symptom management of palliative patients in the ICU
Symptom Management in
Palliative ICU Patients
With a Focus on Pain, Dyspnea, and
Addressing in the Palliative Withdrawal of
Ventilatory Support in the Awake Patient
Mike Harlos MD, CCFP, FCFP
Professor and Section Head, Palliative Medicine, University of Manitoba
Medical Director, WRHA Adult and Pediatric Palliative Care
http://palliative.info
Objectives
• Appreciate the common physical symptoms experienced by palliative patients in the ICU
• Review the common approaches for symptom control at the end of life, particularly pain and dyspnea
• Discuss therapeutic considerations prior to ventilator withdrawal especially in the awake patient
The presenter has no conflict of interest to disclose
There are no “ do-overs ” in managing a death
Addressing Comfort During
Palliative Withdrawal Of Life-
Sustaining Ventilatory Support in the Awake Patient
Assumptions
• the circumstances being considered pertain to patients expected to die without support (‘terminal wean’) rather than a trial of weaning for potential ICU discharge
• may include patients with stenting endotracheal tubes for obstructing tumour, with normal resp drive and strength
• in response to the informed request of the awake and competent patient or their proxy/surrogate decision maker
• focuses on the practical/clinical considerations involved in ensuring comfort during withdrawal of ventilator support, particularly in the alert patient
Examples of Our Palliative Care Experiences
• 74 yo man with multisystem failure due to primary amyloidosis
respiratory failure, on dialysis, TPN, pressor infusion
transferred directly from SBGH ICU to a farm two hours out of town on which he was born, and which his family homesteaded.
• 52 yo woman with untreatable obstructing mediastinal tumour, in
ICU with stenting endotracheal tube, requesting extubation
• 63 yo man with obstructing laryngeal tumour, intubated in spite of clear wishes to the contrary after collapsing in the community with acute obstruction
once he awoke in SICU he demanded extubation
wanted no meds given – wanted to say goodbye to his children with his own voice if possible
• 71 yo man with advanced ALS, locked-in (only motor function was right lateral gaze of the right eye), wanting vent withdrawal in the home
General Considerations In Withdrawing Ventilatory
Support In The Awake Patient Expected To Die
• facilitating saying good-bye to family and friends, and perhaps the health care team
• the concept of picking a date and time of death may seem surreal
• the potential for severe distress is very real – and predictable
• very challenging to gauge potential for patient to breathe unsupported after withdrawal
not uncommon for the person who “never triggers the vent” to breathe for hours or days following withdrawal
Exploring Issues/Concerns With Patient, Family,
Team Prior To Withdrawal
• difference between withdrawing ventilator and euthanasia
allowing the death to unfold naturally from the underlying illness, as it would have done
• the issue of “playing God”
• staff feelings of moral/professional/religious compromise
• need for pre-briefings, de-briefings, education, mediation, supportive counseling
• what they can expect to see
• the outcome is not always certain
How Alert Is The Patient?
• if alert and no CNS impairment (such as with ALS or an obstructing tumour stented with an ET tube) must ensure a deep level of sedation prior to beginning withdrawal of ventilatory support
• if the patient has suffered a devastating neurological injury and is deeply comatose, there is less potential for experiencing air hunger
Anticipatory (Preemptive) vs. Reactive Medications
• reactive dosing essentially requires suffering
• the impact of the medication delivery system must be considered in reactive dosing, e.g.
PCA bolus on a pump with long tubing, vs. manual push into port near the patient
• pharmacokinetics of different opioids not always taken into consideration when planning reactive dosing
• pharmacokinetics of infusions for anticipatory dosing also not always considered – loading dose needed
• the concept of "anticipatory dosing" (as opposed to reactive dosing) should guide clinicians in the use of sedation and analgesia at the end of life
• the rapid withdrawal of mechanical ventilation is an example of the need for anticipatory dosing
• reactive dosing not sufficient
• as a general rule, the doses of medication that the patient has been receiving hourly should be increased by two- or three-fold and administered acutely before withdrawing mechanical ventilation
• Slow vs. Fast Withdrawal?
“the only justification for gradual reduction of ventilatory support is to allow time to control dyspnea through the titration of medications”
• Extubate or not?
considerable variation RE whether to extubate; each circumstance should be approached individually
extubation before death is associated with higher family satisfaction
(Hinkle LJ, Bosslet GT, and Torke AM. Factors associated with family satisfaction with end-of-life care in the ICU: a systematic review. Chest.
United States; 2015;147(1):82-93)
Titration of Analgesics and Sedatives: increase in response to:
1.
patient's request
2.
signs of respiratory distress
3.
physiological signs: unexplained tachycardia, hypertension, diaphoresis,
4.
facial grimacing, tearing, vocalizations with movements, turns or other nursing care
5.
restlessness
The total amount of drugs required for any individual patient may far exceed any preconceived notions of “usual”
Paraphrased : If the patient tells you they’re in distress, or it looks like they’re in distress, treat with an effective dose of medication
Does a Maximal Dose of Opioids or Sedatives Exist?
No.
The goal of palliative care is to provide relief of pain and suffering and whatever the amount of drugs that accomplishes this goal is the amount that is needed for that individual patient.
Paraphrased : The correct dose of an opioid or sedative is the one that works, proportionate to distress and within acceptable adverse effects
Should Analgesics and Sedatives be Administered in Response to Signs and Symptoms of Pain and Suffering, or Before They
Begin?
Support for both approaches exists among lntensivists on this panel.
Paraphrased : Yes. If the patient is in pain, treat the pain. If you’re about to do something that will likely hurt, treat preemptively.
Onset of Opioid Effect
Ref: Geriatric Anesthesiology 2nd Edition 2008; Jeffrey Silverstein (Editor),
Alec Rooke (Editor), J. G. Reves (Editor), Charles H. McLeskey (Editor);
Springer Publications
Determined by:
• route of administration
• dose
• pharmacokinetics determining plasma concentrations over time
• rate of blood-brain equilibration between the plasma and the site of drug effect
Ref: Geriatric Anesthesiology 2nd Edition 2008; Jeffrey Silverstein (Editor), Alec
Rooke (Editor), J. G. Reves (Editor), Charles H. McLeskey (Editor); Springer
Publications
Barr J et al; American College of Critical Care Medicine. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med; 2013;41(1):263-306.
How Effectively Can You Gauge Distress?
• locked-in / advanced ALS – may lack usual visual cues of distress – these patients also have virtually no capability for unsupported breathing
• vital signs (tachycardia or elevated blood pressure) may not reliably reflect discomfort
medication effects (e.g. scopolamine) or physiologic changes (e.g. hypoxia) may result in changes in vital signs without patient necessarily experiencing discomfort
• the inability to adequately gauge distress compels an effective preemptive approach to ensure that air hunger could not possibly be present
• 71 yo man “locked-in” with advanced ALS dx approx 18 mo. earlier
• trach/vent support at home; very capable spouse as main caregiver
• consistently expressed wish to be withdrawn from ventilator once communication severely impaired – that time had come
• still had right lateral movement of his right eye; through yes/no questions could indicate that he wanted withdrawal
• did not want to leave home – however it was not clear that a home vent withdrawal had been done before in Winnipeg
• resp team described absent ability to trigger vent
• Challenges
could not assess distress due to locked-in state, severe motor impairment
published protocols describing terminal vent withdrawal relied on morphine and on reactive dosing in response evidence of distress
local colleagues expressed significant concern with an approach involving aggressive administration of opioids and sedatives
• Outcome
reviewed plan of using high-dose opioids and midazolam with
Ethics (including international discussion list), CPSM, Medical
Examiner – all were supportive
attended patient’s home the day after Halloween (per patient’s request – wanted to see children enjoying Halloween); lots of family present, priest present
administered morphine, midazolam, haloperidol, scopolamine
withdrew ventilatory support; deceased 10 minutes later
Respiratory Physiology For The Palliative MD
• opioids
• CNS pathology
• ALS
Brain (or brainstem) says “ breathe ”
Nerves transmit this message on to the muscles
• Muscular dystrophy
• Pulm. fibrosis
Muscles do the work of breathing
Lungs Exchange Air
•
Severe blood loss
• Mitochondrial disorders
Blood Transports Oxygen
Tissues Use Oxygen
Series circuit wiringif one component fails, they all fail
• opioids
• CNS pathology
Brain (or brainstem) says “ breathe ”
•
•
•
•
•
ALS
Muscular dystrophy
Severe blood loss
Mitochondrial disorders
Nerves transmit this message on to the muscles
Pulm. fibrosis
Muscles do the work of breathing
“zero” capability in any element means zero overall
Lungs Exchange Air
“zero” not that common
– e.g. locked-in ALS
Blood Transports Oxygen
Tissues Use Oxygen
in the context of zero resp. capability due to severe illness, opioids cannot make zero worse than zero – no fatal or compromising dos e
must err on the side of aggressive dosing in vent withdrawal
• Prepare for addressing:
dyspnea
anxiety
secretions
nausea/vomiting from opioid boluses
seizures?
potential for temporarily needing oral airway after extubation – at least until best positioning found
post-extubation stridor?
(Khemani RG, Randolph A, and Markovitz B. Corticosteroids for the prevention and treatment of post-extubation stridor in neonates, children and adults. Cochrane Database Syst Rev. England;
2009;(3))
• families should be prepared for certain physical changes that can’t be prevented – cyanosis, mottling, occasionally some movements
My Usual Approach
1.
Continue existing opioid and sedative infusions
2.
Approx. 30 minutes prior to beginning the withdrawal, administer intravenously:
morphine (dose depends on existing opioid tolerance), or fentanyl (if already on a fentanyl infusion)
methotrimeprazine – e.g. 25 mg IV – antinauseant, sedative
scopolamine 0.6 mg
midazolam – typically 2.5 – 5 mg; depends on existing tolerance
– The patient should now be deeply asleep –
3.
Reduce ventilatory support “by about half” for 10 minutes (Resp.
Therapists take care of the details of this for me)
4.
Consider repeating midazolam and morphine at this time, depending on assessment of patient’s level of sedation
5.
Discontinue ventilator
6.
If needed administer “unit doses” of fentanyl + midazolam – premixed in individual syringes (e.g. 100 mcg fentanyl plus 2 mg midazolam) – in response to distress
What Is The Correct Opioid Dose For Safely
Ensuring Comfort During Terminal Wean/Extubation?
Somewhere in here
Not
Enough
Too
Much
Put another way – there are only three doses of opioids in such circumstances:
1.
Not enough
2.
Just right
3.
Too much
Not enough is unconscionable; just right is unrealistic.
If we are going to err on the side of allowing a suffocating death versus potentially hastening a relentless and certain progression towards a natural death, which side should we err on?
Whose needs are being met by conservative dosing?
DOCTRINE OF DOUBLE EFFECT
From Principles of Biomedical Ethics, Beauchamp & Childress; 7 th Ed. 2013
Four conditions or elements that must be satisfied for an act with a double effect to be justified. Each is a necessary condition , and together they form sufficient conditions of morally permissible action:
1.
The nature of the act . The act must be good , or at least morally neutral (independent of its consequences)
2.
The agent's intention . The agent intends only the good effect .
The bad effect can be foreseen, tolerated, and permitted, but it must not be intended.
3.
The distinction between means and effects . The bad effect must not be a means to the good effect . If the good effect were the direct causal result of the bad effect, the agent would intend the bad effect in pursuit of the good effect.
4.
Proportionality between the good effect and the bad effect . The good effect must outweigh the bad effect . That is, the bad effect is permissible only if a proportionate reason compensates for permitting the foreseen bad effect
•
considerations about appropriate opioid doses in terminal extubation are pretty much the only circumstances where the
Doctrine of Double Effect
feels potentially relevant in palliative care practice
•
personal experience – not one circumstance where I felt I needed to “invoke the Doctrine”
• studies on post-ICU patients showed that 82% remembered pain or discomfort associated with the endotracheal tube and 77% remembered experiencing other moderate to severe pain during their ICU stay
• pain assessment in the non-verbal patient challenging
Approach To Pain Control in the Palliative Patient
1.
Thorough assessment
• History – (challenging in the non-communicative patient) - including detailed description of pain; psychosocial, spiritual, & cultural context; concerns about what the pain means; medication history
• Physical Examination
2.
3.
4.
Pause here - discuss with patient/family the goals of care, hopes, expectations, anticipated course of illness. This will influence consideration of investigations and interventions
Investigations – X-Ray, CT, MRI, etc if they will affect approach to care
Treatments – pharmacological and non-pharmacological; interventional analgesia (e.g. spinal); RadTx
5.
Ongoing reassessment and review of options, goals, expectations, etc.
American College of Critical Care Medicine Clinical practice guidelines: Recommendations RE Pain Assessment i.
We recommend that pain be routinely monitored in all adult ICU patients ii.
The Behavioral Pain Scale (BPS) and the Critical-Care Pain
Observation Tool (CPOT) are the most valid and reliable behavioral pain scales for monitoring pain in medical, postoperative, or trauma
(except for brain injury) adult ICU patients who are unable to selfreport and in whom motor function is intact and behaviors are observable. iii.
We do not suggest that vital signs (or observational pain scales that include vital signs) be used alone for pain assessment in adult ICU patients iv.
We suggest that vital signs may be used as a cue to begin further assessment of pain in these patients, however
A Visual Analogue Scale Developed For Nonverbal Children –
May Be Used In Nonverbal Adults
TYPES OF PAIN
NOCICEPTIVE
Somatic
• bones, joints
• connective tissues
• muscles
• sharp
• dull & aching
• can localize site
• may be worse with movement
(“ incident pain
”)
NEUROPATHIC
• difficult to describe; not a typical “pain”
• numb; burning; tingling;
•
Visceral
Organs – heart, liver, pancreas, gut, etc.
• may be crampy, or crawling; stabbing; etc
• allodynia
• consider it as a possible element of any difficult pain syndrome dull & aching
• referred pain
• difficult to localize
• important to have at least a working assumption of the underlying pain mechanism
not all pain syndromes are expected to respond fully to opioids – specifically neuropathic pain
• difficult to diagnose neuropathic pain if communication limited.
Consider if:
previous diagnosis of neuropathic pain
solid tumours (not just ones involving nerve plexus or spinal cord)
predisposing medical conditions or medications (diabetes mellitus, chemotherapies such as cisplatin etc)
ischemic limbs (nerves are damaged by the ischemia)
bone mets – increasing evidence for a neuropathic element
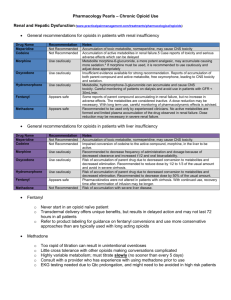
Opioid Selection
• for parenteral administration, typically use morphine, hydromorphone, or fentanyl
• selection depends on comorbidities, previous adverse reactions
• morphine and hydromorphone have active metabolites that accumulate in renal insufficiency and are implicated in the development of opioid-induced neurotoxicity
• fentanyl has no known active metabolites; preferred in renal insuff
• parenteral methadone would be a very useful medication, however not available in Canada (is available in UK, Europe, Australia, USA)
• methadone: NMDA receptor antagonism; may help in neuropathic pain, situations of high opioid tolerance, or opioid-induced neurotoxicity
caution RE drug interactions, QTc interval prolongation
no known active metabolites; preferred in renal insuff
Basic Conversions – Starting Points For Consideration
Drug Conversion morphine:hydromorphone
5 mg morphine = 1 mg hydromorphone fentanyl:morphine (parenteral)
100 mcg (0.1 mg) fentanyl = 10 mg morphine morphine:oxycodone
1.5 mg morphine = 1 mg oxycodone methadone:anything
Notes hydromorphone is about 5 times more potent than morphine fentanyl is about 100 times more potent than morphine oxycodone is about 1.5 times more potent than morphine
Context dependent
Cautions:
• particularly in high doses, tolerance to one opioid will not be fully crossed over to another ( incomplete cross-tolerance ) – consider reducing converted dose
• in the context of opioid-induced neurotoxicity, there are no conversion ratios
Parenteral Adjuvants To Consider For Neuropathic Pain
1.
Ketamine (NMDA receptor antagonist)
•
Taylor M, Jakacki R, May C, Howrie D, and Maurer S. Ketamine PCA for Treatment of End-of-Life Neuropathic Pain in Pediatrics. Am J Hosp Palliat Care. 2014
• Kim K, Mishina M, Kokubo R, Nakajima T, Morimoto D, Isu T, Kobayashi S, and
Teramoto A. Ketamine for acute neuropathic pain in patients with spinal cord injury.
J Clin Neurosci. Scotland; 2013;20(6):804-7.
2.
Dexmedetomidine (alpha-2 agonist)
•
Hilliard N, Brown S, and Mitchinson S. A case report of dexmedetomidine used to treat intractable pain and delirium in a tertiary palliative care unit. Palliat Med.
England; 2015;29(3):278-81
• Ghobadifar MA, Pourghashdar F, Akbarzadeh A, and Mosallanejad Z. Combined use of intrathecal opioids and dexmedetomidine in the management of neuropathic pain. Korean J Pain. Korea (South); 2015;28(2):156-7
•
O'Neil T, Rodgers PE, and Shultz C. Dexmedetomidine as adjuvant therapy for acute postoperative neuropathic pain crisis. J Palliat Med. United States;
2014;17(10):1164-6
Spectrum of Opioid-Induced Neurotoxicity
1.
discontinue the offending opioid
2.
aggressive hydration; may need to monitor electrolytes
3.
use prn doses of opioidnaïve doses of fentanyl – e.g. 50-100 mcg IV q15 min prn (unless it is the offending opioid)
4.
after several hours, determine a fentanyl infusion rate
5.
consider: ketamine (NMDA antagonist) to reduce extreme opioid tolerance
Dyspnea In The Palliative Patient
• an uncomfortable awareness of breathing… an experience of breathlessness rather than an observation of increased work of breathing
• increasing incidence as death nears; can escalate quickly resulting in missed opportunities for comfort measures
• severe dyspnea in the context of advances terminal illness usually reflects imminent death
• n = 96 patients mechanically vented > 24h
• dyspnea evaluated on a “yes–no” basis
• if yes, it was followed by a visual analog scale (VAS) and descriptor choice (“air hunger” and/or “respiratory effort”)
• Pain & anxiety also assessed by VAS
• 47% reported dyspnea
• dyspnea was significantly associated with anxiety (odds ratio 8.84)
• adjusting ventilator settings improved dyspnea in 35% of patients
No dyspnea
Dyspnea - resp effort
Dyspnea - air hunger
Dyspnea - both
Dyspnea - neither
Addressing Dyspnea In The Palliative Patient
• gold standard for assessment is patient report, as with any experiential symptom
• in the non-verbal patient, the usual clinical assessment is a combination of:
work of breathing – which may be absent in a ventilated patient (increased rate, accessory muscle use)
evidence of distress (fearful look, restless, tachycardia)
-
“gut feeling” on the part of clinicians and family
• in the dying palliative patient in ICU the most likely situation will be that of a restless patient who seems generally uncomfortable, for uncertain reasons
• should rule out obvious reversible causes of distress, and treat with opioids; will address pain and air hunger
American College Of Chest Physicians Consensus
Statement On The Management Of Dyspnea In Patients
With Advanced Lung Or Heart Disease - 2010
• Regarding fear of respiratory depression –
• higher doses of opioids and benzodiazepines used in the withdrawal of life-sustaining treatment were not associated with a decreased time from withdrawal of life support to death
• Of 11 studies providing information on ABGs or O
2 sat, only one study reported any significant changes in oxygenation after opioid administration
• Recommend that :
• Oral and/or parenteral opioids can provide relief of dyspnea.
• Opioids should be dosed and titrated for the individual patient with consideration of multiple factors (e.g., renal, hepatic, pulmonary function, and current and past opioid use) for relief of dyspnea.
• Official American Thoracic Society Statement: Update on the Mechanisms, Assessment, and Management of
Dyspnea – 2012
Opioids have been the most widely studied agent in the treatment of dyspnea. Short-term administration reduces breathlessness in patients with a variety of conditions, including advanced COPD, interstitial lung disease, cancer, and chronic heart failure
• Canadian Thoracic Society Clinical Practice Guideline
2011: Managing Dyspnea In Patients With Advanced
Chronic Obstructive Pulmonary Disease
“We recommend that oral (but not nebulized) opioids be used for the treatment of refractory dyspnea in the individual patient with advanced COPD”
• may reduce overall oxygen demand
• “The administration of sedatives (midazolam and morphine) has been associated with decreases in oxygen demand and the attenuation of the cardiopulmonary response associated with increased work of breathing”
• see also: Endoh H et al; Effects of naloxone and morphine on acute hypoxic survival in mice . Crit Care Med; 1999;27(9):1929-33
significantly lower oxygen consumption and improved survival in morphine treated rats subjected to acute hypoxic hypoxia
Common Concerns About Aggressive Use of Opioids at End-Of-Life
• How do you know that the aggressive use of opioids for dyspnea doesn't actually bring about or speed up the patient's death?
• “I gave the last dose of morphine and he died a few minutes later… did the medication cause the death?”
1. Literature: the literature supports that opioids administered in doses proportionate to the degree of distress do not hasten death and may in fact delay death
2. Clinical context: breathing patterns usually seen in progression towards dying (clusters with apnea, irreg. pattern) vs. opioid effects (progressive slowing, regular breathing; pinpoint pupils)
3. Medication history: usually “the last dose” is the same as those given throughout recent hours/days, and was well tolerated