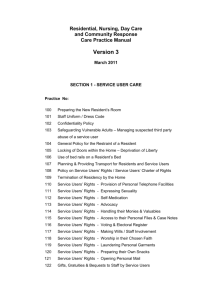
policies and procedures manual
advertisement

8333 Lewinsville Road POLICIES AND PROCEDURES MANUAL TABLE OF CONTENTS ACTIVITIES PROGRAM ............................................................................................................................... 5 BURIAL POLICY .......................................................................................................................................... 7 CONFIDENTIALITY ..................................................................................................................................... 8 Disclosure of Personal Health Information ........................................................................................... 8 Procedures to Protect Confidentiality .................................................................................................. 8 CONTROLLED SUBSTANCE MANAGEMENT............................................................................................. 12 Controlled Substance Destruction Report .......................................................................................... 13 DEATH OF A RESIDENT ............................................................................................................................ 14 DISPOSAL TECHNIQUES........................................................................................................................... 15 Sharps.................................................................................................................................................. 15 Unused Meds and Dropped Pills ......................................................................................................... 15 DOCUMENTATION .................................................................................................................................. 16 Documentation Management............................................................................................................. 16 Record Retention Policy ...................................................................................................................... 19 ELOPEMENT PROCEDURES...................................................................................................................... 19 Initial Assessment ............................................................................................................................... 20 Prevention ........................................................................................................................................... 20 Intervention ........................................................................................................................................ 20 Documentation ................................................................................................................................... 22 Elopement Drills .................................................................................................................................. 22 EMERGENCY DATA PACKETS FOR RESIDENTS......................................................................................... 23 EMERGENCY PREPAREDNESS AND DISASTER PLANNING ....................................................................... 24 House Alarm System ........................................................................................................................... 24 Ejection Pumps (Ipswich and Stoneham only) .................................................................................... 25 EVACUATION POLICIES............................................................................................................................ 26 FINAL STATEMENT OF ACCOUNT ............................................................................................................ 30 GRIEVANCE/COMPLAINT PROCEDURE ................................................................................................... 31 Maryland Complaint Report Form ...................................................................................................... 33 HOT WATER LOG ..................................................................................................................................... 37 INCIDENT REPORTS ................................................................................................................................. 37 Policy ................................................................................................................................................... 37 Procedures .......................................................................................................................................... 37 Falls ..................................................................................................................................................... 38 INFECTION CONTROL POLICY AND PROCEDURES ................................................................................... 38 Hand Washing Protocol ...................................................................................................................... 39 Immunizations..................................................................................................................................... 40 Cleaning Procedures ........................................................................................................................... 41 Contact Precautions ............................................................................................................................ 42 Monitoring of Infections and Infection Control Program ................................................................... 42 Pest Control......................................................................................................................................... 43 LEVEL OF CARE WAIVERS (MARYLAND ONLY) ........................................................................................ 44 RESIDENT AGREEMENT ........................................................................................................................... 44 MEDICAL AND HEALTH EMERGENCIES ................................................................................................... 45 Medical Emergencies .......................................................................................................................... 45 Mental Health Emergency .................................................................................................................. 46 MEDICATION MANAGEMENT ................................................................................................................. 47 MISSING RESIDENT POSSESSION(S) ........................................................................................................ 51 NEGLECT, ABUSE, AND EXPLOITATION ................................................................................................... 53 Reporting............................................................................................................................................. 53 PERSONAL FUNDS POLICY ....................................................................................................................... 55 PREADMISSION REQUIREMENTS ............................................................................................................ 55 Functional Assessment ....................................................................................................................... 56 RELOCATION AND DISCHARGE ............................................................................................................... 57 Relocation ........................................................................................................................................... 57 Discharge of a Resident....................................................................................................................... 58 RESIDENT RECORDS ................................................................................................................................ 58 Documentation Overview ................................................................................................................... 58 Care Notes........................................................................................................................................... 59 Closed Resident Records ..................................................................................................................... 59 REPORTING OF ABUSE, NEGLECT, OR EXPLOITATION ............................................................................ 60 RESIDENTS’ RIGHTS ................................................................................................................................. 61 Maryland ............................................................................................................................................. 61 Virginia ................................................................................................................................................ 63 Implementation Plan .......................................................................................................................... 67 SERVICE PLANS ........................................................................................................................................ 68 SERVICES ................................................................................................................................................. 71 Meals ................................................................................................................................................... 71 Personal Care Services ........................................................................................................................ 72 SMOKING AND WEAPONS ...................................................................................................................... 74 STAFFING PLAN ....................................................................................................................................... 74 Regular Staffing ................................................................................................................................... 74 Transition Phase .................................................................................................................................. 74 Relief Staff ........................................................................................................................................... 75 Shared Administrator .......................................................................................................................... 75 QUALITY ASSURANCE PLAN .................................................................................................................... 75 USE OF MONITORING DEVICES ............................................................................................................... 76 VISITING POLICY ...................................................................................................................................... 76 EXHIBIT 1: HOW TO HAND WASH/HANDRUB? ...................................................................................... 78 EXHIBIT 2: RESIDENT AGREEMENTS........................................................................................................ 79 Virginia ................................................................................................................................................ 80 EXHIBIT 3: OUTBREAK REPORTING REQUIREMENTS .............................................................................. 87 EXHIBIT 4: DISCHARGE NOTIFICATION AND STATEMENT ....................................................................... 88 EXHIBIT 5: ELOPEMENT DRILL OR POST ELOPEMENT CHECKLIST ........................................................... 89 ACTIVITIES PROGRAM Eden Homes provides engaging activities that promote the social, physical, intellectual, emotional, and spiritual wellbeing of each resident. All staff are expected to be active participants in fulfilling this important mission. To encourage resident participation in social and recreational activities, the Activities Department shall: Provide and post a calendar of daily activities for each home with a variety of activity programs to meet the social, physical, intellectual, emotional, and spiritual needs of each resident Provide the supplies and instructions needed to successfully implement the programs on the monthly calendar Provide or arrange for transportation to social and spiritual activities and outings in accordance with each resident’s service plan Lead regular group and individual activity programs in each home, based on the interests and needs of the residents Document the participation of residents in group and individual activity programs using proper documentation methods Keep activity supplies and areas well-maintained and in neat and tidy order Participate in Service Plan Meetings to address the social, recreational and spiritual needs of each resident Work with the Assisted Living Manager, Registered Nurse, and all house staff to assist a resident with communication, interpersonal, and social skills, including managing difficult behaviors in accordance with the resident’s service plan. All staff is expected to contribute to the social, physical, intellectual, emotional, and spiritual wellbeing of the residents. Therefore, all staff is expected to participate in recreational activities for the residents. In order to assist in the delivery of quality activity programs for our residents, staff will: Inform all residents of upcoming activities, giving the residents the choice to attend Safely assist residents to the appropriate area where an activity will take place Ensure that at least one floor staff member stays with the residents in every activity Assist with resident needs during activity program (e.g. toileting, providing snacks, etc.) Minimize distractions and noise during programming Lead activity programs as designated by the posted calendar, making an effort to actively engage each resident without coercing their participation Document each resident’s participation in activity programs using proper documentation methods (an on-line feedback form is available on the Activities page of the Eden Homes intranet) 5|Page 4/14 Encourage residents to keep up with meaningful life skills (e.g. setting the table, folding laundry) as appropriate Facilitate conversation and individual or small group activities during quiet times for residents who are awake and alert Provide feedback to the Activities Department regarding the quality of activities, resident participation, etc. Keep activity supplies and areas well-maintained and in neat and tidy order (including informing the Activities Department when additional supplies are needed) Participate in ongoing trainings about the value of activities and engagement for our residents Staff are further expected to familiarize themselves with the resources provided by the Activities Department and to use them appropriately. These include, but are not limited to: The “Green” Activity Book – A green-colored binder of pre-printed activities with instructions that are rotated monthly. Activities that can be found in the Green Book are notated in green with an asterisk next to them on the monthly calendar (e.g. 3:30p Front Porch Travels*) Conversation Cards – Biographical cards about each residents with sample questions to ask that resident. These are found in a decorative box in the dining room and should be used to get to know the residents and to start conversations during quiet times, especially after meals. Master Activity Binder – A light-blue binder with information and instructions on how to do all of our regularly scheduled programs (e.g. bingo, exercise, Shabbat, movie matinee, etc.). Used to provide guidance on all activities that are not found in the Green Book. Daily Chronicles Binder – An orange binder used for the morning “Daily Chronicles” activity, which includes facts and trivia about the current day and season. The Activity Director shall prepare and post a calendar of all scheduled recreational activities each month. This calendar will be posted conspicuously, so that residents and families can easily read it. The activities calendar is also available at all times on the company’s website at www.edenhomesgroup.com. The facility will provide activities programming using its staff, activities personnel or outside contractors each day of the week. Generally, there will be at least three activities planned for each day to including, but not limited to, morning current events, exercise, afternoon programming and, as dictated by the residents’ schedules, an evening activities. Additionally, using the conversation cards and other tools provided by the Activities Department, the staff shall engage in one-to-one conversations and other activities with the residents throughout the day. This policy meets the requirements of Maryland COMAR 10.07.14.20 and 22 VA 40-72-520 6|Page 4/14 BED HOLD POLICY Eden Homes will hold a bed pursuant to the terms of the Resident Agreement. Without limiting the specific language of the Agreement, in general, no bed will be held without payment for the same. Except in the case of a medical emergency, residents are required to give written notice of their intention to vacate a unit for any reason. Payment is expected through the date of the termination. If a resident is away from the house on a temporary basis (for example hospitalization, vacation, etc.) payment for the days absent is required. For more details, residents should refer to sections 6 and 26 of the Resident Agreement. BURIAL POLICY The staff member at Eden Homes in charge of move-ins shall use their best efforts to determine and document within 14 days of admission of the resident: Any arrangements (financial, religious, name of preferred funeral director, if any, etc.) the resident has made, or wishes to make, with regard to burial, and The name, address, and relationship of any person who has agreed to claim the body of the resident and of who has agreed to assume funeral or burial responsibility. Included in the large marketing folder for potential residents is a letter describing the importance of this information as well as a form on which the family can indicate their preferences. When complete, this information should be retained in the Resident Book. On the death of a resident, the assisted living manager should refer to this form to know who to contact. If the form indicates that no decision had been made, the assisted living manager should contact the POA or resident representative. In the event of an individual who appears to be an unclaimed deceased resident, the assisted living manager or designee shall contact any person who, although not having been identified in advance as being responsible for the burial arrangements, might nevertheless at the time of death be willing to claim the body and assume responsibility. This section meets the requirements of MD COMAR 10.07.14.30 7|Page 4/14 CONFIDENTIALITY Our residents have the right to privacy, confidential care and protection of health information. Our policy is that all information concerning our residents is kept confidential. This includes, but is not limited to, maintaining an individual’s record in a manner that ensures security and confidentiality. Records include, among other items: Pre-admission Assessments Medical Orders Rehabilitation Plans Service Plan Weekly Care Notes Emergency Data Sheet Employees have a legal and ethical responsibility to protect privacy, confidentiality and security of all medical records and personal health information, including a resident’s identity. Employees who do not comply with the confidentiality policy are subject to disciplinary action. Disclosure of Personal Health Information A resident’s health information can only be disclosed: When it will be used to carry out treatment, payment, or healthcare operations, except for research information unrelated to treatment When the resident or substitute decision-maker has consented and it is necessary for a lawful purpose Where it is required by law For use by coroners When it enables the Department of Health and Human Services to investigate or determine the covered entity’s (CE) compliance with HIPAA regulations Only the minimum amount of personal health information necessary to accomplish the allowed purpose may be disclosed. Procedures to Protect Confidentiality Release of Information The resident’s right to authorize release of medical records is codified in many state statutes. These statutes state that medical records are confidential and cannot be disclosed, except in specifically provided circumstances. The extent of the resident’s right to access varies from state to state. 8|Page 4/14 Generally, the authority to release medical information is granted to: The resident (if a competent adult or emancipated minor) The resident’s legally-designated surrogate decision maker A legal guardian The Administrator or executor of the resident’s estate, if the resident is deceased The following guidelines should be followed when releasing records: Records may only be released upon written authorization of the resident or their appropriately designated Power of Attorney The name of the person or entity receiving records and the date of release must be documented Originals are not to be released unless originals are specifically ordered by a court of law Records that are involved in potentially or actively litigious situations are separated from other medical records and maintained in a secured area Release of records should not be denied for non-payment of the resident’s bill Procedures should be developed for managing subpoena and court orders When a resident is hospitalized or tansported by emergency medical personnel, information necessary to the care of the resident (such as medications, advance directives, and organ donation) shall be furnished to the hospital or emergency medical personnel. The staff can print an Emergency Data Sheet from ICareManager to meet this requirement. Staff is encouraged to use the form, Authorization for Release of Confidential Information, found on the Forms page of the Eden Homes intranet. Otherwise, any form received from another party must include the information listed above. There are certain circumstances under which medical information must be disclosed without resident authorization. In general, these include court orders, subpoena, lawful search warrant, and notice to appear. In Virginia, information can also be released to authorized representatives of the Department of Social Services. If you are unclear as to the appropriateness of a request, please ask the House Manager. Storage All personal and medical records of a resident must be kept in secured areas that are not accessible to anyone other than employees. Conversations in the House All staff must exercise caution in the discussion of any personal health matters with residents, physicians, family members or other staff. Any medical discussion, consultation, examination or treatment of a resident is: 9|Page 4/14 Confidential To be done discretely Not open to an individual who is not involved directly in the care of the resident, unless the resident or the resident’s representative permits the individual to be present. Sensitivity is required when discussing resident matters on the telephone or in person within hearing distance of others so that conversations are not overheard E-mail and Technology E-mail communication may be protected by: Turning off computer screens or logging off when staff is not in immediate attendance Double-checking the address of the recipient is correct prior to sending an e-mail Providing all employees with computer passwords, login, and user identification and requiring that they not be shared Not permitting staff to e-mail PHI that has a potential for breaching the resident’s confidentiality Securing the storage of all hard drives and computer disk files Maintaining a secure configuration of the system (intranet and extranet) Installing and configuring wireless network connections in a manner that protects system access Voice Messaging The use of voice messages must be confirmed directly with the resident’s family prior to using this method of communication. The resident or name of family member providing confirmation is to be documented in the resident record The name of the facility and the name of the person that is being contacted may be left in the voice message provided the resident/family has consented to communication by voice messaging Messages should not contain any health information such as tests, current condition, or other personal matters including any details regarding billing information Faxing The use of a fax for Personal Health Information is permitted only when delivery by regular mail does not meet time-sensitive needs of the sender or recipient. When PHI information is transmitted by fax, the following measures must be taken: Faxing to mail rooms is not permitted 10 | P a g e 4/14 A confidentiality statement is required on the fax cover sheet. Please use the fax cover sheets available on the Eden Homes intranet for all faxes. Separate forms are available for Virginia and Maryland. Other cover sheet information is to include: o Name of the intended recipient o Business affiliation o Telephone number o Fax number o Number of pages contained in the transmission Fax confirmation sheets are attached to and maintained with all faxed materials Receipt of information acknowledgment is requested (e.g., call after receipt) A hard copy is sent to follow electronic results Faxing is not permitted for records or information that requires additional confidentiality measures including: o Substance abuse o Mental health treatment o Psychiatric residents o HIV testing Receiving Faxes Employees are to take steps to minimize the possibility that received faxes are viewed or received by someone else, including: Machines that receive faxes that include Personal Health Information are located in secured areas that are not accessible by anyone other than facility staff If an employee receives a fax on a machine that is not secure, the recipient immediately advises the sender that the receiving fax machine should not be used for the transmission of any further information Employees are to promptly remove incoming faxes and deliver them to the proper recipient If a fax is received and the facility is not the intended recipient, the employee immediately notifies the sender and destroy the faxed material The facility staff notifies entities that routinely send faxes if there is a change to the fax number If information is received that contains sensitive Personal Health Information, the sender is advised that the facility is not permitted to accept such information by fax transmission This section meets the requirements of MD COMAR 10.07.14.27 and 22 VAC 40-72-570 11 | P a g e 4/14 CONTROLLED SUBSTANCE MANAGEMENT All drugs considered Controlled Substances are required to be kept double locked. There is a lock box in the locked medicine cabinet in which drugs can be kept. There is a locked refrigerator for drugs which require refrigeration. Also, the door to the medicine room should be kept locked unless a staff member is present (providing three tiers of control for such drugs). Controlled substances are not only pills but may include liquids. Refer to the list of Controlled Substances; all substances listed as Schedule II and III must be listed and managed pursuant to this policy. (The facility will not handle any Schedule I substances.) Upon receipt by the facility, the Med Tech or the Nurse on duty must record the name and amount received of the controlled drug to the Daily Controlled Substance Log Each shift must count the number of controlled drugs on hand at the beginning and end of the shift. This is the responsibility of the Medical Technician assigned to the shifts. Upon completion of the count, if all controlled drugs are accounted for, the incoming and outgoing Med Tech should both initial the Controlled Drug Inventory County This process should take place on each shift. If there is a problem in the count, the Delegating Nurse should be informed immediately. Controlled drugs must be properly disposed of. Only the Nurse and a predetermined witness can dispose of controlled drugs. Staff should NOT dispose of any controlled drugs. The nurse will complete the Controlled Substance Destruction Report, a copy of which can be found on the following page as well as for each house on the Eden Homes intranet under Nursing Forms. In Maryland, a copy of this report must be sent to the Division of Drug Control and the original is retained in the facility. Records are kept for five years. Any questions regarding this policy should be immediately referred to the Director of Nursing. 12 | P a g e 4/14 Controlled Substance Destruction Report Facility Name: ________________________ Director of Nursing: ______________________ Address: _______________________City: ___________________Zip: _____________ License Number (if applicable): _________________________ In Maryland, forward completed form within 10 days to: (COMAR 10.19.03.10D (2) (d)) Item No. Dosage Form Quantity Division of Drug Control 4201 Patterson Avenue Baltimore, MD 21215 Telephone: 410-764-2890 Drug Strength Prescription Pharmacy No. Resident ID Date Destroyed: ________________ Method of Destruction: ___________________________ Destroyed by: ____________________Witnessed by: __________________________________ Print Name: _____________________ Print Name: ____________________________________ Keep original for facility’s records for five years. (21CFR1304.04 (a)) 13 | P a g e 4/14 DEATH OF A RESIDENT In the event a resident passes away or dies there are certain protocols that needs to be followed to ensure uniformity of service and respect to the deceased resident and the family. Do not panic. Remain calm. Follow the procedure listed below. You are not alone and need to be strong for your other residents. Procedure: 1. 2. 3. 4. 5. Once a resident appears to be not breathing you will need to activate 911/EMS (Emergency Medical System) or call Hospice (nurse) depending on whether or not the resident is under hospice care. You need to know whether or not the resident is a “Do Not Resuscitate” (DNR) on the EMS form. This form is located in the blue emergency packets and on each chart. It must be shown to EMS when they arrive or they will resuscitate (do CPR) the resident which is the law. So please be prepared by being informed. 911 (or Hospice) will be your first phone call. EMS will assess the resident for vital signs before calling the physician to pronounce the deceased resident. The police will automatically arrive with EMS because there was a death. Once EMS confirms the resident is deceased, EMS (or the house manager) will call the funeral home on file (in the Resident Book) to pick up the body. Jonathan, the house manager and the nurse needs to be notified by the staff person in charge immediately thereafter. This is your second set of calls. Jonathan will contact the family to see if they want to view the body before the funeral home takes the body. The house manager will ensure all proper protocol was followed. The nurse will assess to ensure all the above was done and that the other residents and staff member(s) on duty are okay. The house manager will arrange for the family to pick up the personal belongings when appropriate and convenient. The house manager will also notify the other residents (if appropriate) and their families and check to see if we can do anything further to assist the family of the deceased during this time. Please continue to monitor the other residents if you are the only staff person on duty (usually at night). Staff Support – please feel free to talk with any administrative person, the house manager or nurse, even another caregiver, if you feel the need to do so. A meeting can be scheduled individually or with a specific group if requested. Please do not hesitate to do so if you feel the need for further support as one of our valued staff members. We are all here to support each other during an unfortunate loss of a resident. Try to remember the good things that brought us joy to remember the resident by! 14 | P a g e 4/14 DISPOSAL TECHNIQUES Sharps “Sharps” is a medical term for devices with sharp points or edges that can puncture or cut the skin (for example, needles, syringes, lancets (for blood sugar) etc.) Used sharps are dangerous to people if not disposed of safely because they can spread infections that cause serious health conditions. We have Red Sharp containers in each house. Always dispose of used sharps in the red sharp container and be extra careful to avoid accidental “needle stick”. Never place loose needles and other sharps in the trash cans or recycling bins, and never flush them down the toilet. You must put them in the Sharp container, never put your hand inside the sharp container. In the event you are accidently stuck by another person’s used needle or other sharp, you must: Wash the exposed area right away with water and soap or use a skin disinfectant (antiseptic) such as rubbing alcohol or hand sanitizer. Seek immediate medical attention by calling your physician or going to the Emergency Room. If the sharp container is full, please notify a RN for replacement. Unused Meds and Dropped Pills It is important to dispose of medications properly when they’re no longer being used to avoid harm to others. ALM or Team Leader should remove them out of the resident’s medicine drawer and set it aside for the nurse to pick up and properly dispose of them. To comply with safety rules associated with medication disposal, the nurse should: Place unwanted or expired medication into a sealable plastic bag or other empty container to prevent liquid medications from leaking out. Mix medicines (do NOT crush tablets or capsules) with an unpalatable substance such as kitty litter or used coffee grounds; Seal the bag and/or container Throw the bag/container in the trash Note: a. Disposal of Narcotics must be handled pursuant to the Controlled Substance Destruction Policy found on Page 11. b. A Dropped narcotic pill must be documented as a “waste”. Do not throw it in the trash. You must save it in a clearly labeled and safe place away from the other medications and immediately contact the Delegating Nurse. The latter will witness it, properly document, and safely destroy it according to the disposal guidelines. 15 | P a g e 4/14 DOCUMENTATION The resident’s legal health record is comprised of the complete documentation of the healthcare services provided to an individual by all healthcare providers. The legal health record includes individually identifiable data, in any medium, collected and directly used in documenting healthcare and health status (includes the open record, the thinned record, and the closed medical record). The purpose of the health record is to provide a view of the resident’s health history and health status and to provide a method of communication among practitioners. This includes observations, measurements, diagnosis, and prognosis. The record identifies services rendered to the resident, why services were needed, resident’s response to the care, and the standards of care used to deliver care. Complete, ongoing and organized records will be maintained for each resident from the time of admission to Eden Homes until termination of any stay at a home. Resident records will be maintained as Confidential Information. A notebook will be created for each resident upon his or her admission and will include the following: Completed Virginia or Maryland required resident assessment form(s) which include the Health Care Practitioner’s assessment form, the assisted living manger’s functional form and the scoring guide; A completed service plan that will address each of the resident’s individual needs; Initial and current medical orders that are signed and dated by the prescribing health care practitioner; Face Sheet Care notes that are dated and signed, Burial From (to the extent provided by the family), and An emergency data sheet. Documentation Management 1. For Maryland Residents: The resident assessment “Health Care Practitioner” form will be given to the prospective resident for completion by their health care practitioner. This form must be completed in its entirety prior to admission to the program. Upon return to the assisted living manager (ALM), the ALM will review the Health Care Practitioner (HCP) form for completeness. At that time, the ALM portion or resident functional assessment form will be completed along with the scoring guide. The resident may be admitted once all necessary forms are complete and approved. For Virginia Residents: The prospective resident must have their health care practitioner complete the Report of Resident Physical Examination and the Assessment of Serious Cognitive Impairment prior to admission. The Administrator and/or Director of Nursing will review the forms for completeness. A qualified assessor will review the documents and 16 | P a g e 4/14 complete the Uniform Assessment Instrument (UAI) before admission (and update them annually as well as whenever there is a significant change in a resident’s condition). Also, in Virginia, a qualified person shall develop an individualized service plan (ISP) in a manner that will maximize the resident’s level of functional ability. An initial plan addressing the immediate needs of the resident will be developed within 72 hours of admission. In all locations, the ALM/Administrator and Director of Nursing will develop a comprehensive service plan for each resident within 30 days of admission. It will contain all of the information required under the assisted living regulations. The ALM or Administrator will update the service plan for changes in services required by the resident whenever necessary or, at a minimum, it will be reviewed every six (6) months if there has been no change. Staff, family, and resident will participate in development and implementation of the resident’s service plan. 2. The ALM/Administrator and the family will sign and date the service plan (ISP) each time it is updated or reviewed. The ALM and Director of Nursing will meet with the family no less frequently than semi-annually to review the service plan. 3. Initial medical orders will be obtained when the resident assessment is completed. The Director of Nursing or her designee will ensure that it is completed, signed and dated by the prescribing HCP. a. Thereafter, the ALM will ensure that a signed medical order is maintained in the resident’s record for any changes in medication orders, treatments, diet and other rehabilitation plans, if appropriate. b. To ensure that current medical orders are received and maintained, the ALM will provide a physician’s visit form for the resident to take to his or her physician each time the resident is seen by the physician. The physician’s visit form will be returned by the resident (or his or her escort) to the facility. It will be reviewed by the ALM or designee for completeness, physician’s signature and date. The ALM will also review the form for any changes in medication, treatment, or diet. If the form has medication changes, the ALM will notify the facility’s Director of Nursing and then make the appropriate changes to the MAR and the emergency date sheet. c. If there are any orders that may affect the services provided to the resident, the ALM will make appropriate changes to the service plan. d. If there are any new medication orders or changes in the dosage of the medication orders, the pharmacy or family providing the medications will be contacted and informed of the change to ensure the new medication or change in dose of the medication is available for the resident. 17 | P a g e 4/14 e. If the physician does not choose to complete the physician’s visit form, the ALM will contact the physician to verify if there are any changes. If there are changes, the ALM will (i) notify the Director of Nursing and (ii) obtain a written copy of the medical order to ensure that the current orders are kept in the resident’s record. If there are no changes, the ALM will make an entry in the care notes stating that the resident was seen by the HCP (including the name of the HCP and the date of the visit) and that no orders were given. The date, time and name of the HCP spoken to will also be documented in the care note. 4. Care Notes will be kept by the ALM or designee. A note will be written for any significant change, occurrence or even such as: a. A deterioration or improvement in a resident’s health status or the resident’s ability to perform activities of daily living. b. An alteration in the behavior or mood resulting in an on-going problematic behavior, c. The elimination of problematic behavior on a sustained basis. d. Any communication made with the HCP or the responsible party/ resident’s agent regarding the resident’s care. e. If the resident’s falls or receives an injury; a brief note may be made that this occurred after the required incident report is completed. f. If the resident is sent to the hospital or the emergency room for any reason, the ALM will document what led up to the emergency transfer. g. The ALM or designee with inform the resident, the resident’s healthcare representative or responsible party and all appropriate health care providers involved in the resident’s care, such as the residents physician, the home health agency, etc. The ALM or designee will document the notifications in the care notes. Each care note entry will be dated, the time noted, written legibly and signed by the person making the entry. 5. The emergency data sheet will be printed from ICareManager and included in the emergency packet for each resident. A copy of the advance directive, DNR order (on the Maryland Emergency Medical Service, Palliative Care/ Do Not Resuscitate (DNR) Order form), guardianship papers or Power of Attorney, available and applicable is to be attached to the emergency data sheet. a. When the resident is transferred to an acute care facility, a brief care note will be written. The care note will state that the emergency data sheet was sent with the resident, the name of the person it was given to, and the date and time given. The Director of Nursing will be notified. b. The ALM will update the emergency data sheet whenever necessary and appropriate. 18 | P a g e 4/14 c. The ALM will make certain that a copy of the Advanced Directive, guardianship papers, Power of attorney and DNR orders are maintained if appropriate in the facility at all times. Record Retention Policy Resident records will be maintained for a period of seven years after the discharge of the resident. The company uses Iron Mountain to manage the storage and destruction of documents. In order to preserve the confidentiality of resident information, resident records are shredded upon the expiration of the holding period. Documentation of destruction is maintained including a list of chart file numbers and resident identifiers are permanently maintained along with the date and certificate of destruction. ELOPEMENT PROCEDURES Eden Homes assesses each resident for elopement on admission, at each care plan review, and when there is a change in status that warrants an updated assessment. In addition, the risk of elopement is minimized through the use of a functional alarm system, staff education, and other techniques. Elopement is the ability of a resident who is not capable of protecting himself or herself from harm to successfully leave the facility unsupervised and unnoticed and who may enter into harm’s way. Wandering refers to a cognitively-impaired resident’s ability to move about inside the facility aimlessly and without an appreciation of personal safety needs and who may enter into a dangerous situation. Elopers are differentiated from wanderers by their purposeful, overt, and often repeated attempts to leave the facility and premises. About 80 percent of elopements involve residents known to be chronic wanderers with prior elopements. Insurance claims statistics show that nearly half of elopement cases and associated accidents occur within the first 48 hours of admission. 19 | P a g e 4/14 Initial Assessment An elopement risk assessment is completed by the nursing staff on all residents on admission, semi-annually and upon a change of condition. If the assessment determines that the resident may be an elopement risk, the ISP will include such information. Prevention Residents at high risk for elopement will be monitored by staff in such a way that they know where the resident is at all times. Residents that wander will be encouraged to participate in activities that are in full view of staff members and be given alternative activities to maintain their interest. The staff will use their best efforts to keep the doors locked and alarmed at all times. In particular, when vendors or families leave, they will recheck the alarms to ensure they are functioning properly. Photographs of each resident will be taken at the time of admission for inclusion in ICareManager and on the resident book. Photographs should be updated as required to reflect changes in a resident’s appearance. Intervention Responding to an unidentified alarm or non-specific concern: It is the responsibility of all staff to respond to an activated door alarm and determine the reason for the alarm. If there any concern that a resident may have exited the facility, they will immediately (a) visually check the area surrounding the door and (b) if no resident is visible outside of the facility, let the shift leader know of the unexplained alarm and assist in conducting a count of the residents. When an unaccompanied resident is visually located in the immediate area outside o Approach in a calm and reassuring manner o Have one individual approach the resident. Discourage large numbers of staff around the resident o Avoid arguing with the resident. DO NOT say “You can’t” or “You have to” o Avoid touching the resident if possible o Using an encouraging voice, invite the resident to return “home” or, at a minimum, join the staff person for a “enjoyable moment sitting on the front porch or an alternative diversionary activity. When the resident is settled in the activity, call the shift leader for assistance if the resident will not re-enter the facility. o The family and physician are to be notified by the administrator or house manager of the incident, and notification documented in the resident’s clinical record. When a resident is determined to be missing: 20 | P a g e 4/14 o Mentally note the time that the resident is/was determined missing o In Virginia, the shift leader will immediately call the adjacent house(s) to determine if the resident is there and, if so, discontinue the search process. The shift leader must determine if the resident went next door without supervision (in which case a full report must be completed and discussed with the administrator) or if, with supervision, who the supervising staff member was and who they informed that they were taking a resident next door. o Next, if the resident isn’t in the adjacent house in Virginia, the shift leader will notify the Administrator or house manager that a resident is missing o Two staff members (the shift leader and one other designated team member) will conduct a thorough search of the immediate area to locate the resident. If any other Eden Homes staff are present in the facility, they should also assist with the search. In Virginia, the shift leader will also enlist the assistance of available staff in the adjacent house(s). The search should be conducted so that all areas of the house, grounds, and neighboring streets are systematically searched when a resident is missing or has eloped o The Administrator or house manager/shift leader assigns each staff member an area to minimize overlapping or overlooking of an area o When conducting a search, it is important to look under beds and furniture, in closets, under desks, and behind doors. When conducting a search in storage rooms, look behind boxes, in boxes, and on shelves. A resident who has eloped may be frightened and may be hiding. Being thorough in the search is of extreme importance o When finished searching a sector, report back to the person who gave the location assignments for the search for further instructions If the resident has not been found after a period of ten minutes, the Administrator or house manager/shift leader calls the police and reports the resident missing. When the police arrive the Administrator or Director of Nursing provides the officer with a picture and other pertinent information such as: • What the resident was wearing • How the resident was ambulating, e.g., with a cane, walker, etc. • The resident’s cognitive status, e.g., confused, alert • Information as to where resident may be going, if known • A resident profile, which includes the resident’s previous address and family’s address, is available in the resident’s chart for this purpose The Administrator/Director of Operations or Director of Nursing notifies the family and attending physician if the resident is not found in the facility or on the grounds When a resident has been found: o The Administrator or house manager/shift leader notifies all staff that the resident has been found o The resident must be examined for injuries by a nurse 21 | P a g e 4/14 o The attending physician is notified by the administrator of the resident’s status o The resident’s responsible person is contacted by the Administrator/Director of Operation or Director of Nursing and informed of his/her status o The care plan is revised and updated o The shift leader completes a Missing Resident form and all staff present a n d involved sign the form. The form is forwarded to the Administrator/Director of Nursing/Director of Operations o The Administrator/Director of Operations will report the incident to the Regional Licensing Office (per procedures specified in 22 VAC 40-72-100 for Virginia only) and other state authorities as required. Documentation Document in the resident record all elopement attempts and events, including objective and factual statements regarding: • Circumstances and precipitating factors • Interventions utilized to return the resident to the unit • The resident’s response to the interventions • Results of reassessment upon the resident’s return and the condition of the resident • Care rendered • Notification of police, physician, and family • Physician orders following notification • Additional prevention strategies implemented • The shift leader must complete an Incident Report and forward the report to the Administrator. Elopement Drills The Training Coordinator will conduct elopement drills on a semi-annual basis. All persons attending the drill will sign-in using the standard sign-in sheet (i.e., name, signature, date of drill, person conducting drill, etc.). When completed, the administrator and Training Coordinator will review and utilize results for further staff education, as needed. The Training Coordinator will document elopement drills with the Elopement Drill Checklist found in Exhibit 5. 22 | P a g e 4/14 EMERGENCY DATA PACKETS FOR RESIDENTS If a resident is being sent out 911, they must be sent with a current emergency packet. ICareManager includes an option for printing the Emergency Packet. Select the main resident screen and then the Emergency Packet icon to the right of the resident’s name. On the next screen, ICare gives you the option to select the documents that you want to print (or, in the event of an emergency where the resident isn’t in the house, fax). The emergency packet must include the following documents: Emergency Data Sheet, List of Current Medication, Insurance Cards, OLST, DNR, Power of Attorney and Advance Directives, as appropriate. Click on each of these items and select the print option. Each house should keep a pre-made emergency packet which contains all documents except the list of current medications. In the event the computer is not available, a copy of the MAR should be put into the emergency packet sent with the resident. 23 | P a g e 4/14 EMERGENCY PREPAREDNESS AND DISASTER PLANNING Eden Homes’ emergency preparedness and disaster training program prepares staff for expected and unexpected disasters. There are several types of emergencies covered: a fire, weather or environmental, or a local medical emergency such as a pandemic. The full version of the Emergency Preparedness Plan can be found in the House Books. All staff must familiarize themselves with these plans and will receive periodic training in general and specific emergencies. The administrative emergency and disaster liaison for all houses is Chido Machanzi. Chido Machanzi can be reached by cell phone at 301-536-2757 or by email at chido@edenhomesgroup.com. Additionally, the House Manager/ALMs are liaisons for their respective houses. They can be reached as follows: Maryland: Stoneham Ipswich Greyswood Bells Mill Arnie Yap Mary Kamaluma Rosaline Wilson Martha Annan 301-767-7167 301-641-4463 301-525-1979 301-785-5195 arnie@edenhomesgroup.com maryk@edenhomesgroup.com rosaline@edenhomesgroup.com martha@edenhomesgroup.com The emergency cell phone numbers for each Maryland house are registered with FRED (Facility Resource Emergency Database). Virginia 8333 Lewinsville 8337 Lewinsville Anna Banda-Freeman Jariatu Koroma 703-350-2064 301-310-1921 anna@edenhomesgroup.com jari@edenhomesgroup.com Information regarding Fairfax County is available from the Fairfax County Office of Emergency Management. Our contact there is Bruce McFarlane, Assistant Coordinator & Community Resiliency Supervisor at 571-350-1016. Each Virginia house is registered with Fairfax Alerts at www.fairfaxcounty.gov/alerts. House Alarm System All houses are equipped with an alarm system that monitors the entire house for fire and smoke. The panel at the front door is the control center for the fire alarm system. This system is maintained by Satellite Industries. It is a monitored alarm so that the monitoring company will call the fire department in the event they receive an indication of alarm from the house. If an alarm goes off in error, you can call the monitoring company who can be reached at 301-840-5420 to cancel the alarm notification. You will 24 | P a g e 4/14 need the password for the system, which is the street name of the house (for example, the password for 6505 Stoneham is “stoneham” and for 8337 Lewinsville is “lewinsville”). This information is also available on the intranet under the Maintenance tab. Checking System for Errors If the alarm system goes off in error, reset it by following the instructions below. If it continues to go off after it was reset contact Jimmy Newton immediately at 301-908-3151. Tell him what the message display on the alarm panel says. He will advise you as to the appropriate action to clear the error. Resetting Alarm System To reset the alarm system if it goes off in error press 1111 pause then press 1111 again. Ejection Pumps (Ipswich and Stoneham only) The ejection pumps, located in the storage room, have their own alarm which can often sound like the fire alarm. If that alarm goes off please DO NOT TOUCH the alarm and DO NOT use the downstairs restrooms until Jimmy advises that it is safe to do so. Call Jimmy immediately at 301-908-3151. 25 | P a g e 4/14 EVACUATION POLICIES Evacuation may need to be immediate following an unexpected event (i.e. sudden fire) or it may follow advance warning (i.e. predicated weather condition). For unexpected emergency evacuation, follow these steps: 1. ALM or Shift Leader calls 911 and engages (in the event of a fire) the fire alarm system. In the event of a non-fire emergency, ALM or shift leader will verbally call to each of the other staff members to alert them of a problem. 2. Keep Calm. ALM or Shift Leader takes residents Emergency Data Sheets with them as they escort residents from the building. 3. All staff escort residents out of facility or, where residents cannot be moved, evacuate “in place”. Residents and staff will meet at the designated meeting place. a. Lewinsville Road houses – Meet in church parking lot on Springhill Road b. Ipswich, Greyswood and Stoneham houses – Meet on the sidewalk (staying clear of the affected house’s driveway and aware of potential emergency vehicle access) on the opposite side of the street from the house. c. Bells Mill – Meet in the area across from the circular driveway (but still on Eden Homes property) 4. ALM or Shift leader will account for each resident making note of those that are in the evacuation safe area and those that evacuated “in-place”. ALM will provide this information immediately to emergency personnel in charge. 5. All staff explain to residents that: a. They must carefully follow staff instructions b. Staff shall continuously monitor and assist them c. They will be taken to a safe location. 6. ALM will contact the designated transportation resources and arrange to move the residents to the nearest Eden Homes facility as an interim measure. The ALM will immediately contact the Director of Nursing to arrange for each of the residents to be evaluated when they reach their interim destination. If any of the residents are in need of immediate medical attention, they will be transported by ambulance (i.e., call 911) to the nearest emergency room to assess the impact of the disaster on their health and mental status. At least one staff member shall accompany them, taking with them the emergency data sheets. 26 | P a g e 4/14 Suburban Hospital located on Old Georgetown Road in Bethesda, Maryland is the designated hospital for all Maryland houses. Inova Fairfax Hospital at 3300 Gallows Road, Falls Church, Virginia is the designated hospital for all Virginia homes. 7. Once the residents are at the emergency department, one staff member will overlook the residents and provide resident emergency data to hospital staff. 8. When the residents and staff are accounted for and safe, the ALM or shift manager shall call the emergency off site contract person--Lori Larson (301)325-9250 or, in her absence, Lisa Max (301) 325-2410. The ALM or Shift Leader shall also call each resident’s family and/or responsible agent to notify them of the event and let them know where their resident is located. For expected emergency evacuation follow these steps: 1. Residents in Maryland will be transported, with staff, to Bethesda Court Hotel, located at 7740 Wisconsin Avenue, Bethesda, Maryland 20814, Telephone number 301-656-2100. An alternative location is the American Inn at 8130 Wisconsin Avenue, Bethesda. Residents will be monitored and cared for by staff members until tor if they are claimed by family and/or responsible party. Residents in Virginia will be transported, with staff, to Crowne Plaza Tysons Corner at 1960 Chain Bridge Road in McLean. The ALM or Shift Leader will account for each staff member as they are both entering the transportation and arriving at the temporary facility. 2. ALM or Shift Leader to call emergency off site contact person, Lori Larson (301)325-9250 or, in her absence, Lisa Max (301) 325-2410. The contract person shall be updated to the status of residents and staff. 3. ALM or Shift Leader make sure to provide the following to the family member and/or responsible agent, in the event a resident is picked up: - A copy of the updated face sheet - Any medication needed by resident - Any treatment materials needed by resident (i.e., pads) - Any personal belongings wanted by resident - Have family and/ or responsible agent sign for my medical, treatment, and/ or personal belongings they removed from premises. 27 | P a g e 4/14 28 | P a g e 4/14 29 | P a g e 4/14 FINAL STATEMENT OF ACCOUNT Within 30 days of a resident leaving Eden Homes, the company will provide the resident or their representative with a final statement of account. At that time, any funds due to the resident shall be paid. The account will be in the format of an accounting statement or, if real property is involved, shall include the following information. NAME OF RESIDENT NAME OF FAMILY/ RESPONSIBLE AGENT REFUNDS DUE EDEN HOMES - BELLS MILL PROGRAM RETURNED THE FOLLOWING: (LIST OF MONEY, PROPERTY, OR VALUABLES RETURNED) STAFF SIGNATURE DATE __/__/____ RESIDENT SIGNATURE DATE __/__/____ RESPONSIBLE AGENT DATE __/__/____ 30 | P a g e 4/14 GRIEVANCE/COMPLAINT PROCEDURE 1. Grievances, which for the purpose of this procedure involve items less serious in nature than complaints, may arise in the day-to-day activities within the house. Residents and their families are encouraged to bring any concerns to the attention of the House Manager or the Director of Nursing. If the family feels that they do not receive acceptable resolution from those initial contacts, the family should contact Jonathan Edenbaum (for Maryland houses), Renee Groban (for Virginia houses) or Lori Larson (for either) to discuss the matter further. Grievances need not be put in writing unless the family desires to do so. Both written and unwritten grievances will receive equal attention. 2. The persons authorized to receive written inquiries and complaints are Lori Larson or Lisa Max, owners of Larmax Homes, LLC who manages the facility. 3. Ms. Larson or Ms. Max will investigate and respond to any complaints within 7 days of receipt of a written complaint. 4. All complaints will be addressed in a timely manner and verbally communicated to the resident and/or the non-resident. All complaints will be followed up with a written confirmation of the investigation findings, resulting actions and further evaluation. 5. All complaints will be verified with the resident, staff and non-residents affected. Staff and involved residents and non-residents will meet and identify and select appropriate alternatives to resolve the problem. The alternative selected will be implemented and after the change in care, there will be an evaluation process to assess if all parties are satisfied with the chosen alternative. Maryland Procedures In Maryland, non-residents will be notified at the time of filing for the license that, if complaints are unresolved, they have the right to lodge a complaint or input with Montgomery County Health & Human Services (240-777-6600) or Licensure and Regulatory Services (240-777-1133). Complaints must be in writing and a copy sent to LarMax Homes at PO Box 59664, Potomac, MD 20859. Copies of any complaints indicating that a complaint has not been resolved to the satisfaction of the person filing the complaint will be forwarded to Montgomery County Health & Human Services, Licensure & Regulatory Services within 7 business days. 31 | P a g e 4/14 Complaints can also be filed with the Maryland Department of Health and Mental Hygiene A copy of the Maryland complaint form follows this section. Virginia Procedures In Virginia, complaints can be filed with the Northern Virginia Long-Term Care Ombudsman Program by contacting them at 703-324-5861. Also, the Virginia Department of Social Services will review complaints filed online. The complaint form is found at http://www.dss.virginia.gov/facility/alf.cgi under Related Links on the righthand side of the page. A copy of the Virginia complaint form follows this section. 32 | P a g e 4/14 MARYLAND Department of Health and Mental Hygiene Office of Health Care Quality Spring Grove Center • Bland Bryant Bldg. • 55 Wade Avenue • Catonsville, MD 21228 • 410-402-8015 Maryland Complaint Report Form Complete this form if you have concerns about the health care or treatment that you or a family member received or did not receive. Answer all questions. Give complete details. Use additional sheet, if necessary. You may use this form as a guide when making a complaint by telephone. We will investigate your concerns based on the information that you provide. You may file an anonymous complaint Complete the following questions. I. Name of patient/resident/client involved in the incident: ___________________________________ Sex: [] Male [] Female Age: _____ II. Health care facility, residence, or community treatment program involved in the incident: Name and Address: ________________________________________________________________________ ________________________________________________________________________ Check the type of facility or program: [] Nursing home [] Adult medical day care [] Assisted living [] Hospital [] Home health agency [] Residential treatment center [] Community mental health program [] Hospice [] Dialysis Center [] HMO [] Ambulatory surgery center [] Residential services agency [] Birthing center [] Medical laboratory [] Community drug treatment program [] Developmental disabilities provider [] Other. Please specify __________________________________ III. Witnesses to the incident: Name Contact information, if known (include telephone number) _______________________________ ____________________________________________________ _______________________________ ____________________________________________________ _______________________________ ____________________________________________________ 33 | P a g e 4/14 IV. Person filing complaint or reporting incident (optional). Note: If you would like a deficiency report that may result from our investigation, please complete this section. Name: ______________________________________________ Relationship: ____________________ Address: ___________________________________________________________________________ Telephone: _____________ May we reveal your identity during the investigation of your complaint? [] Yes [] No V. Briefly describe the incident or your concerns (use additional paper if necessary): Include dates and times, persons involved, and description of what happened. Include attachments, if appropriate. Note: If this is an anonymous report, be complete since we will not be able to contact you to obtain missing information. VI. Have you reported this incident or concern to the person in charge of the facility, residence or program? [] Yes [] No Address written complaints to the appropriate licensing unit (listed below) and mail to: Office of Health Care Quality Spring Grove Hospital Center Bland Bryant Building 55 Wade Avenue Catonsville, Maryland 21228 Or submit your complaint to the appropriate OHCQ licensing unit phone: Nursing homes- (410) 402-8201 Toll-free 877-402-8219 Assisted living homes- (410) 402-8217 Toll-free 877-402-8221 34 | P a g e 4/14 35 | P a g e 4/14 36 | P a g e 4/14 HOT WATER LOG Hot Water temperature shall be measured weekly at point-of-use control valve. These temperatures shall be documented in the hot water log which is found on the Eden Homes intranet. Temperatures should not exceed 120 degrees Fahrenheit or fall below 105 degrees Fahrenheit. INCIDENT REPORTS Policy An incident report will be completed within 24 hours of staff having knowledge that an incident has occurred. An incident may include: The death of a resident from other than natural causes; The disappearance of a resident; An assault on a resident (or staff member) resulting in injury; An injury to a resident that requires treatment by a health care practitioner, or an event such as a fall that could subsequently require treatment; Abuse of a resident; An error or omission in medication or treatment which results in harm to the resident; or treatment which results in harm to the resident, or An emergency situation or natural disaster. An exception to the 24 hour rule is in the case that the whereabouts of a resident are unknown and there is reason to be concerned about his or her safety. In such event, the Administrator, house manager or shift leader (in order based on who is in the facility at the time), shall immediately notify the appropriate law enforcement agency by calling 911. After law enforcement is contacted, the resident’s next of kin, legal representative or designated contact person shall be notified. Procedures Any staff member having knowledge of an incident either by witnessing its occurrence or learning its occurrence from the resident or someone who witnessed the incident must complete an incident report. Incident reports regarding residents are completed through ICareManager. To do this, long into your ICare account and click on the “Residents” tab on the left hand side of the page. 37 | P a g e 4/14 Select the resident for whom you want to enter an incident report and then click on “Resident eChart” by their name. Once in the eChart, select the red box called “Incident Report”. When you have thoroughly filled out the report, print a copy of the report from ICareManager and place the original into the Incident Log in the office. Notify the House Manager and Director of Nursing that a new Incident report is available. Once an incident report is completed, the house manager or his or her designee must review the report, ensuring that the report is completed properly and that follow-up action is taken to discover the cause of the incident and to implement corrective measure to prevent a recurrence of the incident. The house manager or administrator will document the follow-up action taken along with the corrective measure that were implemented. The manager/administrator will also sign and date the report when follow-up is complete. Incidents involving injury to a staff member (which may include, but is not limited to, a resident who is physically abusive to a staff member) should be handled using the Incident Report for Staff which is found on the Eden Homes Intranet under Forms. If a staff member is injured and requires medical treatment due to an incident at work, please refer to the appropriate Workmen’s Compensation forms. Falls The assisted living manager will, within 24 hours, notify the next of kin, legal representative, designated contact person, or if applicable, any responsible social agency of any incident of a resident falling or wandering from the premises, whether or not it results in injury. The resident’s record shall include documentation of the notification, including date, time, caller and person or agency notified. INFECTION CONTROL POLICY AND PROCEDURES To reduce or prevent the transmission of infections, standard precautions will be used in all settings at Eden Homes. The use of standard precautions is not based solely on diagnosis. In the event of an infectious outbreak, Eden Home will delay the admission of new residents until the outbreak is cleared. An “outbreak” is defined as 3 or more residents in a house in a 7 day period with comparable symptoms that are determined by the Director of Nursing to be significant and contagious. In this instance, the nurse or doctor will notify the local health department and follow their recommendations. (For Virginia Department of Health Reporting Requirements, see Exhibit 3.) All staff members, including housekeepers, will receive in-service training at least annually on infection control practices. 38 | P a g e 4/14 Sharp containers will be replaced when they’re ¾ full. Eden Homes has a contract with Biomedical Waste Services to collect the containers. The RN, House Manager or their designee will contact Biomedical Waste Services at 410-437-6590 when a container needs removal. Eden Homes recommends that any individual whose responsibilities include direct hands-on patient care have natural fingernails. Artificial fingernails or other nail enhancements, including but not limited to overlays, wraps, tips or attached decorations are often difficult to clean. Should the Nurse determine that having such enhancements pose a potential hazard to residents, the Nurse can ask the employee to remove the enhancements. Hand Washing Protocol An important component of infection control is proper hand washing. Hand sanitizing is accomplished by either washing with anti-microbial soap and water or using an alcohol based hand rub. Both of these products are readily available around the house. According to the CDC, the following are the guidelines for hand sanitizing by healthcare staff. All staff and volunteers will follow these procedures. When hands are visibly dirty or contaminated, wash hands with either a non-antimicrobial soap and water or an antimicrobial soap and water. If hands are not visibly soiled, use an alcohol-based hand rub for routinely decontaminating hands in all other situations. Decontaminate (using an alcohol-based hand rub unless otherwise indicated) hands before o Having direct contact with residents o Moving from a contaminated-body site to a clean-body site during resident care o Eating (using antimicrobial soap and water) Decontaminate hands (using an alcohol-based hand rub unless otherwise indicated) after o Contact with a resident’s intact skin (e.g., when taking a pulse or blood pressure) o Contact with body fluids or excretions, mucous membranes, non-intact skin, and wound dressing (If hands are visibly soiled, wash with antimicrobial soap and water) o After contact with inanimate objects (including medical equipment) in the immediate vicinity of the patient o After removing gloves o After using the restroom (using antimicrobial soap and water) Techniques for hand-hygiene are: With an alcohol-based hand rub, apply product to palm of one hand and rub hands together, covering all surfaces of hands and fingers, until hands are dry. Follow the manufacturer’s recommendations regarding the volume of product to use. With soap and water, wet hand first with water, apply an amount of product recommended by the manufacturer to hands, and rub hands together vigorously for at least 15 seconds, covering 39 | P a g e 4/14 all surfaces of the hands and fingers. Rinse hands with water and dry thoroughly with a disposable towel. Use towel to turn off the faucet. Avoid using hot water, because repeated exposure to hot water may increase the risk of dermatitis. (For more information, see the How to Handwash? and How to Handrub? posters in Exhibit 1.) Immunizations a. All new employees are required to provide proof that they have either (1) been vaccinated against no less than MMR and Chicken Pox or (2) have blood titers providing evidence of antibodies to these diseases. Furthermore, the Company will encourage staff members to be vaccinated pursuant to the CDC recommendations (as shown in the chart below) for Healthcare Personnel. b. New residents and staff members must show evidence of being free of Tuberculosis whether through PPD or x-ray prior to admission and annually thereafter. c. Influenza vaccines will be given annually to all residents that have a doctor’s order unless contraindicated or declined by a family representative. Consent forms will be sent to families in early fall and will include an option to also request the pneumonia vaccine. d. All staffs will be encouraged to get the influenza vaccine without charge from Eden Homes’ nurses or their own physicians. If they obtain an influenza vaccination other than at work, they will be reimbursed for their out-of-pocket cost. Staffs must sign a consent before getting the vaccine at Eden Homes. e. Staffs, families, and visitors are not to come to work (for staff) or visit (for families and visitors) when they have or suspect they have any communicable disease or infection. f. Residents 65 years and older are encouraged to receive the pneumonia vaccine. Family must consent and a doctor’s order written for this vaccine to be given. 40 | P a g e 4/14 Procedures: -The company will adhere to OSHA standards in the provision of Personal Protective Equipment (PPE) such as gowns, gloves, mask, or eye protection, if potentially harmful splash is anticipated. Cleaning Procedures All equipment (blood pressure machine, stethoscope, pulse ox, scale, etc.) will be cleaned after each use with EPA approved mycobactericidal disinfectant (e.g. bleach concentrate is used at Eden Homes). When disinfecting with a bleach solution, you must wear protective gloves. Concentrated bleach may damage floor finishes, carpets, clothing and other fibers in higher concentrations. Surfaces must be precleaned with a general cleaning agent (for example soap and water) and then disinfected with bleach concentrate. When a resident has been on isolation, the entire space occupied by the resident should receive a thorough disinfecting. When using a disinfectant, keep in mind that some microbes required extended contact with the disinfectant in order to be effective. You should read the label of the container to obtain specific “dwell times” (i.e., lengths of time the solution should be in contact with the surface to be disinfected.) 41 | P a g e 4/14 Bleach used for disinfecting should not be stored longer than 3 months. When mixed with water, the solution is only effective as a disinfectant for 24 hours. Contact Precautions A resident will be put on contact precautions when the doctor or Nurse suspects MRSA, VRE, C-Diff, or Noravirus infection. Contact precautions include: a. Standard Precautions: Before ENTERING the resident’s contact isolation room, Clean hands Put on Gown Put on Gloves Enter the isolation room When EXITING the isolation room: Remove Gloves Remove Gown (from shoulders, roll inside out) Exit the isolation room Wash hands b. Limit transport by having resident stay in his/her room. Private duty assistant may be needed based on cognitive status. c. Dedicated equipment by resident’s door including appropriate means of disposing of any PPE (including gloves, gowns, masks, etc). d. All persons entering a room under Contact Precautions must wear a mask, including visitors, if a concern exists for potential droplet transmission i.e. transmission of droplet coughing, sneezing, and or suctioning. In order to protect our residents and staffs at Eden Homes, at the discretion of the Director of Nursing, additional isolation categories may supplement Standard Precautions based on the ways a specific organism is spread. Monitoring of Infections and Infection Control Program The Director of Nursing shall receive information from each house about both suspected and diagnosed infections as part of a formal monitoring and feedback program. As part of the semi-annual Quality 42 | P a g e 4/14 Assurance meetings, the senior staff shall review such data to determine the effectiveness of the Infection Control Program. Pest Control Eden Homes maintains a service relationship with a pest control company (currently Orkin) for on-call pest control services. If needed, services can be requested by completing the Maintenance Request Form on the intranet and the Director of Maintenance will schedule and oversee the work. 43 | P a g e 4/14 LEVEL OF CARE WAIVERS (MARYLAND ONLY) There may be circumstances under which a resident at Eden Homes in Maryland requires care, for a period expected to exceed 30 days, which is beyond the care that the facility is authorized to provide. This care would include, but not be limited to, the following types of situations: Care exceeding that normally provided for Level 3 residents More than intermittent nursing care Treatment of stage three or stage four skin ulcers; Ventilator services Skilled monitoring, testing, and aggressive adjustment of medications and treatments where there is the presence of, or risk for, a fluctuating acute condition; Monitoring of a chronic medical condition that is not controllable through readily available medications and treatments; or Treatment for a disease or condition which requires more than contact isolation The requirement to seek a waiver does NOT apply when a resident is under the care of a general hospice program licensed by the State (e.g., JESSA Hospice or Montgomery Hospice). Responsibility for applying for a waiver with the Office of Health Care Quality rests with the Director of Nursing. The Application Form follows on the following page. Copies of completed Waiver Applications as well as the State approvals are to be filed in the Resident Book. This section meets the requirements of Maryland COMAR 10.07.14.22 RESIDENT AGREEMENT Each resident is required to sign the Resident Agreement before moving into Eden Homes. The fully resident agreement will be maintained in the Resident’s Book with a copy in the administrative file at the main office. Sample Resident Agreements are found in Exhibit 2. 44 | P a g e 4/14 MEDICAL AND HEALTH EMERGENCIES Staff must be prepared to deal with various emergencies including medical or mental health issues. The first rule in the event of any emergency is to remain calm. The person who identifies the emergency should be the one to take charge. Clear thinking is the key to a successful outcome; panic leads to overreaction or lack of attention to detail. If you find yourself starting to worry about what to do, immediately call for help and turn the situation over to another person, preferably a house manager or shift leader if they are readily available. Medical Emergencies For medical emergencies, the first step is triage so that you can provide the RN on duty with the information she needs to make an appropriate determination. If other staff are close by, ask them to assist you (as soon as they are sure the other residents are safe and secure). Obtain the following information as quickly as possible and then agree on which one of you (if another person is helping you) will call the RN: Vital signs Symptoms Pain level (if relevant) DNR/911 Status (from the OLST) After speaking with the RN, follow her instructions exactly. If she wants you to call the rescue squad, do that immediately. The person who speaks with the RN must be the one to call the rescue squad. Once you have done that, ask the most senior person on the shift to contact the family (if the RN asks you to do so) and to prepare the documentation package for transfer of the resident. At that point, you should return to the resident and stay with them until the rescue squad or RN arrives. If the nurse indicates that CPR is appropriate, the person staying with the resident should do so and continue CPR until the rescue squad arrives. Do not stop giving CPR until told to do so by a medical professional. If for some reason you are not able to immediately reach the RN, check the OLST form to determine the resident’s 911 status. If they are a “Do Not Transfer” continue for three attempts to reach the RN (including sending a text). If you cannot do so, contact the physician directly or physician’s emergency number. In any event, if a resident is listed as “To Transfer” and you suspect a life threatening condition such as a heart attack , call 911 immediately and follow-up with a call to the RN and family. If first aid is prescribed by the RN (or physician in the absence of the RN), the person taking the instructions should provide the first aid (asking for assistance from the senior person on the shift if necessary) and then document the first aid provided and any follow-up first aid needed in the resident communication log. All care staff are certified in First Aid so any person assigned to the shift should be capable of providing assistance. 45 | P a g e 4/14 Mental Health Emergency In general, the residents at Eden Homes will not have diagnoses which might lead to a mental health emergency; however, such an event is not impossible. Prevention of a mental health emergency is the best solution. All staff member should carefully watch residents for escalating signs of mental stress which might result in a mental “break”. If there is any concern, the house manager should discuss their concerns with the RN and appropriate psychiatric intervention obtained. In the event of a significant event which might pose a danger to the other residents and staff, the house manager should instruct the staff to relocate the other residents into a distant, safe area of the house (if that is possible). If during the daytime, two of the staff should remain with the residents in a safe area. As the residents are being relocated, the manager should immediately call 911 for assistance. If safe to do so, the manager should remain with the affected resident until emergency personnel arrive, talking with them in a very calm, reassuring voice but staying an appropriate distance from the resident. In no event should the staff member attempt to touch or restrain the resident in any way. If PRN medicine has be prescribed for an event as the one happening, the manager should obtain and offer the resident the medication. When the resident is safely in the control of the emergency personnel, the house manager should contact the RN and family representative/POA to advise them of the situation. The RN will be responsible for any follow-up activities in conjunction with the psychiatrist and family members. The resident will not be allowed to return to the house until the RN is satisfied, with reasonable certainty, tat the resident no long poses a danger to the other residents or themselves. Otherwise, in accordance with discussions with family members or representatives, Eden Homes will give notice to the resident that it is terminating the Resident Agreement and will assist the family in locating alternative, suitable living arrangements for the resident. 46 | P a g e 4/14 MEDICATION MANAGEMENT (In the state of Virginia, any changes to this section must be approved by the Department of Social Services.) A. Initial health care assessment of the resident will include the following information about the resident’s ability to manage his/her medication(s): a. Capability to self- administer medication(s): b. Capability to self-administer medication(s), but requires a reminder to medication(s) or physical assistance with opening and removing medications from container, or both; or c. Requires that medications be administered by Eden Homes staff or other caregiver who has been oriented, trained and licensed to administer medication. B. Residents who can self- administer medication(s) with or without reminders (as determined with the UAI) will be re-evaluated by the Director of Nursing or a RN every three months or after a change in condition for the ability to safely self- administer medications(s) with or without assistance. a. Qualified medication technicians will setup the medications in a resident’s preferred box or compartment every night to facilitate self-administration of medicines. A current MAR will be kept but the resident is not required to sign as “taken” nor is the staff required to initial and circle as “not given”. b. Residents will be reminded and checked on at scheduled times of medication. When they are going out of the facility with families or friends, medications will be given to them to travel with in case they are due prior to their returns. c. If the Director of Nursing determines that a resident is no longer capable of selfadministering medications (because of non-compliance, errors, lack of following doctors’ instructions, or change in health status etc.), the nurse will update the UAI to reflect the change and have qualified medication technicians administer medications as ordered from that point forward in accordance with the standard Eden Homes procedures. C. Prior to admission, except for those residents who self-administer medication(s) without a reminder or physical assistance, the Director of Nursing will review a new resident’s medication regime. The purpose of this review is to gather comprehensive information about: a. A resident’s current medication profile, including all prescription and nonprescription medication(s) and/or tube feedings; b. The potential that current medication(s) have to act as chemical restraints; c. Potential adverse and/or side effects, and drug interactions from current medication(s); d. Evaluate medication errors that might have occurred since admission. 47 | P a g e 4/14 D. Pharmacy Review: Every six months, a licensed pharmacist shall review the medications of each resident taking nine or more prescription or over-the-counter medications. The purpose of the on-site review is to ensure that: a. Each resident’s medication(s) are properly stored and maintained; b. Each resident will receive the correct medication(s) in the manner prescribed; c. Desired therapeutic effects of medication will be attained and if not the appropriate prescriber will be notified; and d. Adverse effects, undesired side effects, and medication(s) errors will be reported to the appropriate authorized prescriber and/or agency. e. The on-site reviewer shall make all or any recommendations to the appropriate authorized prescriber or assisted living manager or designee. E. Only Licensed Medication Technicians can administer resident’s medication(s) and then only after review and approval by the Director of Nursing. The assisted living manager will arrange for an on-site review or each resident by the Director of Nursing at least every 45 days. The Director of Nursing shall make appropriate recommendations to the authorized prescriber and the assisted living manager or designee. F. Medication Management Training Program – Understanding the Responsibilities All staff must understand the responsibilities associated with giving medicines to others. To ensure that staff understand the requirements of being a CMT, a staff member must meet the following criteria: a. All medication technicians must complete a medication management training course approved by the Department having jurisdiction in the state they will be administering medications. b. Personnel that monitor (under the guidance of the Director of Nursing) staff that provide medications must complete, every two years, an approved clinical update refresher course. c. Upon receipt of the CMT licensure, a staff member must shadow with d. Only Eden Homes staff that has completed approved medication training shall assist a resident with taking medication(s). Moreover, completing an approved class and receiving a license does not mean that a staff member is approved to give medications at Eden Homes. A licensed medication technician can only give medications at Eden Homes AFTER being approved to do so by the Director of Nursing. Your CMT license is not a guarantee that you will be able to give medications with Eden Homes. 48 | P a g e 4/14 e. Eden Homes human resources manager shall document completion of the training in each staff member’s personnel file or other readily available record. f. Medication technicians shall attend clinical updates as required by the Director of Nursing. G. Standard Medication Management Administration Procedures: All Medication Technicians shall follow the following standard procedures in giving medications. There shall be no exceptions or shortcuts. 1. Wash hands prior to preparing medication 2. Identify resident appropriately 3. Compare the Physician’s Medical Order Form (PMOF), the Medication Administration Record (MAR) and the Pharmacy’s medication label for agreement. 4. Checks for allergies of resident if administering a new medication or dietary supplement if the resident is new to the medication assistant 5. Check the expiration date on the label 6. Stop the procedure if the medication has expired 7. Prepare the medication according to directions. 8. Read the label three times. 9. Measure or count the right dose (even when prepackaged ensure that the dosage matches the MAR 10. Confirm that the right medication is being given 11. Administer the medication at the prescribed time on the MAR 12. Administer medication by the route listed on the MAR 13. Prior to administering, double check to ensure it is the right resident (residents pictures are on their charts) 14. Chart the medication (s) by initialing the correct block on the MAR using ink. 15. Chart immediately following medication administration 16. Should the medication be omitted, chart omission accurately and completely 17. When administering a PRN, the med tech must subsequently document the results of using the PRN 49 | P a g e 4/14 H. Preventing the Use of Outdated, Damaged or Contaminated Medicine: Medication Technicians must check the expiration date for any medicine before administering. Additionally, the Med Tech must confirm that the package is not damaged and inspect the medicine for any changes in color or appearance. If there is any question as to the efficacy of the medicine, please contact the RN on duty before dispensing and notify the house manager of the concern. Additionally, the Med Tech is not to directly touch by bare hand any medicine. I. Filling and Refilling Prescriptions: Each house will inventory all medicines (both prescription and over-the-counter) twice each week pursuant to fixed dates established by the house manager. The dates shall be spread apart in a manner that evenly distributes the time between inventories (e.g, Tuesday and Friday). The staff person designated to review the medication supply shall ensure that there is no less than a 7 day supply of each medication on hand at that time. If there is less than a 7 day supply and the physician’s orders are to continue the medicine beyond that 7 day period, the person doing the inventory shall notify that manager that a refill is needed. The manager or her designee shall follow the appropriate procedure for re-ordering the medicine (i.e., if a standing prescription, order a refill directly through the pharmacy; if a new prescription is needed, notify the house manage to obtain a new order from the physician). J. Transcription of Medication Orders: Only the house manager or senior shift leaders who have been properly trained and approved by the Director of Nursing shall transcribe medication orders into ICareManager and the MAR. If the designated staff are unclear of the order (even those that may be hard to read), they must fax the order to the DON and obtain help from her on the phone in the transcription of the order. The Director of Nursing or a RN working for her shall review each month all medication orders for each resident as well as, as needed, any new order once it has been transcribed. K. Monitoring Medication Administration: Eden Homes requires that the MAR (either electronic, paper based or both) shall be (1) fully and accurately completed by each staff member dispensing medications, (2) reviewed each day the house manager or assistant house manager is working at the facility for completeness and accuracy, and (3) reviewed monthly by an RN as well as more frequently if needed. Any concerns that arise during the manager’s review shall be immediately discussed with the DON and, if needed, the Medication Technician shall not be allowed to pass medications again until re-approved by the DON. 50 | P a g e 4/14 L. Supervision of Medication Technicians: The Director of Nursing is responsible for the supervision of all medication technicians. No technician, regardless of their license status, may pass medications at Eden Homes until approved by the DON. This approval process shall include, but not be limited to, achieving a 100% accuracy score on the Observation of Medication Pass form found on the Eden Homes intranet. Additionally, during her 45 day reviews, the DON or her designee shall observe a medication pass selected randomly from among the medication technicians currently passing medications at that house. M. Communications with Physicians: At Eden Homes, the house manager, assistant house manager and RN are responsible for routinely communication issues or observations to the prescribing physician or other prescriber. N. Medication Storage: The House manager or designee shall safely store medication(s) by ensuring that: 1. Medications are stored in the original dispensed container; 2. Medications are stored in a secure location, at proper temperature; 3. The following documentation is maintained for all resident for whom medications are administered, or who receive assistance in taking their medications: 4. Name of the resident 5. Name of the medications 6. Reason for the medication 7. Dose 8. Physician’s or authorized prescriber’s name 9. Date of issuance 10. Expiration Date 11. Refill limits, and 12. Direction for Use MISSING RESIDENT POSSESSION(S) In the event a resident or resident’s family reports that an article of the resident’s belongings is missing, the House Manager shall be immediately notified. The House Manager will complete an Incident Report – Missing Item containing all of the information necessary to conduct an appropriate investigation. The House Manager shall, at a minimum, complete the following actions: Discuss with the (a) shift leaders who have worked during the time between the reported loss and the date of the investigation and (b) the staff assigned to the specific resident the nature of 51 | P a g e 4/14 the missing items to determine the last time that anyone saw the item and where it last resided. At the same time, the House Manager shall obtain suggestions from the staff as to possible locations that the resident might have left the item. The House Manager shall assign a staff member to complete a thorough search of the location in which the item(s) was last seen as well as an ancillary locations where the item(s) might be. The House Manager will notify all staff on the upcoming schedule as to the loss and shall ask them to be vigilant during their shifts to potentially find the missing item. The House Manager shall notify the Administrator, resident and his/her family as to all actions being taken to locate the missing item and keep them informed as the investigation progresses. If any investigation suggests that a staff member may be responsible for the loss, the Administrator shall turn the investigation over to the proper authorities. All documentation regarding the loss shall be maintained in the resident’s file for a period of two years. 52 | P a g e 4/14 NEGLECT, ABUSE, AND EXPLOITATION Abuse, neglect, and exploitation of any types are prohibited at Eden Homes. Abuse is: the physical, sexual, mental, or verbal abuse of a resident, or the use of physical or chemical restraint or involuntary seclusion. Physical Abuse means: injury as a result of cruel treatment Sexual Abuse means: rape, a sexual act or sexual contact with another person by force against the will and without the consent of the other person. Mental Abuse means: conduct resulting in emotional harm Verbal Abuse means: the use of any oral or gestured language that includes disparaging or derogatory terms Physical Restraint means: any method, device, material, or equipment such that a resident cannot move freely. Chemical Restrain means: a drug used for discipline or convenience not ordered by a physician to treat the resident’s medical symptoms. Involuntary Seclusion means: separating a resident from others against the resident’s will. Neglect is: depriving a resident of adequate food, clothing, shelter, supervision, essential medical treatment, 01 essential rehabilitative therapy. Exploitation is: the misappropriation of a resident’s assets or income, including spending the resident’s assets or income (1) against or without the resident or resident’s agent’s consent, or (2) for the use and benefit of a person other than the resident if the resident or agent has not consented to the expenditure. Reporting If a staff member observes abuse, neglect, or exploitation, that staff member is obligated by law to report the incident to the assisted living manager immediately, if possible, and in no case, more than 24 hours. Additionally, the staff member will report the incident to the appropriate agencies. These agencies are: Adult Protective Services Virginia – 1-888-832-3858 Maryland – 240-777-3000 (Montgomery County) 53 | P a g e 4/14 And one of the following: The Police The Office of Health Care Quality or VA Department of Social Services The Ombudsman o Virginia – 703-324-5861 o Maryland – 410-767-1108 If the staff member believes that the manager has taken part in the abuse, neglect, or exploitation, the report will be made directly to Lori Larson. If the staff member is observing abuse, the staff member shall take immediate steps to stop the abuse, if this can be done in a safe manner. Eden Homes shall thoroughly investigate all allegations of abuse, neglect, or exploitation. Eden Homes shall take appropriate action to prevent further incidents of abuse, neglect, and exploitation. After any incident of abuse, neglect, or exploitation, staff will have a training session reiterating the facility’s policies in these areas. The assisted living program shall post signs that set forth the reporting requirements, conspicuously in the employee and public areas of the facility. (Relevant Maryland COMAR sections that are: 10.07.14.02, 10.07.14.22, 10.07.14.27) 54 | P a g e 4/14 PERSONAL FUNDS POLICY Eden Homes of Bethesda, LLC , LarMax Homes, LLC, Eden Homes of Virginia, LLC and their respective employees do not handle residents’ financial affairs. PREADMISSION REQUIREMENTS Before admission, the Assisted Living Manager (ALM)/AALM and the Director of Nursing will determine if a person’s needs can be met at Eden Homes by conducting a personal visit with the potential resident and reviewing, with a family’s permission, medical records. This review, in combination with the documentation required by the state (as outlined in the section entitled Documentation Management), will enable Eden Homes to be fully prepared and knowledgeable about a new resident’s need should they be appropriate for our homes. Before move-in, the ALM or Director of Nursing will gather written information about the resident’s physical condition and medical status. This information shall be based on an examination conducted by a primary physician, certified nurse practitioner or registered nurse, who shall certify that the information being provided reflects the resident’s health status within 30 days of resident’s admission. The assessment information, including that obtained by the staff as well as the state forms, shall include at a minimum: 1. Recent Medical history, including any acute medical condition or hospitalization; 2. Significant medical conditions affecting functioning, including the resident’s ability of selfcare, cognition, physical condition, and behavioral and psychosocial status; 3. Other active and significant chronic or acute medical diagnosis; 4. Known allergies to foods and medications; 5. Medical confirmation that the individual is free from communicable tuberculosis, and other active reportable airborne communicable diseases; 6. Current and other needed medication; 55 | P a g e 4/14 7. Current and other needed treatments and services for medical conditions and related problems; 8. Current nutritional status, including weight, height, risk factors, and deficits; 9. Diet as ordered by physicians; 10. Medical necessary limitations or precautions; and 11. Monitoring or tests that need to be performed or followed up after admission Functional Assessment No more than 30 days prior to admission, the ALM or Director of Nursing, shall collect, on an assessment tool, the following information about each resident: Level of functioning in activities of daily living; Level of support and intervention needed, including any special equipment and supplies required to compensate for the individual’s deficits in activities of daily living; Current physical or psychological symptoms requiring monitoring, support or other interventions; Capacity for making personal and health care related decisions; Presence of disruptive behaviors, or behaviors which present a risk to the health and safety of the residents or others, and Social factors including o Significant problems with family circumstances and personal relationship o Spiritual status and needs, and o Ability to participate in structure and group activities, and the resident’s current involvement in these activities The required assessment tools include the UAI in Virginia and the HCP in Maryland. In Virginia, all potential residents must also ascertain, prior to admission, whether a potential resident is a registered sex offender. This can be accomplished by searching the Virginia State Police Sex Offender Registry at http://sex-offender.vsp.virginia.gov/sor/zipSearch.html. A copy of the search results must be placed into the resident’s file. 56 | P a g e 4/14 RELOCATION AND DISCHARGE Relocation Eden Homes will abide by the following relocation policy. Relocation refers to the movement of a resident to a different assigned bed or living area within the same licensed assisted living program. Discharge refers to the release of the resident from an assisted living program, after which the releasing program will no longer be responsible for the resident’s care. 1. Eden Homes will only relocate a resident in accordance with the terms and conditions of the resident agreement. An Eden Homes staff member shall notify a resident and the resident’s agent at least 14 days before a relocation, except when the program has the consent of the resident or resident’s agent, or in case of emergency. A staff member shall document in the resident’s record how the requirements have been met. 2. When a resident is discharged to another facility, Eden Homes shall provide to the receiving facility, upon authorization by the resident or the residents legal representative, any information related to the resident that is necessary to ensure continuity of care and service. 3. In case of an emergency, a copy of an emergency data sheet shall accompany the resident to an acute care facility. This data sheet shall include at least: a. The resident’s full name, date of birth, Social Security number, if known, and insurance information; b. The name, telephone number, and address of the resident’s agent; c. A copy of advanced directives, guardianship orders, or power of attorney, if any; d. The resident’s current documented diagnosis; e. Medications taken by the resident, if known; and f. The resident’s know allergies, if any. 4. In the event of an emergency, Eden Homes staff shall communicate the following information to the acute care facility at the time of the transfer: a. The resident’s customary or usual function level and needs requirements, and b. Any relevant information concerning the event that precipitated the emergency. 5. Within 30 days of the date of discharge, Eden Homes shall give each resident or resident’s agent a final statement of account, any refunds due, and return any money, property, or valuable held in trust or custody by the program and complete the discharge statement. 57 | P a g e 4/14 6. When the resident returns to the assisted living facility from the emergency room or hospital, the ALM will update the emergency date sheet, ISP and medication orders. The ALM shall notify the delegating nurse/ case manager (Director of Nursing) immediately upon return from the emergency room or hospital. Discharge of a Resident Eden Homes will abide by the terms of the Resident Agreement in the event the discharge of a resident becomes necessary. This means that, in the event of a discharge that is not the result of extenuating circumstances, the resident and their legal representative will be given no less than 30 days written notice of the discharge. Eden Homes will assist the resident in the discharge process and document the process using the Discharge Notification and Statement found in Exhibit 4. When a resident’s condition presents an immediate and serious risk to the health, safety or welfare of the resident or others, an emergency discharge can take place. Staff should be continually discussing with the resident’s family or legal representative behavior or concerns that could potentially lead to the need for care outside of the scope of what Eden Homes can legally and safely provide. A resident may terminate the Resident Agreement at any time by giving 30 days written notice. RESIDENT RECORDS Documentation Overview - Eden Homes considers the resident’s record as a legal document; therefore, they must be prepared and maintained for thorough review. In order to capture resident information in a reliable, complete, accurate, and legible manner, staff must follow the following steps in documenting on any form concerning resident(s): 58 | P a g e Record resident’s information promptly If charting must be delayed, mark the entry as a “late entry” or highlight the date and/or time that the actual entry was made; NEVER “squeeze in” an entry into already recorded information. It may be perceived as “altered” information; 4/14 Recordings should be legible and have only approved abbreviations used; If any error is made (i.e., recoding is made in wrong resident record): a. line through the error, so that it still can be read b. mark next to the error either “error” or “mistake in entry” c. always initial and date after the “error” mark All entries need to be traced back to the individual making the entry. Sign entry with first initial and full last name, and professional designation (i.e., Lucy Brown, LPN would sign as L. Brown LPN). Initials only can be used if you have recorded your name and professional designation in the Staff Roster. Every recording must contain date and time. If an untoward event happens to a resident, record the event in the resident report and state if an Incident Report was completed. DO NOT put “See Incident Report”. The Incident Report is a document between the facility and their insurance carrier. In the event the recording staff and the staff who provided resident care is not the same, then make sure to emphasize that in recording. Fox example, if Nursing assistant Gina Holt provided care and Lucy Brown, LPN records it, it should read “Nursing Assistant, Gina Holt reported that Mr. White…” Each resident will have an individual record to document all resident specific information while ensuring the security and confidentiality of the given information. The log will include: 1. 2. 3. 4. 5. All required preadmission documentation Medical orders and rehabilitation plans, if appropriate The service plan (known as the ISP in Virginia) Care notes Emergency Data Sheet Care Notes. All documentation will be updated in a timely manner regarding resident’s condition and/or preferences. This information will be transmitted in a timely manner to the resident and the resident’s health care representative, when appropriate. Closed Resident Records. Eden Homes program shall maintain a resident’s record for 5 years after the resident is discharged. If Eden Homes ceases operation, we shall make arrangement to retain records for the 5 year period. 59 | P a g e 4/14 REPORTING OF ABUSE, NEGLECT, OR EXPLOITATION Abuse, neglect, and exploitation are prohibited at Eden Homes. Abuse is: the physical, sexual, mental, or verbal abuse of a resident, or the use of physical or chemical restraint or involuntary seclusion. Physical Abuse means: injury as a result of cruel treatment Sexual Abuse means: rape, a sexual act or sexual contact with another person by force against the will and without the consent of the other person. Mental Abuse means: conduct resulting in emotional harm Verbal Abuse means: the use of any oral or gestured language that includes disparaging or derogatory terms Physical Restraint means: any method, device, material, or equipment such that a resident cannot move freely. Chemical Restrain means: a drug used for discipline or convenience not ordered by a physician to treat the resident’s medical symptoms. Involuntary Seclusion means: separating a resident from others against the resident’s will. Neglect is: depriving a resident of adequate food, clothing, shelter, supervision, essential medical treatment, 01 essential rehabilitative therapy. Exploitation is: the misappropriation of a resident’s assets or income, including spending the resident’s assets or income (1) against or without the resident or resident’s agent’s consent, or (2) for the use and benefit of a person other than the resident if the resident or agent has not consented to the expenditure. If you believe that a resident has been subjected to abuse, neglect, or exploitation, you will within 24 hours make report to: In Maryland – Adult Protective Services (phone #240-777-1400) And one of the following: A local law enforcement agency. (phone #311) The Office of Health Care Quality, (phone # 1-877-402-8221) The local area on aging/ombudsman (phone# 240-777-3910) 60 | P a g e 4/ 14 If you do not make a report within three (3) days after learning of alleged abuse, neglect, or exploitation, we may be subject to a fine of up to $1,000. COMAR 10.07.14.27 In Virginia – Adult Protective Services (phone # ) Department of Social Services Licensing (phone # ) RESIDENTS’ RIGHTS While each of the states in which Eden Homes works has different specific language, as included below, with respect to residents rights, all staff members are expected to, without exception, uphold and respect the dignity, individuality and personal rights of each of our residents regardless of how they may be written or whether or not they are included in the lists promulgated by each state. This is a fundamental premise on which our mission is based. Maryland A. At Eden Homes, our residents have the right to: Be treated with consideration, respect, and full recognition of the resident’s human dignity and individuality; Receive treatment, care, and services that are adequate, appropriate, and in compliance with relevant State, local, and federal laws and regulations; Participate in planning the resident’s service plan and medical treatment; Choose a pharmacy provider, subject to the provider’s reasonable policies and procedures with regard to patient safety in administration of medications; Refuse treatment after the possible consequences of refusing treatment are fully explained; Privacy, including the right to have a staff member knock on the resident’s door before entering unless the staff member knows that the resident is asleep; Be free from mental, verbal, sexual, and physical abuse, neglect, involuntary seclusion, and exploitation; Be free from physical and chemical restraints; Manage personal financial affairs to the extent permitted by law; Retain legal counsel; Attend or not attend religious services as the resident chooses, and receive visits from members of the clergy; 61 | P a g e 4/ 14 Possess and use personal clothing and other personal effects for a reasonable extent, and to have reasonable security for those effects in accordance with the assisted living program’s security policy; Determine dress, hairstyle, or other personal effects according to individual preference, unless the personal hygiene of a resident is compromised; Meet or visit privately with any individual the resident chooses, subject to reasonable restrictions on visiting hours and places, which shall be posted by the assisted living manager; Make suggestions or complaints or present grievances on behalf of the resident, or others, to the assisted living manager, government agencies, or other persons without threat or fear of retaliation; Receive a prompt response, through an established complaint or grievance procedure, to any complaints suggestions, or grievances the resident may have; Have access to the procedures for making complaints to; o The Long-Term Care Ombudsman Program of the Department of Aging as set forth in COMAR 32.03.02; o The Adult Protective Services Program if the local department of social services; o The Office of Health Care Quality of the Department; and o The designated protection and advocacy agency, is applicable; Have access to writing instruments, stationary, and postage; Receive a prompt, reasonable response from an assisted living manager or staff to a personal request of the resident; Receive and send correspondence without delay, and without the correspondence being opened, censored, controlled, or restrictions, except on request of the resident, or written request of the resident’s representative; Receive notice before the resident’s roommate is changed and, to the extent possible, have input into the choice of roommate; Have reasonable access to the private use of a common use telephone within the facility; and Retain personal clothing and possessions as space permits with the understanding that the assisted living program may limit the number of personal possessions retained at the facility for the health and safety of other residents. B. Confidential Information Any case discussion, consultation, examination, or treatment of a resident is: o Confidential; o To be done discreetly; and o Not open to an individual who is not involved directly in the care of the resident, unless the resident or resident’s representative permits the individual to be present. Except as necessary for the transfer of a resident from the assisted living program to another facility, or as otherwise required by law, the personal and medical records of a resident are confidential and may not be released without the consent of the resident or resident’s representative, to any individual who is: o Not associated with the assisted living program; or o Associated with the assisted living program, but does not have a demonstrated need for the information. o The assisted living manager shall share resident information with the Department as necessary to administer this chapter. 62 | P a g e 4/ 14 C. Service Prohibited. A resident may not be assigned to do any work for the assisted living program without the resident’s consent and appropriate compensation, unless the resident declines to be compensated. D. Adult Medical Day Care. Adult day care attendance may be encouraged. Adult day care attendance or attendance at any other structured program shall be voluntary, not mandatory. Adult medical day care availability and policies shall be disclosed in the assisted living program’s admission agreement. E. Notice of Resident’s Rights. An assisted living program shall place a copy of the resident’s rights, as set forth in this regulation, in a conspicuous location, plainly visible and easily read by residents, staff, and visitors, and provide a copy to each resident and resident’s representative on admission. Virginia A. Any resident of an assisted living facility has the rights and responsibilities enumerated in this section. The operator or administrator of an assisted living facility shall establish written policies and procedures to ensure that, at the minimum, each person who becomes a resident of the assisted living facility: 2. Is fully informed, prior to or at the time of admission and during the resident's stay, of his rights and of all rules and expectations governing the resident's conduct, responsibilities, and the terms of the admission agreement; evidence of this shall be the resident's written acknowledgment of having been so informed, which shall be filed in his record; 3. Is fully informed, prior to or at the time of admission and during the resident's stay, of services available in the facility and of any related charges; this shall be reflected by the resident's signature on a current resident's agreement retained in the resident's file; 4. Unless a committee or conservator has been appointed, is free to manage his personal finances and funds regardless of source; is entitled to access to personal account statements reflecting financial transactions made on his behalf by the facility; and is given at least a quarterly accounting of financial transactions made on his behalf when a written delegation of responsibility to manage his financial affairs is made to the facility for any period of time in conformance with state law; 63 | P a g e 4/ 14 5. Is afforded confidential treatment of his personal affairs and records and may approve or refuse their release to any individual outside the facility except as otherwise provided in law and except in case of his transfer to another caregiving facility; 6. Is transferred or discharged only when provided with a statement of reasons, or for nonpayment for his stay, and is given reasonable advance notice; upon notice of discharge or upon giving reasonable advance notice of his desire to move, shall be afforded reasonable assistance to ensure an orderly transfer or discharge; such actions shall be documented in his record; 7. In the event a medical condition should arise while he is residing in the facility, is afforded the opportunity to participate in the planning of his program of care and medical treatment at the facility and the right to refuse treatment; 8. Is not required to perform services for the facility except as voluntarily contracted pursuant to a voluntary agreement for services that states the terms of consideration or remuneration and is documented in writing and retained in his record; 9. Is free to select health care services from reasonably available resources; 10. Is free to refuse to participate in human subject experimentation or to be party to research in which his identity may be ascertained; 11. Is free from mental, emotional, physical, sexual, and economic abuse or exploitation; is free from forced isolation, threats or other degrading or demeaning acts against him; and his known needs are not neglected or ignored by personnel of the facility; 12. Is treated with courtesy, respect, and consideration as a person of worth, sensitivity, and dignity; 13. Is encouraged, and informed of appropriate means as necessary, throughout the period of stay to exercise his rights as a resident and as a citizen; to this end, he is free to voice grievances and recommend changes in policies and services, free of coercion, discrimination, threats or reprisal; 64 | P a g e 4/ 14 14. Is permitted to retain and use his personal clothing and possessions as space permits unless to do so would infringe upon rights of other residents; 15. Is encouraged to function at his highest mental, emotional, physical and social potential; 15. Is free of physical or mechanical restraint except in the following situations and with appropriate safeguards: As necessary for the facility to respond to unmanageable behavior in an emergency situation, which threatens the immediate safety of the resident or others; 16. As medically necessary, as authorized in writing by a physician, to provide physical support to a weakened resident; 17. Is free of prescription drugs except where medically necessary, specifically prescribed, and supervised by the attending physician, physician assistant, or nurse practitioner; 18. Is accorded respect for ordinary privacy in every aspect of daily living, including but not limited to the following: a. In the care of his personal needs except as assistance may be needed; b. In any medical examination or health-related consultations the resident may have at the facility; c. In communications, in writing or by telephone; d. During visitations with other persons; e. In the resident's room or portion thereof; residents shall be permitted to have guests or other residents in their rooms unless to do so would infringe upon the rights of other residents; staff may not enter a resident's room without making their presence known except in an emergency or in accordance with safety oversight requirements included in regulations of the Board; f. In visits with his spouse; if both are residents of the facility they are permitted but not required to share a room unless otherwise provided in the residents' agreements; 65 | P a g e 4/ 14 19. Is permitted to meet with and participate in activities of social, religious, and community groups at his discretion unless medically contraindicated as documented by his physician, physician assistant, or nurse practitioner in his medical record; and 20. Is fully informed, as evidenced by the written acknowledgment of the resident or his legal representative, prior to or at the time of admission and during his stay, that he should exercise whatever due diligence he deems necessary with respect to information on any sex offenders registered pursuant to Chapter 9 (§ 9.1-900 et. seq.) of Title 9.1, including how to obtain such information. Upon request, the assisted living facility shall assist the resident, prospective resident, or the legal representative of the resident or prospective resident in accessing this information and provide the resident, prospective resident, or the legal representative of the resident or prospective resident with printed copies of the requested information. B. If the resident is unable to fully understand and exercise the rights and responsibilities contained in this section, the facility shall require that a responsible individual, of the resident's choice when possible, designated in writing in the resident's record, be made aware of each item in this section and the decisions that affect the resident or relate to specific items in this section; a resident shall be assumed capable of understanding and exercising these rights unless a physician determines otherwise and documents the reasons for such determination in the resident's record. C. The rights and responsibilities of residents shall be printed in at least 12-point type and posted conspicuously in a public place in all assisted living facilities. The facility shall also post the name and telephone number of the regional licensing supervisor of the Department, the Adult Protective Services' toll-free telephone number, as well as the tollfree telephone number for the Virginia Long-Term Care Ombudsman Program, any substate ombudsman program serving the area, and the toll-free number of the Virginia Office for Protection and Advocacy. D. The facility shall make its policies and procedures for implementing this section available and accessible to residents, relatives, agencies, and the general public. E. The provisions of this section shall not be construed to restrict or abridge any right that any resident has under law. F. Each facility shall provide appropriate staff training to implement each resident's rights included in this section. 66 | P a g e 4/ 14 G. The Board shall adopt regulations as necessary to carry out the full intent of this section. H. It shall be the responsibility of the Commissioner to ensure that the provisions of this section are observed and implemented by assisted living facilities as a condition to the issuance, renewal, or continuation of the license required by this article. (1984, c. 677, § 63.1-182.1; 1989, c. 271; 1990, c. 458; 1992, c. 356; 1993, cc. 957, 993; 1997, c. 801; 2000, c. 177; 2002, cc. 45, 572, 747; 2004, c. 855; 2006, 396; 2007, cc. 120, 163.) Implementation Plan Eden Homes is committed to the protection of residents’ rights. To that end, the Administrator shall see that all of the following occurs: All new staff will receive specific training in residents rights, including, but not limited to a review of the “Rights and Responsibilities of Residents of Assisted Living Facilities” upon their hiring. The administrator shall discuss with new families how residents rights are respected at Eden Homes, including freedom of choice and encouragement of each resident to remain a participant as long possible in decision making. Annually, the Administrator will review with staff residents’ rights as part of a staff meeting, holding a discussion and answer period to enable staff to discuss particular opportunities to meet our responsibilities to our residents. Should there be any violation, either actual or perceived, the Administrator with meet with the staff member(s) involved to review our policies with respect to Residents rights and counsel them on appropriate implementation. Any violations of residents’ rights will be reported as required by Fairfax County and Virginia regulations. Annually, the House Manager and/or Administrator shall review with each resident their rights. 67 | P a g e 4/ 14 RISK MANAGEMENT AND COMMUNICATION Whenever there is an incident involving a guest, visitor or employee that has or may result in injury or in misappropriation the following protocol of who to contact should be followed. The House Manager and Director of Operations (HM/DO) must be aware of all incidents. The Shift Leader (if the House Manager is not working the shift in which an incident occurs) is responsible for reporting incidents in accordance with the enclosed table for “Notification of Corporate Staff.” When an incident involves a resident, follow the appropriate policies and notification protocol listed in under Incident Reporting. Guest Affected/Injured The HM/DO must be aware of incidents that occur at their facilities where a guest is affected/injured. W hen a guest is seriously injured, the Nurse on duty must be called immediately. The Shift Leader will have the responsibility of informing the other corporate staff of the injury prior to the end of their current shift. If the DO needs to initiate an investigation, please contact Lori Larson. This notification can be done via email. Employee Injured The Shift Leader will report to the DO any employee injury that results in the employee receiving treatment at an outside clinic. We must have an investigation into the causes of the injury completed. All work related injuries and the paperwork that goes with such injuries are to be reported via email to enclosed listed corporate staff. In addition, the HM/DO must be informed by the shift leader of the employee injury prior to the end of the shift that the employee is working. Visitor Injured When a visitor injures themselves, the shift leader on duty must report all visitor incidents (whether an injury results or not) to the House Manager and Director of Operations. This report can be via phone or e-mail. If the incident is something which causes harm (i.e. ANY treatment is rendered either at our facility or at any health care provider) the Nurse on duty must also be contacted immediately. The House Manager will be responsible for informing the appropriate corporate individuals. Regulatory, Public Safety or Legal Contact If the facility receives a visit from an outside entity, such as a surveyor, a police officer, fire marshal, attorney, the Director of Operations must be contacted immediately. In this case, you should ask that the individual go to a private room while you are calling the Director of Operations. The Director of Operations will ensure that the appropriate corporate individuals are contacted. 68 | P a g e 4/ 14 Building & Equipment Failure If the facility experiences a failure in its equipment (such as a power failure or back up of its water) or has a fire alarm, the Director of Maintenance must be contacted. If the issue is something that does not pose an immediate concern (such as a fire alarm with no fire), he can be notified the following day using an Online Maintenance Request. However, if it is something which poses a serious concern, such as any type of fire, outage, etc. the Director of Maintenance must be notified immediately by phone call. Possible Litigation Any incident, letter, statement regarding possible litigation must be reported by e-mail (including a scanned copy of any letter) to Lori Larson immediately. For clarification sake, this notification must occur 24/7. Notification Protocol TYPE OF GuestINCIDENT/ISSUE with an incident that is harmed and/or incident is reportable to the state Employee injury where employee is treated at an outside health provider WHO TO REPORT TO Director of Nursing Director of Operations Employee Requiring ER visit House Manager Director of Nursing Director of Operations Director of Operations Director of Operations Visitor injury with or without harm Director of Operations Attorney Contact Surveyor, police officer, fire marshal, attorney or other outside entity Lori Larson Director of Operations WHEN TO REPORT In all cases, prior to notification to the state; prior to end of the shift on which the incident occurs Prior to the employee receiving treatment unless the person has an emergent medical condition – at which time notification will be as soon as the person is stabilized As soon as the employee has left the premises. Reporting by shift leader. As soon as the incident occurs; prior to the end of the shift, if no injury Immediately Immediately 69 | P a g e 4/ 14 Equipment failure/ power failure/ etc Director of Maintenance Director of Operations If equipment failure affects the running of the facility (for example, a generator, SERVICE PLANS Eden Homes shall develop a service plan (ISP) for each resident upon admission to our facility. In Virginia, this plan will be completed by the Administrator or his/her designee in two stages: within 72 hours of admission an ISP will be developed to meet the immediate needs of the resident. A comprehensive plan shall be completed within 30 days after admission. The person completing the ISP in Virginia must first complete a training program approved by the Virginia Department of Social Services. In Maryland, the plan will be completed within 30 days of admission. The written service plan that will be recorded in the resident’s record will at a minimum address: 1. Service to be provided to the resident, which are based on the resident’s health assessments collected prior to admission; 2. When and how often the services are to be provided; 3. How and by whom the services are to be provided to the resident; 4. The expected outcome and date of expected outcome. The service plan/ISP is to be revised at least every 6 months, and updated if needed, unless a resident’s condition or preferences significantly change, in which case the Assisted Living Manager/Administrator or Director of Nursing shall review and update the service plan sooner to respond to these changes. The purpose of the service plan is to comprehensively address the resident’s needs in a manner that respects and enhances the dignity, privacy and independence of the resident. Eden Homes shall ensure that each resident will have a service plan that enhances the principles of dignity, privacy, resident choice, resident capabilities, individuality and independence without compromising the health or reasonable safety of other residents. 70 | P a g e 4/ 14 SERVICES Meals 1. Eden Homes shall ensure that: a. A resident is provided three meals in the breakfast and dining area and additional snacks during each 24-hour period, 7 days a week; b. Meals and snacks are well balanced, varied, palatable, properly prepared, and of sufficient quality and quantity to meet the daily nutritional needs of each resident with specific attention given to the preferences and needs of each resident including but not limited to religious dietary practices; c. All food is prepared in accordance with all state and local sanitation and safe food handling requirements; d. As meals are often a source of great enjoyment and stimulation, residents shall have as much time as they require or desire to finish their meals; e. Food preparation areas are maintained in accordance will all state and local sanitation and safe food handling requirements; f. Menus are written at least 1 week in advance with portion sizes tailored to each resident and that menus are maintained on file, as served, for 2 months (2 years in Virginia); g. Residents have access to snacks or food supplements during the evening hours; h. Staff shall assist residents, as appropriate, who need help with eating, i. Staff shall continually monitor each resident’s food intake for changes in not only the amount they consume but also for their ability to swallow, manage their utensils or 71 | P a g e 4/14 any other signs that suggest a change in physical or cognitive functioning. The staff noticing such change shall immediately discuss their observations with the shift leader, who shall include such information in their daily report; j. Based on each resident’s service plan (ISP), staff shall monitor compliance with any nutritional needs outlined in the plan; k. For the Maryland licensure approval and renewal process, Eden Homes shall submit a letter stating that they will serve nutritionally balanced, healthy meals. 2. Eden Homes program staff shall prepare or arrange for the provision of special diets as ordered by the resident’s personal physician or as needed by the resident’s condition. If the diet is beyond the capability of the program, the resident or the resident’s physician shall make other arrangement for the resident’s care, or the program shall discharge the resident. 3. Menus shall be dated and posted weekly. Any menu substitutions or additions shall be recorded on the posted menu. 4. Residents experiencing a temporary illness or incapacity may have their meals served in their room (using a sturdy table). Documentation in the resident’s file will reflect these circumstances. Personal Care Services A. Eden Homes shall provide or ensure the provision of all necessary personal care services, including, but not limited to, the range of assistance needed by a resident to complete the following activities of daily living: 1. Eating or being fed; 2. Personal hygiene, grooming, bathing, and oral hygiene including brushing teeth, shaving, and combing hair; 3. Mobility, transfer, ambulation, and access to the outdoors, when appropriate; 4. Toileting; and 5. Dressing in clean, weather- appropriate clothing. Staff shall encourage residents, to the maximum extent possible, to participate in decisions regarding the care and services provided to him or her. Encouraging participation and engagement 72 | P a g e 4/14 in daily decisions is an important component of maintaining a portion of independence in the elderly. B. Eden Homes shall ensure that each resident is monitored on a daily basis to ensure that the resident’s service plan is being properly implemented and to ensure that all adaptive equipment, ambulation devices, and other necessary independent livings aids are in proper working order. C. Eden Homes shall ensure that laundry and housekeeping services are provided and that all areas of the facility are maintained in a clean and orderly condition. D. Eden Homes is responsible for facilitating access to appropriate health care and social services for the resident, including but not limited to: 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Social work services Rehabilitative services, including occupational, physical, speech, and audiology therapy; Home health services; Hospice services; Skilled nursing services; Physician services Oral health care; Dietary consultation and services; Counseling; Psychiatric service; and Other specialty health and social work services such as services for residents with cognitive impairments. E. Eden Homes shall provide or arrange appropriate opportunities for socialization, social interaction, and leisure activities which promote the physical and mental well-being of each resident, including facilitating access to spiritual and religious activities consistent with the preference and background of the resident. To ensure resident participation in social and recreational activities, the assisted living manager shall: (1) Provide or arrange for transportation to these activities in accordance with the resident’s service plan, and (2) Assist a resident with communication, interpersonal, and social skills, including managing difficult behaviors in accordance with the resident’s service plan. 73 | P a g e 4/14 SMOKING AND WEAPONS Smoking is not permitted at any facility owned by Eden Homes. No weapons of any kind are permitted at any facility owned by Eden Homes. STAFFING PLAN Regular Staffing Eden Homes provides staff to meet the 24-hour schedule and unscheduled needs of the residents. At all times, when a resident is in the facility, a staff member will be present. Eden Homes manager shall ensure that each resident is monitored daily to ensure that the resident’s service plan is being properly implemented and to ensure that all adaptive equipment, ambulation devices, and other necessary independent living aids are in proper working order. Staff will have continuous training to enhance and promote quality health care to all residents. Orientation and training shall be provided to all staff to perform all resident-specific procedures (i.e., bathing, wound care) behind closed doors. Staff shall address and communicate to residents in a respectful and friendly manor. There will be two working shifts in a 24-hour period. When the facility is filled with 8 residents there will be 3 staff members during the morning and evening hours and, in Maryland, 1 staff member during the overnight shift and, in Virginia, 2 staff members. In addition, Maryland will have one additional night time staff member designated as the “floater” who shall be available in any house as needed. Transition Phase During the transition phase of populating the facility, the number of residents will vary from 1 to 8. During this span of time, our staffing plan will be one staff member for each shift until there are over 3 residents. Once there are 4 residents, there will be 2 staff members for the daytime shift and 1 overnight to oversee the residents. Once there are over 6 residents, there will be 3 staff members for the daytime shift and 1 overnight to oversee the residents. 74 | P a g e 4/14 Relief Staff In the event that regular staff needs additional assistance, and/or is unable to fulfill required tasks; relief staff will be available as needed. Eden Homes maintains a current list of PRN’s available to fill shifts as needed. Participants on this list are called regularly to ensure that they are available for work and desire to remain on call. Also, staff members working part time at our other houses often are available for relief shifts. Shared Administrator The administrator will be shared by 8333 and 8337 with an office in 8337. Generally, the hours of the administrator shall be 9:00 AM to 5:00 PM Monday through Friday; however, the administrator shall work weekends as needed based on resident and family events and other times when his or her presence is appropriate. The Administrator shall spend appropriate time in each house in order to carry out the responsibilities of the Administrator but in no event shall the total weekly hours be less than 10 per house. The administrator shall be responsible for all staff supervision in both properties as well as relationships with families and other professionals. Each house shall have a designated house manager who reports directly to the Administrator. QUALITY ASSURANCE PLAN Semi-annually, the Owner, Director of Nursing, Assisted Living Manager, Activities Director and Marketing staff meet to discuss and develop a Quality Assurance Plan for each house. This meeting is intended to serve as the basis for continually improving the quality of services provided by Eden Homes. The meeting is an opportunity for each team member to analyze the past six month and engage in constructive criticism of the facilities activities during that time. The review shall include, but not be limited to, a discussion of the following topics: Detailed review of each resident, including any change in their status and adjustments to their service plans Outcome of the pharmacy reviews, including the written recommendations of the consultant pharmacist Review of selected general policies and procedures of the company that could be adjusted for better execution Review of the staff for the facility including performance evaluations, training status, career goals, scheduling, etc. 75 | P a g e 4/14 Review of the structural and maintenance needs of the house; and General comments from the ALM as to their needs and objectives for their house over the next six months The quality assurance meetings will take part in two phases (one a general discussion of the corporate policies and next a detailed discussion regarding a particular house and its residents). The following documents will be reviewed during these meetings: Written Pharmacy Review Any state or county inspection reports dated during the preceding 6 months Results of any “mini” inspections conducted during the last six months The prior Quality Assurance Meeting Report The Director of Nursing will be responsible for scheduling and documenting the meetings. Reports will be filed in the House Book for each house and kept for a period of three years. USE OF MONITORING DEVICES Maryland Only: Some residents may start to wander at night (or while resting in their room) or to continually get up from their beds. While the first line of protection is the installation of a bed alarm, it may become necessary to increase the level of monitoring. With the family’s permission, you can use a baby monitor to easily listen in on the resident’s activities. Prior to using a monitoring device, ask the family representative who has Power of Attorney or, if capable, the resident to sign the following permission form. Virginia Only: Some residents may start to wander at night (or while resting in their room) or to continually get up from their beds. In such cases, the installation of a bed or chair alarm is warranted. No additional audio or video monitoring devices, regardless of family preference, may be used in Virginia homes. VISITING POLICY There are no scheduled visiting hours at Eden Homes. Families are not only invited but encouraged to visit at any time. To ensure that a resident is up and receiving visitors, families are asked to contact the manager to determine, should they want to visit in the evening, what the resident’s preferred sleeping hours are and when the best times to visit might be. Family members are welcome to join a resident for a meal. Up to two meals per month for visitors are included in the monthly fee. Families are asked, to the extent possible, to provide advance notice of their intention to stay for a meal so that adequate food can be prepared. 76 | P a g e 4/14 EXHIBITS EXHIBIT 1: HOW TO HAND WASH/HANDRUB? 78 | P a g e EXHIBIT 2: RESIDENT AGREEMENTS 79 | P a g e Virginia RESIDENT AGREEMENT LarMax strongly encourages You to have Your attorney or other representative review this Agreement before You sign. PARTIES This Agreement (the “Agreement”) is between LarMax Homes, LLC (“LarMax”) and ____________ (“You”). You are leasing a private room and being provided meals and other assisted living services in our Home at 8333 Lewinsville Road, McLean, VA 22102 (the “House”.) This Agreement is effective as of __________. This property is currently managed by Eden Homes of Virginia, LLC (“Eden Homes”). LEVEL OF CARE 1. Based on information provided by Your doctor, You, Your family and our assessment, an initial level of care is established as part of your Service Plan. If LarMax determines at any time that (i) You need a higher level of care than LarMax is licensed to provide; (ii) Your care needs are such that LarMax cannot safely handle them based on its standard staffing patterns (including, for example, more than one staff member is required to turn, bathe or move You or the time required to assist with Your activities of daily living substantially extends beyond those provided other residents), or (iii) if LarMax determines that Your emotional and physical limitations are not conducive to residing in this Home, LarMax may discharge You and terminate this Agreement as provided herein. 2. By signing this Agreement, You acknowledge that You received and carefully reviewed the Uniform Disclosure Statement for this Home. It provides detailed information on what our standard services are as well as the staffing levels LarMax expects to maintain. It also identifies services that are outside of the scope of this Lease. If a conflict arises between the provisions of this Agreement and the Uniform Disclosure Statement, this Agreement shall prevail. FEES 3. The monthly fee for Your room, board and care is $ _____. You agree to pay this fee in advance by the first (1st) day of each month. In addition, a monthly invoice will be sent to You detailing any additional fees or expenses due such as transportation, beautician services, personal hygiene items, nutritional supplements and other items purchased on Your request or behalf. You agree to promptly reimburse LarMax for such costs within 14 days of receipt of the billing. 4. Upon signing this Agreement, You agree to pay LarMax a deposit equal to the first full month’s rent. This deposit will be returned to You, less any outstanding fees and expenses You owe under this Agreement, within forty five (45) days after the removal of Your belonging from the Home. Your security deposit may be used to repair or replace any damage to Your room or common areas that You cause. You also agree to pay a non-refundable Admission Fee in the amount of $5,000. No room will be held for occupancy prior to receipt of this Admission Fee and, once paid, this fee shall be deemed earned by LarMax and is not refundable for any reason. 5. Fees shall be adjusted periodically; however, except as provided below, there shall be no increase in the monthly fee during the first year of this Agreement. LarMax will give You forty five (45) days advance notice in writing before any increase or change in the monthly fee. (This notice does not apply to costs of incidental expenses, which will change as market prices change.) 80 | P a g e 6. If You are absent from the house for any reason (i.e., vacation, hospitalization, temporary stay at a nursing facility, etc.), You agree to continue to pay the full monthly fee and other charges until this Agreement is terminated as provided herein. 7. Any fees or charges incurred and billed on the monthly statement are due and payable by the 5th day of the month. If You do not pay any charges by the 10th day of each month, You agree to also pay an administrative fee of $150 plus interest at the rate of one and one half percent (1.5%) per month, calculated from the first day of the month, until satisfied. If You default on paying any of the fees or charges billed on the monthly statement, LarMax may at its discretion refer the unpaid invoices for collection and terminate this Agreement as provided herein. If sent for collection or eviction for non-payment of fees, You also agree to pay all court costs, services of process, litigation expenses and reasonable attorney fees incurred for the collection of the debt and termination of this Agreement. 8. By signing this Agreement, You represent that You have assets and income which are sufficient under foreseeable circumstances for payment of Your obligations under this Agreement. SERVICES 9. Your monthly lease covers the following services: a. A private room which includes a bed, bedside table and lamp, reclining chair, dresser, bath towels and bed linens. You may use Your own bedroom furniture and linens if You prefer; b. Three meals a day based on published menus and additional snacks; c. Personal care services which include assistance with eating, personal hygiene, transferring, toileting and dressing; d. Laundry (except dry cleaning) and housekeeping services; e. Cable TV and telephone in common areas (Each bedroom is wired for cable TV and private telephone service which You can obtain at Your expense.) Wi-Fi is available at no cost to You throughout the house. f. Assistance with access to health care, social services, and social activities; g. Reminders and/or physical assistance with medications as prescribed by Your physician; h. Two escorted trips per month within seven miles of the Home; and i. In-house activities and occasional programs outside of the Home. 10. Your monthly fee does NOT cover the following services: a. Medications b. Doctors fees c. Medical supplies and equipment d. Personal supplies (i.e., incontinent care products, toothpaste, deodorant, etc.) e. Barber, beautician and manicure fees f. Private telephone and long distance services; and g. Personal Cable TV services 11. You will be in bedroom #___ in the Home. 12. Your room includes a personal lock box for Your use in securing valuables and cash. You understand that LarMax strongly discourages keeping cash or any other valuables (including items of sentimental value) in the Home. You agree that LarMax is not responsible for Your valuables should they be misplaced, lost or stolen. LarMax is not an insurer of Your property and is not liable for property damage, loss, or theft. This includes, but is not limited to, damage to, loss or theft of Your personal property or the vehicles or personal property of Your agents, guests or invitees. Should You elect, against our advice, to keep valuables in the house, You agree to insure them against loss, at Your expense, at their replacement value. 13. LarMax will provide the following security provisions: 81 | P a g e a. b. c. Bedroom and bathroom door locks operable by staff Lock Box for valuables Alarms for every exit door. 14. Staff is available 24 hours a day to request personal emergency medical and protective services (i.e., police, fire and rescue, etc.). Costs related to these services are Your sole responsibility. GENERAL POLICIES 15. To ensure Your safety and wellbeing, the staff has the right to enter Your room and bath; however, the staff will make every effort to respect Your privacy and will always knock before entering. 16. You are responsible for moving in and out of Your room including packing and unpacking Your personal belongings, hanging artwork on Your walls and removing Your personal possessions. Except for normal wear and tear, You agree to return Your room to the same condition that it was at the time You moved in. 17. Any redecoration of Your living space, except for redecoration scheduled and performed by us, must be approved in advance. Any such redecoration is Your responsibility and will be at Your expense. Redecoration includes painting, wallpapering, and applying other cosmetic materials. Any other remodeling is strictly prohibited. If LarMax consent to redecorating, You agree to pay for work to return the room to its original state when this Agreement is terminated. 18. LarMax provides awake staff to care for up to eight residents in the Home on a 24-hour, 7 days per week basis. You understand that LarMax does not provide You with one-on-one, skilled nursing or medical care. LarMax will provide the personal services described in the Uniform Disclosure Statement and Your Service Plan. You will notify staff immediately if You are aware of any unsafe or hazardous conditions or if You would like to discuss changes in the Service Plan. 19. You may have and use a television, computer, stereo, radio and telephone in Your room. All other electrical devices (i.e., space heaters, coffee maker, etc.) are strictly prohibited. Heating pads require a physician’s order and, when not in use, will be stored in a secure area. 20. You agree that the House and surrounding property are non-Smoking areas. ADMISSION AND DISCHARGE POLICIES 21. By signing this Agreement, You are giving your consent to LarMax (at its expense) to complete a background check on You with the National Sex Offender Registry. 22. In the event of a temporary emergency that could make it unsafe or unhealthy to provide services at the Home, LarMax will seek to make arrangements to temporarily relocate You to another licensed facility. 23. You understand and agree that Your age, application forms, health history and medical report, personal interviews and emergency information records are a part of this Agreement. Any significant omission or misrepresentation made by You or Your representatives or agents shall render this Agreement voidable at the sole option of LarMax. You agree to provide updated copies of any of the above forms from time to time as requested. 24. You may be discharged for any one of the following reasons: a. 82 | P a g e Non-payment of the monthly fees; b. c. d. e. Behavior that poses risk of injury to Yourself or others; A change in Your health care or psychological needs above a level of care LarMax is licensed to provide; Your care needs are beyond those that can be safely provided by our standard staffing schedule and staff training; or Your emotional state or physical limitations are not consistent with the environment of the Home. 25. In the event LarMax decides to discharge You for reasons other than health or safety, You will be given 30 days advance notice prior to the date of discharge. In the event You are discharged because of a health or psychological emergency, LarMax may not be able to give You 30 days notice. 26. To terminate this Agreement for any reason other than a health or psychological emergency, You must give written notice at least 30 days prior to the date of termination (the "Notice Period"). (If You pass away while this Agreement is in effect, the written notice is deemed to be given as of the date of death.) If You and Your personal property vacate the property prior to the end of the Notice Period, Your rent will be prorated up to the date, if any, Your room is occupied by a new resident. If You leave because of a health emergency (a medical event which permanently prevents Your return), 30 days advance notice is not required; however, the termination will not be effective and You agree to continue to pay rent until (i) You give written notice that You will be unable to return, and (ii) You remove Your personal belongings from the Home, or (iii) the room is available for occupancy, normal wear and tear excepted, by a new resident. If, for any reason, You do not take all of Your personal property with You within 10 days of Your Notice, LarMax may arrange to have Your belongings packed and stored for 20 days. If You or Your representatives do not retrieve Your belongings within 20 days of placing them in storage, You agree that LarMax can dispose of Your property in the most expedient manner. You agree to pay any costs associated with the disposal of any belongings (including, but not limited to, hospital beds, furniture, clothing, etc.) You leave at the Home after the end of the Notice period. 27. This Agreement begins on the date indicated above and continues in force until terminated upon 30 days written notice by one of the parties. ADDITIONAL PROVISIONS 28. If needed, You or Your representatives are responsible for scheduling, overseeing and paying for Your extra care, including, but not limited to, medical, physical therapy, counseling, and private duty aides if needed as well as contracting for services including equipment and supplies such as a hospital bed or wheelchair. Any private duty aides are Your employees but must agree to and abide by LarMax’s policies for private duty aides. 29. You or Your representatives are responsible for monitoring Your health status and for taking appropriate action. In no event is LarMax responsible for Your medical care other than conducting daily activities as provided in Your Service Plan, assisting in arranging transportation to and from appointments and providing information LarMax has to Your medical care givers. 30. You or Your representatives are responsible for managing Your finances, including ensuring timely payment and the fees and other charges due under this Agreement. In no event will LarMax handle Your finances. RESIDENTS RIGHTS AND RESPONSIBILITIES 31. A copy of the residents’ rights is attached and incorporated by reference into the Agreement. LarMax and Eden Homes will seek to honor and respect Your rights. 83 | P a g e INHERENT RISK OF THE AGING PROCESS 32. There are inherent risks in the aging process that are outside of our control. LarMax will use its best efforts to prevent these risks; however, if You think that You need more care or different care than LarMax provides, we strongly encourage You to consider moving to a different setting. Several of these risks are outlined below and, by signing this Agreement, You acknowledge that You understand these risks and that LarMax is not, except for willful and intentional misconduct, liable for the risks outlined below as well as others normally associated with aging. a. Falls – It is common for the elderly to trip or have trouble moving from one place to another. Falls can occur anywhere and may require medical attention or even hospitalization. You understand and agree that falls are common with the aging process. If concerned about falls, You should discuss with Your physician or physical therapist methods You can take to prevent serious injuries (such as careful selection of special shoes) or consider a living arrangement where You have continual one-on-one care. b. Skin Breakdown – Another part of the aging process is skin breakdown which causes tearing and bruising. In some people this can be more common than others. If at any time You notice areas that raise concern, please point them out to a staff member. c. Loss of Personal Items – Sometimes property can be misplaced or damaged. LarMax cannot guarantee the safety of Your belongings and strongly requests that You not bring valuables with You. RELEASE AND INDEMNIFICATION 33. You (i) waive all claims, causes of action, and other legal actions against LarMax, Eden Homes and all of their members, officers, employees, and agents, and (ii) shall indemnify them against all costs incurred by them (including legal fees) associated with any claim asserted against them by You or Your successors or assigns, provided, however, that LarMax and Eden Homes shall be liable, if at all, only for damages finally determined to be directly attributable to their willful and intentional misconduct. Moreover, LarMax and Eden Homes shall be liable only for the actions of their members, officers and employees, and not for the actions of any resident, his or her guests or other persons. LarMax and Eden Homes shall in no event be liable for any amount which exceeds the limits of the policy as shown in the Eden Homes Certificate of Insurance and shall be liable only for actual damages, not punitive damages or pain and suffering. You hereby expressly release, waive and relinquish any claims whatsoever against LarMax, Eden Homes and their agents and employees in excess of the policy limit. This Resident Agreement is agreed and accepted between the parties, as acknowledged by their signatures below. 84 | P a g e Any changes to the terms and conditions of this lease must be made in writing and accepted in writing by both parties. FOR THE RESIDENT: Resident’s Name: _____________________________________ Signature: _______________________________ Date: _______________ Name of Resident’s Agent: ________________________________ Relationship to Resident: __________________________________ Authority to Sign: ________________________________________ Larmax Homes, LLC Larmax Homes, LLC. By: ________________________________________ Its: ___________________________________ 85 | P a g e Date: _________________ Addendum to Resident Agreement between You and LarMax Homes, LLC By signing this Addendum to the Resident Agreement, You acknowledge that You have read, understand and agree with all of the terms and conditions of the Agreement. You acknowledge that You can, if You so choose, have this Agreement reviewed by the counsel of Your choice. There are no verbal Agreements between You and LarMax Homes, LLC that are not reflected in the Agreement. For the purposes of this and the Resident Agreement, “You” means not only You as the resident but also Your representatives and any person signing the Resident Agreement on Your behalf. You understand that this Agreement calls for a 30 day Notice Period should You leave the Home for any reason other than a Health Emergency. A Health Emergency, for the purposes of this Agreement, is an event for which You need immediate and continuous (defined as a period reasonably expected to extend more than 30 days) skilled nursing or in-patient psychiatric care or hospitalization. A Health Emergency is a precipitous event which requires ongoing rehab or advanced care. A Health Care Emergency can also include a situation in which Your mental health needs change dramatically over a period of several days and You need immediate and continuing psychiatric intervention. In a Health Care Emergency, You need urgent, advanced care not available at the Home. Care during a Health Care Emergency is for the purpose of prolonging Your life. In such cases, if You provide written notice to LarMax that You are vacating the Home, Your financial obligations will cease on the later of (i) the day that You remove all personal belongings from the Home or (ii) the date that You deliver written notice to LarMax. Death is not a Health Emergency as it does not involve medical means to prolong life. The standard 30 day Notice requirement applies upon death. The Agreement states that Notice is deemed to have been given as of the date of death, therefore, in that event, You do not need to give written Notice in order to start the 30 day period. While we will use our best efforts to release Your room prior to the end of the 30 day period, in which case Your obligation to pay rent will stop as of the date the unit is reoccupied, there are no assurances that will happen. In the event that the room is not released, You acknowledge that You are responsible for the full rent for the 30 day period. If You have any questions at any time about this Addendum or any other section of Your Resident Agreement, please ask the person signing the Agreement on behalf of LarMax or a Managing Member of LarMax. The staff, who are excellent caregivers, are not trained to answer Your questions about legal Agreements nor are their answers binding on LarMax. This Agreement may be amended only by a written document executed by You and by a Managing Member or authorized agent of LarMax. Agreed and Accepted: __________________________________ LarMax Homes, LLC ________________________________ Resident (“You”) or Resident’s Legal Representative By: ___________________________ Its: ___________________________ 86 | P a g e EXHIBIT 3: OUTBREAK REPORTING REQUIREMENTS Virginia Outbreak Reporting Requirement for Facilities and Programs What are the legal requirements for facilities and programs to report outbreaks? Section 32.1-37 of the Code of Virginia requires certain facilities and programs to report outbreaks to the local health department. The most recent update to this requirement went into effect on July 1, 2008. Who is required to report? The person in charge of any residential or day program, service, or facility licensed or operated by any agency of the Commonwealth, school, or summer camp is required to report. This includes child care facilities, assisted living facilities, correctional and other detention facilities, mental health programs, and other group settings where outbreaks of illness may occur. Facilities licensed by the health department (hospitals and nursing homes) as well as physicians and directors of laboratories have always been required to report diseases to the health department. What diseases should be reported? An unusual level of activity of any illness that may be spread from one person to another or that may be caused by a common exposure should be reported. The diseases that most commonly cause outbreaks in group settings are respiratory illnesses such as influenza, gastrointestinal illnesses that cause vomiting and/or diarrhea, and rash illnesses such as chickenpox or scabies. The local health department should be notified when an outbreak is suspected, even if no specific disease has yet been diagnosed. What is an outbreak? An outbreak is the occurrence of more cases of disease than expected. There is no strict definition of an outbreak or specific number of cases that need to occur to be considered an outbreak. How does a facility/program director know if an outbreak is occurring? If people who work in a facility or program sense that more people are sick with similar symptoms than is usually seen, then an outbreak should be reported to the local health department. Many facility directors have already been doing this, even prior to the new law going into effect. Which health department should be contacted? How should they be contacted? The local health department serving the city or county in which the facility or program is located should be telephoned immediately if an outbreak is occurring. Contact information for Virginia’s health districts and their component city and county health departments is available at www.vdh.virginia.gov/lhd/ What will the health department do when they receive an outbreak report? Health department staff will collect and assess information about each ill person, such as the date illness began, symptoms experienced, and exposure history. Specimens may be collected for laboratory testing. The health department might need to interview people at the facility or program, both those who are ill and those who have not been ill, to identify factors that may be associated with illness. Most importantly, the health department will recommend steps to follow to stop the outbreak and reduce the risk of disease. July 1, 2008 87 | P a g e EXHIBIT 4: DISCHARGE NOTIFICATION AND STATEMENT RESIDENT'S NAME: ___________________________ HOUSE: ___________________________ Method of notification: 1. Date of discharge notification to resident: 2.a. Date of discharge notification to legal representative, if any: Name of legal representative: 2.b. Method of notification: Date of discharge notification to designated contact person, if any: Name of Method of designated contact person: notification: 3. Emergency or Regular Discharge: ___________________________________________________ 4. Reason(s) for the discharge: 5. Actions taken by the facility to assist the resident in the discharge and relocation process: 6. Date of the discharge: Destination (name and address): 7. Date discharge statement provided (or mailed, optional if emergency) to resident, legal representative and designated contact person: Signed by: (Licensee or Administrator) Date: 88 | P a g e EXHIBIT 5: ELOPEMENT DRILL OR POST ELOPEMENT CHECKLIST Drill or Actual Elopement: ____________________ Date: Time: Resident Name: Resident Missing Time: ___________(AM/PM) Room # Resident Found Time: ___________ (AM/PM) Circle the following Yes or No 1. Did staff verify resident was not signed out? Y N 2. Did staff check house? Y N 3. Did staff notify Director of Operations? Y N 4. Was the Director of Nursing and Administrator notified? Y N 5. Was a full search of the facility and grounds implemented? Y N 6. Were the police notified? Y N 7. Was search called off when resident was located? Y N 8. Was resident examined when located? Y N 9. Was resident physician notified when resident was discovered missing? Found? YY N N 10. Was family and/or responsible party notified when resident was discovered missing? Found? Y Y N N 11. Was Incident/event report completed? Y N 12. Did the alarm system function (if an egress system was in place)? Y N Name of person completing report Title of Person Completing Report: ______________________________________________ 89 | P a g e