Impact of health comorbidities on ACC costs (PPT 1.5
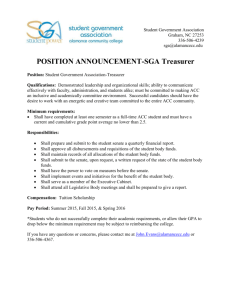
advertisement

The Impact of Co-morbidity ACC Service Utilisation & Costs 2012 - 2025 Dr Barry Gribben CBG Health Research Dr John Wren Principal Research Advisor ACC Lauren Prosser Senior Policy Advisor ACC 2nd ACHRF Auckland, New Zealand 8 November 2012 The Questions WHAT is the effect of a health co-morbidity on ACC clients ? ˃ injury treatment claim rates (utilisation) ˃ duration of claim ˃ costs over time WHAT are the cost effects on an aging population ? WHAT are the policy implications ? The Process BUILT on the pilot studies reported in 2010 (Wren & Mason) LINKED Primary Health Care data (GP Practice) with Ministry of Health & ACC data using New Zealand NHI ˃ Random sample of 337,665 people ˃ Sample representative of the New Zealand population Descriptive & Multivariate Statistical Analysis Co-morbidities Asthma Chronic obstructive pulmonary disease Ischaemic heart disease Heart failure Diabetes mellitus Mental health condition Cancer diagnosis Osteoarthritis Hypertension Variables & Interactions Age Sex Ethnicity Socio-economic status (New Zealand social deprivation index) Treatment utilisation Claims duration ACC Costs Headline Statistical Results Multivariate Model Analysis Presence of a health co-morbidity was found to have a strong statistically significant (95%) association with: ˃ increased service utilisation ˃ higher costs The effects were independent of, and additional to, normal health cost effects typically associated with age, gender, ethnicity & socio-economic status Headline Statistical Results Presence of one or more health co-morbidities showed … ˃ 28% more claims ˃ 346% higher lump sum payments ˃ 59% higher medical treatment costs ˃ 39% more weekly compensation costs OVERALL 59% more total ACC cash costs across all cost categories Cost relativity … stronger relativity for some than others Average total cost per person per year (95% CI) Average total cost per annum NZD 1400 1200 1000 800 600 400 200 0 Yes No Osteo-arthritis Yes No Stroke Yes No Hyper-tension Yes No Mental Health Yes No IHD Yes No Heart Failure Yes Cancer No Yes Asthma No Yes No Diabetes Claim Utilisation Claims Utilisation vs. Number of Co-morbidities 2.50 2.00 Claims per annum 1.50 1.00 0.50 0.00 0 1 2 3 4 Number of co-morbidities present 5 6 7 Medical Treatment Cost Medical Treatment Costs vs. Number of Co-morbidities $500 $450 $400 $350 Medical $300 Treatment $250 Cost $200 $150 $100 $50 $0 1 2 3 4 Number of co-morbidities present 5 6 7 Total Annual Cost Total Annual Cost vs. Number of Co-morbidities $3,000 $2,500 Total Annual Cost $2,000 $1,500 $1,000 $500 $- 0 1 2 3 4 Number of co-morbidities present 5 6 7 Based on the analysis 10.7% Total Annual ACC Cost is attributable to presence of co-morbidities in the New Zealand population 276 million $ (NZD, 2011) Ageing Effects Mean $ NO co-morbidity Average total cost per person Age group co-morbidity vs. no co-morbidity Mean $ co-morbidity 2000 Mean cost per annum per person 1800 1600 1400 1200 1000 800 600 400 200 Excess cost is the area of the gap between the two lines – largest gap is in the working age population 0 Age group Modelling Ageing Effects to 2025 Population by age group with co-morbidity vs no co-morbidity 160,000 Without co-morbidity 140,000 With co-morbidity 100,000 80,000 Expect this area to get bigger 60,000 40,000 20,000 Age group + 90 5- 9 10 -1 4 15 -1 9 20 -2 4 25 -2 9 30 -3 4 35 -3 9 40 -4 4 45 -4 9 50 -5 4 55 -5 9 60 -6 4 65 -6 9 70 -7 4 75 -7 9 80 -8 4 85 -9 0 0 04 Number of people 120,000 Costs Attributable to Co-morbidities 14.0% Percentage of total ACC costs 12.0% 10.0% 8.0% 6.0% 4.0% 2.0% 0.0% no change 1% growth 2% growth 2012 10.66% 10.71% 10.77% 2015 10.67% 10.83% 11.00% 2020 10.96% 11.43% 11.91% 2025 11.25% 12.06% 12.72% Conclusions Presence of a wide range of health co-morbidities in the population has a real effect on injury compensation treatment utilisation volumes and costs To 2025, 10.7% to 12.7% of total annual ACC costs is estimated to be attributable to presence of co-morbidities in the population It appears that although aging of the population means more people have co-morbidities, this is counterbalanced by relatively fewer people being in the age groups where the cost differences are greater Results are consistent with recent research from NCCI in America about working age effects Policy response Confirms and quantifies our assumptions – ACC appears to be paying more than required to meet a person’s injury-related needs But how big is the problem? Within current legislative constraints? ACC is liable for injury costs unless an unrelated comorbidity is ‘wholly or substantially’ the cause of the person’s ongoing incapacity Where does the cost burden fall in the ACC Accounts? What is the impact on liability? Policy questions: How can ACC be smarter at managing the additional costs associated with co-morbidities? Should the costs be shared with others, eg individuals or other agencies? How can ACC continue to deliver a client-centred service? No silver bullet – distinguishing injury and non-injury related needs is difficult, particularly in the context of different funding systems and philosophies Working through the policy issues and options Potential responses could include: cost-sharing arrangements targeted risk and claims management integrated assessment and services injury prevention initiatives reviewing assessment of individual entitlements status quo? For further information Gribben, B. & Wren, J. ( 2012) The Impact of Health Comorbidities on ACC Injury Treatment and Rehabilitation Utilisation and Costs, and cost estimate to 2025 of effects in an aging population. CBG Health Research and ACC Research, Sep 2012. Wren, J. & Mason, J. 2010. Results of Three Pilot Studies Exploring & Quantifying Health Co-morbidity Effects on ACC Injury Treatment Utilisation and Costs. ACC. Additional Slides Health Literature Pre-existing health co-morbidity effects on increased health service utilisation well-documented in recent World Health Organisation (WHO) reports ˃ Injured people are different from the non-injured population in terms of pre-existing morbidity ˃ Patients with higher numbers of co-morbidities utilise injury services more than patients with lower co-morbidities. Cameron, Prudie, Kliewer et al., 2005) Health co-morbidity (ICD9-CM Chapter) Source: Adapted from Cameron et al, 2005. Tables 4 and 5 respectively. Rate Ratios* Injured/ Non-Injured *Adjusted for age, sex and place of residence * Hospital Admissions Physician Claims per 1000 person years Mental Health disorders 9.31 3.50 Injury and poisonings 3.68 2.72 Blood diseases 3.36 1.53 Endocrine and metabolic 2.79 1.38 Musculoskeletal disorders 2.61 1.76 Nervous system diseases 2.35 1.42 Respiratory diseases 1.98 1.38 Circulatory diseases 1.70 1.21 Health Literature Role of Mental Health, Alcohol and Psychological Traits “There appears to an aetiological link between mental health conditions and injury, particularly in relation to risk-taking behaviours, alcohol misuse, and psychological traits such as impulsivity, sensation-seeking, and risk-perception.” (Cripps & Harrison, 2008. Briefing report for the Australian Institute of Health and Welfare) Workers Compensation Literature Increased injury risks, higher medical treatment costs (including pharmaceutical services), workers compensation costs, and poor work performance (presenteeism) have consistently been associated with specific lifestyle risk factors such as tobacco use (current and previous), obesity, stress, and lack of regular physical activity among working people in a variety of settings (Studies published by Health Management Research Centre, and Others) Workers Compensation Literature Considerable confidence the excess risk from health comorbidities accounts for at least 25% to 30% of medical costs per year across a wide variety of companies, regardless of industry or demographics The biggest cost factors are the cost of extra treatment utilisation, and medical costs associated with the complications of a co-morbidity (Studies published by Health Management Research Centre) ACC Claims Costs Highly skewed All Results Significant at 95% Multivariate Analysis Future Cost Calculation The proportion of ACC costs attributable to chronic illness in any given out year is a function of: the population structure (the matrix Nij) the number of years from our baseline, n. Pij, r, $ccij and $nccij are all constants calculated earlier, or assumed. P f ( N , n) n N P ( 1 i ) ($ccij $nccij ) ij ij ij n n N ($ cc P ( 1 i ) $ ncc ( 1 P ( 1 i ) ) ij ij ij ij ij ij