing_advice_safeguarding_practitioners.pdf See also GMC ‘Protecting Children and Young People (2012). 10.0 GP ATTENDANCE AT CASE CONFERENCES The contribution of GPs to safeguarding children is invaluable and priority should be given to attendance wherever possible. A written report should be made available for the conference, whether or not the GP will be in attendance. (GMC, Child Protection Guidance 2012). The report will inform the child protection decision making The report should provide details of the GPs/Practices involvement with the child and family, and their assessment of the capacity of the parents to meet the needs of their child within their family and environmental context. The report must make it clear the distinction between fact, observation, allegation and opinion. When information is provided from another source, this should be made clear. It is recommended that the report is shared with the family prior to conference. 11.0 RECORDING INFORMATION GMC 2013 Guidance Good Medical Practice ( http://www.gmc-uk.org/guidance/good_medical_practice.asp ) states: - ‘Documents you make (including clinical records) to formally record your work must be clear, accurate and legible. You must make records of the same time as the events you are recording or as soon as possible thereafter’. Records must be written in compliance with the Race Relations Act, Equality Act and Disability Discrimination Act and should provide evidence of history, Page 25 of 51 examination and interventions including any management plans, medication prescribed, other care delivered. If any information is shared the reason for this, who it has been shared with and whether it has been shared with or without consent must be recorded including the rationale for decisions made. Where there are concerns about a child’s welfare, all concerns, discussions about the child, decisions made and the reasons for those decisions must be recorded in writing in the child’s records, and where appropriate, the notes of siblings and significant adults. Any bruises, marks and/or injuries observed should be clearly documented on a body map within the records. To assist in recording information about vulnerable children the following additional guidance is given: Information that must be recorded in the notes includes: That supplied by all members of the primary care team, including the Health Visitor/School Nurse, should be recorded in the notes. Conversations with, and referrals to, outside agencies are recorded in the notes of the child and relevant adults. Legal status of the child – such as a child subject to a Care Order under the Children Act 1989 Where it is considered that a child is subject to fabricated or induced illness (FII) If a child is subject to a child protection plan. All child protection conference notes are to be retained, although it is up to individual practices to determine the most practicable way to retain this information it is suggested that it is scanned into the notes of all children and adults (where registered with the practice). If a child is no longer subject to a child protection plan. This information should also be recorded in the notes of the parents/carers where they are registered with the practice. Recording when a child is considered to be a ‘vulnerable’. It is good practice to always record: The name of the professional seeing the patient as well as the date and time Who attends with the child and their relationship with that child (if any) The use of email or unlinked correspondence is discouraged other than for the purpose of alerting individuals to new information in notes. Records, storage and disposal must follow national guidance, for example Records Management, NHS Code of Practice 2006. For electronic records see also https://www.gov.uk/government/publications/the-good-practice-guidelines-forgp-electronic-patient-records-version-4-2011 If information is about a member of staff this is recorded securely in the staff personnel file in line [insert practice guidance] Page 26 of 51 Regulated practitioners must also have regard to their regulatory body guidance, for example, Nursing & Midwifery Council Record Keeping Guidance 2009; General Medical Council , Good Medical Practice (2013). 11.1 Identifying those with Potential Safeguarding Concerns - Coding Practice computer systems are used to identify those patients and families with risk factors or concerns and especially when the patient or their family consults a range of practitioners. The Practice will: Have someone who is responsible for putting the alerts on the computer Use the computer alert system Use a standard set of Read codes It is important to be alert to the siblings and other members of the household as the child there are direct concerns about. Detailed instructions from EMIS on how to set up alerts are available: Title: TH869 EMIS Web Patient warnings Details on practice records and coding can be found in the RCGP/NSPCC Toolkit 2014. http://www.rcgp.org.uk/clinical-and-research/clinicalresources/~/media/54D5AE22B3A14BAF9A92DB25D125DBAF.ashx 12.0 CREATING A SAFE ENVIRONMENT 12.1 Safer Employment The aim of creating a safe environment is to minimise risks to children and young people from abuse in practice. We sometimes need to be mindful that there may be people who work, or seek to work, in organisations who pose a risk to children and young people. The following is intended to further support practices in creating a safer environment by setting out key safeguarding arrangements that help to protect patients as well as protecting individuals against false allegations of abuse and the reputation of the practice and professionals. The Criminal Records Bureau (CRB) and Independent Safeguarding Authority (ISA) functions have now merged to create the Disclosure and Barring Service (DBS). All GPs applying to join the medical performers list under Performers List Regulations have to provide an enhanced disclosure as part of their application. General practices also have a responsibility to ensure that they carry out appropriate criminal record checks on applicants for any position within their practice that qualifies for either an enhanced or standard level check. Any Page 27 of 51 requirement for a check and eligibility for the level of check is dependent on the roles and responsibilities of the job. NHS employers also have a legal duty to refer information to the DBS if an employee has harmed, or poses a risk of harm, to vulnerable groups and where they have dismissed them or are considering dismissal. This includes situations where an employee has resigned before a decision to dismiss them has been made. For further information: http://www.homeoffice.gov.uk/agencies-public-bodies/dbs or http://www.nhsemployers.org/RecruitmentAndRetention/Employmentche cks/Pages/Employment-checks.aspx Safer employment extends beyond criminal record checks to other aspects of the recruitment process including: 12.2 Making clear statement in adverts and job descriptions regarding commitment to safeguarding Seeking proof of identity and qualifications Providing two references, one of which should be the most recent employer Evidence of the person's right to work in the UK is obtained Staff Behaviour and Professional Boundaries: The practice should have clear expectations for staff behaviour e.g. attitude. The following list is by no means exhaustive and all staff should remember to conduct themselves in a manner appropriate to their position. Wherever possible, you should be guided by the following advice. If it is necessary to carry out practices contrary to it, you should only do so after discussion with, and the approval of, your manager/General Practitioner. You must: challenge unacceptable behaviour and report all allegations; provide an example of good conduct you wish others to follow; respect a young person’s right to privacy and encourage children, young people and adults to feel comfortable to point out attitudes or behaviours they do not like; involve children and young people in decision-making as appropriate; be aware that someone else might misinterpret your actions; not engage in or tolerate bullying of a child, either by adults or other children; never promise to keep a secret about any sensitive information that may be disclosed to you but follow the practice guidance on confidentiality and sharing information; never offer a lift to a young person in your own car unless in an emergency; never exchange personal details, such as your home address with a young person; Page 28 of 51 not engage in or allow any sexually provocative games involving or observed by children, whether based on talking or touching. Detailed guidance on safe working practices for adults who work with children can be accessed at: http://www.dcsf.gov.uk/everychildmatters/resources-andpractice/IG00311/ 12.3 Use of Internet, Mobile Phones and Electronic Equipment You must always act responsibly with regard to internet, electronic and telecommunications equipment (including use of mobile phones), using them in a professional, lawful and ethical manner. 12.4 Inappropriate types of Web sites Accessing or downloading data from inappropriate websites (e.g. pornographic websites or emails, racist, sexist or gambling websites or emails, sites promoting violence and illegal software) at any time is forbidden and may lead to disciplinary proceedings. 12.5 Managing allegations against workers who have contact with children. Children can be subjected to abuse by those who work with them in any and every setting. All allegations of abuse or maltreatment of children by an employee, agency worker, independent contractor or volunteer will be taken seriously and treated in accordance with the Safeguarding Children Board (LSCB) procedure for Managing allegations against people who work with children and young people, accessed at: http://panlancashirescb.proceduresonline.com/chapters/p_allegations.html The procedure must be followed when there are concerns that any person who works with children, either in a paid or unpaid capacity i.e. any employee, independent contractor, or volunteer, where the adult is in a position of trust in relation to the child and family, has: behaved in a way that has harmed a child, or may have harmed a child possibly committed a criminal offence against or related to a child behaved towards a child or children in a way that indicates s/he is unsuitable to work with children. These behaviours should be considered within the context of the four categories of abuse i.e. physical, sexual and emotional abuse and neglect and includes concerns relating to inappropriate relationships between members of staff and children or young people. Compliance with the above procedure allows for consideration of the adult’s behaviour at the earliest opportunity when a concern or allegation arises. Compliance also helps to ensure that allegations of abuse are dealt with expeditiously and in a manner that is consistent with a thorough and fair process. If a serious allegation is made against a member of practice staff and it relates to conduct towards a child, you must inform the Local Area Designated Officer (LADO) who is employed by the Local Authority after taking immediate action in line with your practice policy. This person assumes oversight of your investigation process from beginning to end and will give you advice. They will also liaise with the police and social care if necessary. Page 29 of 51 LADO for Lancashire Is: Tim Booth: Tim.booth@lancashire.gov.uk Tel: 01772 536694 or 07826902522 12.6 Whistle-Blowing It is important to build a culture that allows practice staff to feel comfortable about sharing information, in confidence and with a lead person, regarding concerns about quality of care or a colleague’s behaviour. This will also include behaviour that is not linked to child abuse but that has pushed boundaries beyond acceptable lines. http://proceduresonline.com/panlancs/scb/chapters/p_whistle_blowing.html 12.7 Complaints procedure The practice has a robust mechanism for of dealing with complaints from all patients (including children and young people), employees, accompanying adult or parent. Please refer to [insert link or cite practice document]. Consideration should always be given to whether a complainant meets the criteria for managing allegations procedures. 12.8 Consent Guidance and Procedure The practice has a clear consent guidance and chaperone procedure which all practitioners are aware of. Please refer to (insert links or cite practice documents). If a child refuses treatment, consideration should be given as to whether the child is ‘Fraser competent’ see practice consent guidance (cite appropriate section in practice consent guidance) for further detail. Under no circumstances should children be restrained by practice staff in order to administer medication / treatment. 12.9 Serious Untoward Incidents The practice has a robust system for recording serious untoward incidents and procedures for undertaking investigations. These may be in the form of a significant event analysis. 12.10 Training To protect children and young people from harm, all health staff must have the competences to recognise child maltreatment and to take effective action as appropriate to their role. The training framework at Appendix Two indicates the level of training required by different members of the practice. All staff undergoing training are expected to keep a learning log for their appraisals and/or professional development. 12.11 Supervision of staff Staff working with children, young people and families to have access to support and supervision; this will provide an opportunity for practitioners to share their concerns and to enable them to manage the stresses inherent in this work. It also promotes good standards of practice, which are soundly Page 30 of 51 based and consistent with local and national guidance for safeguarding children. It also provides an opportunity to ensure there is an understanding of roles and responsibilities, as well as the scope of professional discretion and authority. Key decisions taken during supervision must be recorded in the child’s records. 13.0 Safeguarding Children Processes 13.1 Common Assessment Framework (CAF) The Common Assessment Framework is a key tool in the early identification of children and young people and families who may experience problems, require additional support or who are vulnerable to poor outcomes and underpins the work of Early Support. Further details can be found via the link below which also links to the current Lancashire Thresholds Guidance http://lancashirechildrenstrust.org.uk/resources/?siteid=6274&pageid=45056 13.2 Domestic Homicide Reviews Domestic Homicide Reviews (DHRs) were established on a statutory basis under section 9 of the Domestic Violence Crime and Victims Act 2004. This provision came into force on 13th April 2011. All heath organisations are obliged to participate in these reviews. Therefore, this practice acknowledges this obligation and will contribute in the same way as it does during the serious case review process. 13.3 Serious Case Reviews Regulation 5 of the Local Safeguarding Children Boards Regulations (2006) sets out the functions of LSCB’s including a requirement to carry out serious case reviews in specific circumstances. This includes undertaking a serious case review for every case where abuse or neglect is known or suspected and either: A child dies; or A child is seriously harmed and there are concerns about how organisations or professionals worked together to safeguard the child. The Regulation can be read in full by following the link below. http://www.legislation.gov.uk/uksi/2006/90/regulation/5/made The GP Practice will work with the Local Area Team (LAT) and Designated professionals to contribute in full to the serious case review process. 13.4 Child Death Overview Panel (CDOP) The Child Death Overview Panel (CDOP) is a multi-agency group which reviews all child deaths up to the age of 18 years. It is a sub-group of the Local Safeguarding Children Board. Since April 2008 it has been a statutory requirement to notify all child deaths to a central point, regardless of the age of the child or the cause of death. Page 31 of 51 Anonymous data is collected on all child deaths including expected deaths. The information collected needs to be as complete as possible (particularly when the death was unexpected) in order to ascertain whether there are any modifiable factors. The CDOP makes recommendations when there are lessons to be learned, and informs local planning on how best to safeguard and promote the welfare of children in their area. The panel is also responsible for ensuring that follow-up and support for families is in place. When a child’s death is Unexpected (i.e. the death was not anticipated as a possibility 24 hours before the death or the event that preceded the death), there is an immediate information sharing and planning discussion between the lead agencies (Health, Police and Social Care) and usually there will be a joint home visit between a police officer and a senior health professional (Rapid Response Team) to take a detailed history from the family and also to keep the family informed about the next steps. This visit is made as soon as possible within working hours and the information is passed onto the pathologist when a post mortem is to be held. A multi-agency professionals meeting is then held, usually within a few days of the death, involving relevant agencies (e.g. primary health care, midwives, coroner’s office, police, paediatrician, education). The purpose of this meeting is to share information, to raise concerns about whether there is a possibility of abuse or neglect having contributed to the child’s death and to ensure that the family are supported. GPs are expected to contribute to the CDOP process by completing a ‘Form B’ on request. 14.0 REVIEWING THE PRACTICE SAFEGUARDING GOVERNANCE ARRANGEMENTS There are several ways in which the practices safeguarding arrangements can be reviewed. The RCGP/NSPCC toolkit suggests steps to help you prioritise tasks based on self-audit and/or risk assessment. It includes information on many of the areas key to establishing effective arrangements, including an audit tool and templates for reviewing significant events. Be aware of, understand and recognise child abuse Develop and maintain a culture of openness and awareness Identify and manage the risks and dangers to children and young people in your practice and activities: Health & Safety Executive. http://www.hse.gov.uk/index.htm Develop a child protection policy: Toolkit for GPs, p10 Create clear boundaries, for example, with the limits to confidentiality: BMA Toolkit, p7 &15 Page 32 of 51 Follow safe recruitment practice including obtaining references for all team members Support and supervise staff and volunteers Ensure there is a clear procedure for addressing concerns Know your legal responsibilities: Toolkit for GPs, p7, GMC Guide, p6-8 Have a practice policy which welcomes and encourages children and young people to participate in your practice: “Involving children and young people in health services”. NHS Confederation & RCPCH 2011. Provide safeguarding education and training to all members of the team. 15.0 CQC GUIDANCE Outcome 7 of the essential standards relates to safeguarding patients (children and adults) from abuse. Staff should be in a position to identify abuse and act appropriately in cases of alleged or suspected abuse. Your practice is likely to be compliant if it does the following: Ensures that staff have safeguarding training, appropriate to their role, so that they can recognise the signs of possible abuse. Takes appropriate action to protect patients in the event that any member of staff exploits a vulnerable adult or child in any way. Healthcare professionals in GP practices should be reported to the GMC/Nursing Midwifery Council/HPC in cases where they are in possible breach of their professional guidelines. Performers should be reported to the relevant CCG/LAT. Ensures that patients can raise concerns and make complaints related to abuse. The practice should have a mechanism for patients to make comments and a publicised complaints procedure. Shares relevant information with other providers, in accordance with local safeguarding procedures, when there are safeguarding concerns about a patient. Complies with the Vetting and Barring Scheme: o Practices that knowingly employ someone who is barred to work with children or vulnerable adults will be breaking the law. o Practices that dismiss or remove a member of staff/volunteer from working with children and/or vulnerable adults (in what is legally defined as regulated activity) o Practices are under a legal duty to notify the DBA* of relevant information, so that individuals who pose a threat to vulnerable groups can be identified and barred from working with these groups. Page 33 of 51 Your practice has the following: o A safeguarding children (child protection) policy o A safeguarding adults policy o A patient information leaflet about abuse, containing information on what patients should do if they have suspicions that another person has been abused and what they might expect to happen under safeguarding procedures, is available in your practice. o A range of patient information leaflets can be accessed at: http://www.safenetwork.org.uk or the NSPCC 16.0 EQUALITY IMPACT ASSESSMENT On initial screening no issues were identified that would indicate the need for a full Equality Impact Assessment. Please see Appendix One. 17.0 REFERENCE /BIBLIOGRAPHY AND USEFUL WEB LINKS In developing this guidance and procedures account has been taken of the following statutory and non-statutory guidance, best practice guidance and the policies and procedures of Blackpool Safeguarding Children Board. Statutory Guidance Department of Health et al (2000) Framework for the Assessment of Children in Need and their Families, London, HMSO Department of Health et al (2009) Statutory guidance on Promoting the Health and well-being of Looked After Children, Nottingham, DCSF publications HM Government (2010) Working Together to Safeguard Children, London, DCSF Publications HM Government (2013) Working Together to Safeguard Children, London, DCSF Publications HM Government (2015) Working Together to Safeguard Children, London, DCSF Publications HM Government (2008) Safeguarding Children in whom illness is fabricated or induced, DCSF publications HM Government (2009) The Right to Choose: multi-agency statutory guidance for dealing with Forced marriage, Forced Marriage Unit: London Non-statutory guidance BMA Child Protection Toolkit DH (Nov, 2011), Building Partnerships, Staying Safe. - The Health Sector Contribution to HM Governments Prevent Strategy. Guidance for Healthcare organisations. Page 34 of 51 https://www.gov.uk/government/publications/building-partnerships-stayingsafe-guidance-for-healthcare-organisations GMC (2012) Protecting Children and Young People. GMC HM Government (2008) Information Sharing: Guidance for practitioners and managers, DCSF publications HM Government (2015) What to do if you’re worried a child is being abused, DSCF publications RCGP/NSPCC (2014) Safeguarding Children and Young people: The RCGP/NSPCC Safeguarding Children Toolkit. Royal College Paediatrics and Child Health et al (2014) Safeguarding Children and Young people: Roles and Competencies for Health Care Staff. Intercollegiate Document. http://www.lscbchairs.org.uk/sitedata/files/Safeguarding_Children_Heal.pdf Best practice guidance NICE National Institute for Health and Clinical Excellence (2009) When to suspect child maltreatment, Nice clinical guideline 89 http://www.nice.org.uk/guidance/cg89 Guidelines Domestic Abuse http://www.nice.org.uk/guidance/ph50 Lancashire Safeguarding Children Board Policies, procedures and practice guidance and Recommendations from Serious Case Review accessed at: Website: http://www.lancashiresafeguarding.org.uk learning and Care Quality Commission BMA (2012) what is CQC Registration? Care Quality Commission (2009) Guidance about compliance: Essential Standards of Quality and Safety NHS Employment Check standards (2013) http://www.nhsemployers.org/recruitmentandretention/employmentchecks/employment-check-standards/pages/employment-checkstandards.aspx Useful links Victims of human trafficking www.gov.uk/government/publications/identifying-and-supporting-victims-ofhuman-trafficking-guidance-for-health-staff Page 35 of 51 Forced marriage www.gov.uk/forced-marriage Female genital mutilation https://www.gov.uk/government/publications/female-genital-mutilation-multiagency-practice-guidelines Advice and links for young people, parents, teachers, and organisations: www.childnet.com/sorted - a site designed by young people. www.ceop.gov.uk – Child Exploitation and Online Protection. Linked to a Virtual Global Taskforce, enabling police to investigate reported, actual or attempted abuse. www.iwf.org.uk – the Internet Watch Foundation. Hotline for reporting illegal online content. www.digizen.org – information about the safe use of social networking sites The responsibility for ensuring policies are reviewed belongs to the partners, who may delegate this responsibility [insert name here]. We have reviewed and accepted this guidance and procedure. Signed: Dated: Signed by on behalf of the partnership The practice team have been consulted on how we implement this guidance and procedure. Signed: Dated: Appendix One Page 36 of 51 CHCT/Safeguarding Business Case 2014 Yes Equality Analysis Checklist Does the ‘Activity’ being considered for equality analysis affect service users, employees or the wider community and therefore potentially be highly significant in terms of equality? (Relevance will depend not only on the number of those affected but also by the significance of the effect on them) Is it a major ‘Activity’ with significant implications for equality? E.g. a strategy, commissioning large scale programmes, care pathway redesign, building development etc No X X Has previous engagement highlighted important inequalities x for protected groups? X Does or could the ‘Activity’ affect different protected groups differently? Does the ‘Activity ‘relate to a known area of inequalities? x E.g. access issues for disabled people, services for vulnerable people. If you have answered yes to any of the questions above you need to complete an Equality Analysis. Focus attention on those aspects most relevant to equality. Which protected groups is it most relevant to? If you answered no to all of the questions above then you don’t need to undertake an Equality Analysis. *When you decide an ‘Activity’ is not relevant to equality and therefore does not require an Equality Analysis it is important to document the decision and reason for the decision. This ensures that you have not overlooked potential issues relevant to equality which could leave you vulnerable to legal challenge. Decision: Reason: This document applies to all. An equality analysis is not required. Name: Date: 27.11.14 Cathie Turner Page 37 of 51 Appendix Two Safeguarding Children and Adults Training for GP practices / Requirements and accessibility within Lancashire Introduction All Healthcare staff have a duty to safeguard and protect the welfare of children and vulnerable adults. Safeguarding children and adults training is therefore essential for all staff engaged in services for children and vulnerable adults. This document aims to provide guidance on the requirements and resources available for training in general practice. The responsibility for ensuring staff are properly trained rests with their employers. The list of individuals to whom this guidance might apply includes GP’s (Partners, Salaried GP’s, Retainers, Locums), Nurse Practitioners, Practice Nurses, Healthcare Assistants, Receptionist and Administrative Staff, Practice Managers and any other staff employed by the practice. The guidance draws on national guidance found in Working Together to Safeguard Children: A guide to interagency working to safeguard and promote the welfare of children (2013). The Intercollegiate Document Safeguarding Children and Young people: roles and competencies for healthcare staff (2014) and GMC Protecting Children and Young People: the responsibilities of all doctors (2012). GMC Guidance states General Practitioners must develop and maintain their knowledge and skills to protect children and young people at a level appropriate to their role. As per Safeguarding Children and Young People: Roles and Competencies for Healthcare Staff Intercollegiate Document (2014), all Clinical Staff working with children, young people and/or their parents/carers and who could potentially contribute to assessing, planning, intervening and evaluating the needs of a child or young person and parenting capacity where there are safeguarding/child protection concerns should be trained to level 3 competency. GP’s should make sure they are able to identify risk factors that might raise concerns about abuse or neglect of children or vulnerable adults and take the required action. All providers need to be compliant with CQC essential standards of quality and safety. Outcome 7 is safeguarding people who use services from abuse, ensuring people are protected from abuse and staff respect their human rights. The decision on the competency required of a particular staff member, employed by any GP practice, is one for each practice to take dependent upon employee roles and responsibilities, for example a Practice Nurse who works a lot with children such as administering childhood immunisations, might be required to complete level 3 training. Reaching and maintaining Safeguarding Children competencies is a statutory requirement. The following table provides detail of the recommended training options to achieve required levels of competency. The available resources are detailed on the following pages of this document. Staff Training Level Level 1 e.g Reception/Admin staff Level 2 e.g HCA, Practice Nurse Level 3 e.g GP, Nurse Practitioner, Practice Nurse Type of training recommended to achieve required levels of competency Multi Agency Training via Single Agency Training e.g E-Learning LSCB via national/local events/NSPCC/BASCPAN NO NO YES Reading/Reflective Practice NO NO NO YES NO YES YES YES YES Page 38 of 51 Safeguarding Children and Adults Training for GP practices / Requirements and accessibility within Lancashire Children Target Group Level/Group and suggested content Training opportunities available Level/Group 1 Safeguarding Children Training All non-clinical staff working in health care settings Staff groups Include receptionists, administrative staff, and maintenance staff To access training within 6 weeks of taking up post What is abuse and neglect How to recognise abuse and neglect To be able to understand the impact a parent/carers physical and mental health can have on the well-being of a child or young person, including the impact of domestic violence To be able to understand the risks associated with the internet and online social networking Appropriate action to take if an individual has concerns National Skills academy for Health Level 1 and 2 E Learning Children www.skillsforhealth.org.uk LSCB e-learning level 1 and level 2 (1 hour max) accessed via: http://www.lancashire.gov.uk/corporate/web/view.asp?siteid=3829&pageid=20832&e=e ( you will need to register on ISA training to do this) RCGP e-GP accessed at http://e-lfh.org.uk/projects/egp/index.html this training is free to all staff working in primary care, not just RCGP members Competencies should be reviewed annually as part of staff appraisal in conjunction with individual learning and development plans. Staff should receive refresher training every three years as a minimum equivalent to a minimum of 2 hours. The e-learning programme can also be accessed as part of refresher training. Level/Group 2 Safeguarding Children Training All clinical staff who have any contact with children, young people and/or parents/carers Staff groups Includes Practice Nurses / health care Documentation and information sharing Professional roles and responsibilities Impact of parent/carers physical and mental health on the wellbeing of the child in order to be able to identify a child/young person at risk Using the common assessment framework Using professional and clinical knowledge and understanding of what constitutes child maltreatment and how to recognise signs of abuse and neglect National Skills academy for Health Level 1 and 2 E Learning Children www.skillsforhealth.org.uk LSCB e-learning level 1 and level 2 (1 hour max) accessed via: http://www.lancashire.gov.uk/corporate/web/view.asp?siteid=3829&pageid=20832&e=e ( you will need to register on ISA training to do this) RCGP e-GP accessed at http://e-lfh.org.uk/projects/egp/index.html this training is free to all staff working in primary care, not just RCGP members Page 39 of 51 assistants etc. Training should be undertaken within six months of coming into post. NB: Staff are also required to have accessed level/group 1 training To be aware of the risk of Female Genital Mutilation (FGM) and be able to refer appropriately for further care and support To be able to identify and refer a child suspected of being a victim of trafficking and/or sexual exploitation To be aware of the risk factors for radicalisation and know who to contact regarding preventative action and support Acting in accordance with statutory and nonstatutory guidance and legislation Lancashire Safeguarding Children Boards LSCB policies and procedures accessed at: http://www.lancashire.gov.uk/education/safe_child_board/safeguarding_children_procedures/index.asp Competencies should be reviewed annually as part of staff appraisal in conjunction with individual learning and development plans. Staff should receive refresher training every three years as a minimum and training should be tailored to the roles of individuals. A minimum of 3 to 4 hours over three years is required. Level/Group 3 Safeguarding Children Training All clinical staff working predominately with children and or their families who could potentially contribute to assessing, planning, intervening and evaluating the needs of a child and parenting capacity where there are safeguarding /child protection concerns Staff groups include GPs and practice nurses NB: Staff in this To be able to identify possible signs of sexual, physical, or emotional abuse or neglect using child and family- focused approach To be able to know what constitutes child maltreatment including the effects of carer/parental behaviour on children and young people Identify, assess and meet the needs of children where there are safeguarding concerns The impact of parenting issues such as domestic abuse, substance misuse on parenting capacity and the interagency response Recognising the importance of family history and functioning Working with family members including the lack of co-operation and superficial compliance within the context of the role Awareness of interagency policy and national guidance, implications of legislation Advice would be that for staff requiring level 3 competency the ideal route would be by accessing the multi-agency training below. The LSCB run an extensive training programme for staff working with vulnerable children, who need to access training at levels 3 and above, details of which can be obtained via the following link: http://www.lancashire.gov.uk/corporate/web/view.asp?siteid=3829&pageid=20832&e=e The contact number for safeguarding training co-ordinator is 01772 538357 Additional resources for achieving level 3 National Skills academy for Health Level 3 E Learning Children www.skillsforhealth.org.uk RCGP website – safeguarding children toolkit ELearning for Healthcare.org.uk - in conjunction with the royal colleges. Resources and examples of reading and reflective practice which can be used to achieve level 3 Page 40 of 51 group are also required to have accessed level/group 1 and 2 training N/B Record Safeguarding activity in personal development file and practice development file Information sharing, confidentiality and consent; Remit and role of Lancs Safeguarding Children Board Interagency frameworks for safeguarding including the Common Assessment framework (CAF); Team around the Child and the role of the Lead Professional. competency if linked to personal development plan and appraisal Lancashire Safeguarding Children Boards LSCB policies and procedures accessed at: http://www.lancashire.gov.uk/education/safe_child_board/safeguarding_children_procedures/index.asp Common Assessment Framework CAF /Continuum Of Need CON training www.lancashire.gov.uk/corporate/web/?siteid=5943&pageid=33997&e=e Additional specialist competencies Interagency working Contributing to serious case reviews/critical incidents/child death overview processes Applying lessons learnt from audit and serious case reviews to improve practice Advising others on appropriate information sharing Discussions with colleagues- e.g. health visitors/school nurses/midwives about safeguarding issues can count towards level 3 training as long as the learning from this is documented (take out any patient identifying information though) as can case discussions/ significant event analyses in practice meetings. For the purposes of annual GP Appraisal and revalidation, GPs should have all the competencies at level 2 and be at or be able to demonstrate they are working towards level 3. The GMC and RCGP state that for the purposes of revalidation, GPs need to demonstrate that they are up to date and fit to practise in all aspects of their work. Level 3 describes the scope of work of GPs in relation to safeguarding children and young people. It is the responsibility of GPs to demonstrate that they maintain their competence. A GP may keep up to date in a variety of ways, for instance completing an elearning module, attending a training session in or out of practice or reading appropriate guidelines. In house training sessions arranged by practice safeguarding leads or bought into the practice is an effective way of delivering training to a group. They could simply go through their practice policy, discuss potential case scenarios or deliver a presentation. A session to discuss GMC guidance would be a good way to ensure that everyone is aware of their responsibilities. Remember to invite any locum or sessional doctors. The updated intercollegiate Document (2014) no longer defines level 3 competency as being measured in hours, but by being able to demonstrate on-going career long competence in the areas listed above. As a general rule to demonstrate you are keeping up to date will take as a minimum of 2 hours update each year. It is the responsibility of the GP, in their appraisal, to demonstrate they are competent and up to date. Case reviews and critical incident reviews can be used to show how knowledge and skills are used in Completing reports- for and attending multi-disciplinary meetings e.g. TAC meetings/ child protection conferences can count towards level 3 training, again as long as this is documented and you can show what you have learnt from it. RCGP Toolkit children and young people- Good resource for practice leads wishing to run level 3 sessions in house. Local and National Safeguarding Training Events. NICE guidance 2009 CG89 - When to suspect child maltreatment General Medical Council 2007 0-18 years: guidance for all doctors 2012 Protecting Children and Young People - the responsibilities of all doctors Information and guidance re working with children who are looked after “Promoting the health and Well-being of Looked After Children” (DH 2009) https://www.education.gov.uk/publications/standard/publicationDetail/Page1/DCSF-01071-2009 Information on domestic violence, forced marriage and honour based violence www.gov.uk Information on working with sexually active young people accessed at http://panlancashirescb.proceduresonline.com/chapters/p_sexually_active_yp.html Page 41 of 51 practice. GPs work to achieve level 3 competence within the first twelve months of practice and refresher training equivalent to a minimum of 6 hours over a three year period. Safeguarding Children and Adults Training for GP practices / Requirements and accessibility within Lancashire Adults Target Group Level/Group and suggested content Training opportunities available All clinical and nonclinical staff groups Introduction to safeguarding adult training The Lancashire Safeguarding Adults Board provide training for staff working with vulnerable adults at level 1 via E learning to access www.lancashire.gov.uk/safeguardingadults follow information for professionals then training What is abuse and neglect How to recognise abuse and neglect Appropriate action to take if an individual has concerns. National Skills academy for health E learning at level 1 www.skillsforhealth.org.uk Refresher training at a minimum every three years. The e-learning programme can also be accessed as part of refresher training. All clinical staff i.e. GP’s /nursing staff / health care assistants etc What is abuse and neglect Link to the Pan Lancashire and Cumbria multi agency Safeguarding adult procedures manual. The manual provides information about safeguarding adults at risk of abuse and neglect and how to make a safeguarding adult alert into social care http://plcsab.proceduresonline.com/ Understanding the terms ‘vulnerable’ and adults ‘at risk’ RCGP Toolkit Vulnerable adults MCA and DOLS How to recognise potential or actual abusive situations BMA Toolkit- BMA guide for Practitioners An overview of the background legislation and guidance ELearning programme SCIE website http://www.scie.org.uk/publications/elearning/index.asp Safeguarding Adults – What you need to know Recognition of local pathways and safeguarding structures Understanding of CQC outcome 7 expectations All clinical staff Understanding the Mental capacity Act (MCA) and the Deprivation of Liberty Safeguards (DOLS) CCG Safeguarding and Mental Capacity Act standards for commissioned services appendix 4 safeguarding standards for GP member practices can be accessed on the CCG websites. Practice safeguarding leads and deputies may wish to arrange in house training sessions as a time effective way of delivering training to a group. They could simply go through their practice policy, discuss potential case scenarios or deliver a presentation. Try to remember to invite any locum or Page 42 of 51 All staff Awareness of the legal framework underpinning the mental capacity Act 2005 and the Deprivation of Liberty safeguards Roles and responsibilities in respect of this legislation Guidance on completing capacity assessments and applying the best interests check list What makes a restriction a deprivation? Awareness of the role of the Independent mental capacity Advocate (IMCA) sessional doctors. PREVENT Health WRAP training Currently this is only available as face to face training: LEARNING OUTCOMES How to support and redirect individuals with vulnerability How to share concerns, get advice, and make referrals Please contact : Regional PREVENT Coordinator (North West) NHS England North Rm 206, Preston Business Centre, Watling St Rd, Fulwood, Preston, PR2 8DY Mob: 07900 715497 Guidance- Building Partnerships, Staying Safe: guidance for healthcare organisations at https://www.gov.uk/government/publications/building-partnerships-staying-safe-guidance-forhealthcare-organisations Page 43 of 51 Appendix Three Key contacts Designated Doctor CCG Dr (Designated Doctor) Address: Phone (Sec) Designated Nurse Tel: Mobile : Tel: Mobile : CCG Named Safeguarding CCG Professional Children and Primary Care Safeguarding Practitioner CCG Children and Primary Care GP Lead Children Chief Nurse Safeguarding Tel: Mobile : CCG Dr Dr CCG (Chief Nurse) SecretaryTel: Page 47 of 51 Page 48 of 51 Appendix 5 What to do if you are worried a child is being abused (Abuse may take the form of physical abuse, sexual abuse, emotional abuse or neglect) Any member of staff who believes or suspects that a child may be suffering, or is likely to suffer significant harm should always refer their concerns to Children’s Social Care. (There should always be an opportunity to discuss concerns with a manager, named professional or qualified social worker, but never delay emergency action to protect a child) Are you concerned a child is suffering or likely to suffer harm, for example: You may observe an injury or signs of neglect You are given information or observe emotional abuse A child discloses abuse You are concerned for the safety of a child or unborn baby Step One Inform parents/carers that you will refer to Children’s Social Care UNLESS The child may be put at increased risk of further harm (e.g. suspected sexual abuse, suspected fabricated or induced illness, female genital mutilation, increased risk to a child, forced marriage) or there is a risk to your own personal safety. Step Two Make a telephone call to Children’s Social Care Follow up the referral in writing within 24 hours Document all discussions held, actions taken, decisions made including who was spoken to (for physical injuries document injuries observed) and who was informed Where a CAF or equivalent has been completed forward this with the written referral. Step Three Children’s Social Care acknowledges receipt of referral and decides on next course of action. If the referrer has not received an acknowledgement within 3 working days contact Children’s Social Care again. Step Four You may be requested to provide further reports/information or attend multi-agency meetings Who to contact in Children’s Social Care Lancashire Duty Social Worker (Mon – Fri 8.45am – 5pm) Tel 0300 123 6720 Emergency Duty Team (out of hours) Tel 0300 123 6720 Who to contact for local NHS advice: Designated Nurse for Safeguarding Children for the (-------------) Clinical Commissioning Group: Tel: Who to contact in the Police Public Protection Unit Tel: 0845 125 35 45 and request to speak to the PPU for the area in which the person resides In an emergency contact the police on 999 Staff should update their knowledge by accessing regular training and be familiar with local safeguarding policies, including those of the Local Safeguarding Children Board. Possible signs and indicators of abuse and neglect can be found overleaf. Page 49 of 51 Appendix 6 Page 50 of 51 Page 51 of 51