PENETRATING NECK INJURIES
advertisement
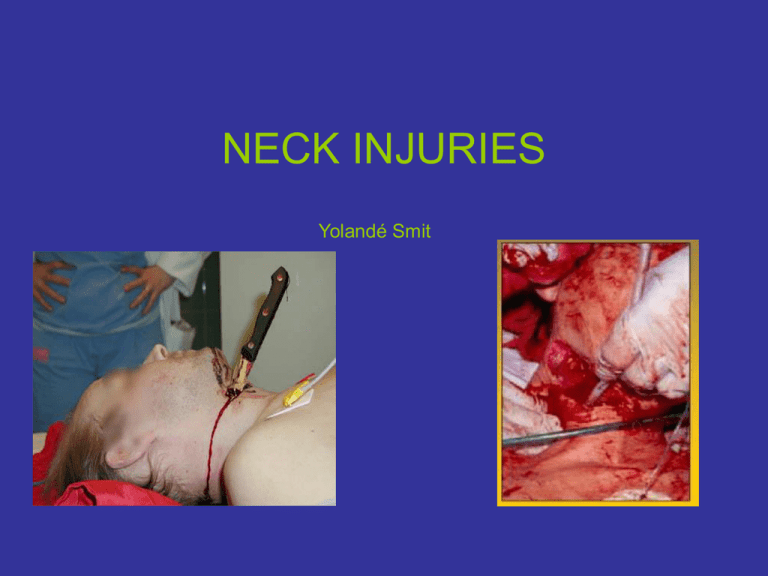
NECK INJURIES Yolandé Smit Perspective • 5 – 10% of all trauma cases • 30% associated with injuries outside neck • Leading cause of immediate death is exsanguination • Esophageal injuries represents the most frequently missed injury and may be leading cause of delayed death • Compound difficulties in evaluation & Mx is the complicated anatomy - dense concentration of vital structures in a small space • Ongoing debate : mandatory vs selective exploration HISTORY • In 1552, Ambrose Pare ligated CCA. • WW1 – mortality 60% • WW11 - mandatory exploration, mortality 47% • Continuous advances in anaesthesia and perioperative management – mortality 6% for early vs 35% for late exploration • Currently 2-6% Mechanism of Injury • Penetrating • Blunt • Strangulation/ near-hanging Penetrating Trauma (1) • 5-10% of all traumatic injuries • GSW – High velocity – Low velocity (50% lower incidence of significant lesions) • Stab wounds • Miscellaneous (shrapnel, impalement) Penetrating Trauma (2) Incidence • • • • • • • Location Arterial Venous Tracheolaryngeal Pharyngoesophegeal Spinal cord Neuroligical, other Thoracic duct Total 1275 patients Percentage % 12.8 11.3 10.1 9.6 3 3.4 0 Blunt Trauma • Vascular injuries are rare but represent one of the most under diagnosed injuries • Aerodigestive injuries are rare in comparison to penetrating injuries but can cause acute AW compromise and delayed complications • Causes: – – – – – Motor vehicle collisions ‘Clothesline’ injuries Assault Strangulation Sports injuries Strangulation • Near hanging – Complete/judicial – Incomplete – Typical – Atypical • Manual Strangulation • Ligature Strangulation • Postural Strangulation Strangulation (2) Pathophysiology • High cervical fractures, complete cord transection, death • Venous congestion with stasis of cerebral blood flow leading to unconsciousness • Arterial occlusion with brain injury and death • Vagal reflexes contribute to fatal dysrythmias • Pulmonary sequelae Compression of AW doesn’t play as significant role in incomplete hanging as does vascular occl Anatomy Three components • Structural • Visceral collumn – Respiratory layer (trachea & larynx) – Alimentary layer (pharynx & esophagus) – Endocrine layer (thyroid & parathyroid) • Paired neurovascular bundle Anatomy Two fascial layers 1. Superficial fascia • • Beneath skin Contains platysma 2. Deep fascia • • • Investing layer Visceral layer Prevertebral Anatomy Prevertebral Fascia • Covers paraspinal structural components • Two layers/laminae: alar & prevertebral • Fans out to cover roots of brachial plexus and subclavian a • Axillary sheath Anatomy Visceral Fascia • Forms visceral compartment • Pretracheal anteriorly • Buccopharyngeal and retroesophageal posteriorly • Portion enclosing the strap muscles a.k.a middle cervical fascia • Space between buccopharyngeal and prevertebral fascia Anatomy Investing fascia • Envelopes Trapezius & SCM • Forms complete sheath of neck • Base of skull to sternum • Suprasternal space Anatomy Carotid Sheath • Loose aggregation of connective tissue • Visceral compartment medial • SCM anterolateral • Prevertebral fascia posteriorly Anatomy Fascial Layers: Importance • Superficial layer contains platysma: important surgical landmark • Tight fascial compartments may limit external hemorrhage from vascular injuries BUT easily compromises the airway • Danger space: mediastinits Anatomy Three Zones • ZONE 1- thoracic outlet – Cricoid cartilage to sternal notch • ZONE 2- Central – Cricoid to angle of mandible • ZONE 3 - Skull base – Angle of mandible to base of skull Anatomy Zones • Zones apply to neck anterior to anterior border of trapezius • Wounds to posterior triangle rarely associated with vascular, airway or digestive injury, except vertebral artery • Wounds through SCM or anterior triangle have high likelihood of injury • Decision making for diagnostic tests & surgical approach Anatomy Cervical arteries Anatomy Brachiocehalic A • 4-5 cm in length • Ascend obliquely to right of sternoclavicular joint • Divides into right common carotid and subclavian aa Anatomy Suclavian A • Passes behind SCM, Jugular vein and Vagus nerve • Three branches • Vertebral • Internal mammary • Thyrocervical trunk • Courses post to anterior scalene than crosses first rib to become axillary artery Anatomy Carotid A • Common carotid has no branches • Bifurcates to external and internal carotids at superior border of thyroid cartilage • Internal – no cervical branches • External – 8 branches Anatomy Vertebral A • First branch of subclavian • Extra-osseous until entering the transverse process of C6 (V1) • Intra-osseous from C6 – C2 (V2) • Distal extracranial top of C2 to base of skull (V3) INITIAL MANAGEMENT Initial Management Airway (1) Indications for immediate intubation • Apnoeic or near apnoeic patient • Comatose patient • Significant respiratory compromise (stridor, dysphonic with air hunger) • Rapidly expanding neck hematoma • Massive subcutaneous emphysema causing airway compression or distortion of trachea or larynx • Massive bleeding into airway Initial Management Airway (2) ‘Wait-and-see’ – If no immediate indication – Fastidious observation of clinical status – Equipment readily available – Prompt intubation if any evidence of expanding hematoma or enlarging neck sc emphysema Initial Management Airway (3) • Avoid BMV if possible • Oral intubation preferred – Without sedative in unconscious/ flaccid/near apnoeic patient – With sedation in uncooperative/agitated pt – RSI technique-of-choice – Difficult intubation anticipated: • ‘Brutane’ technique • Ketamine 1-2mg/kg IV Initial Management Airway (4) • Surgical airway last resort • Cricothyrotomy preferred to tracheostomy: – Time – Position of neck – Bleeding • If laryngeal injury suspected – Consider awake local tracheostomy – Cricothyroidotomy for emergencies – Fibreoptic laryngoscope only if prepared to emergently obtain surgical airway • Needle cricothyroidotomy + jet insufflation may be acceptable to temporize • Retrograde intubation and blind nasal intubation is contra-indicated Initial Management Airway (5) Pediatric considerations • Ideally with RSI • Fewer AW salvage techniques available: – Cricothyrotomy contra-indicated under 10 – Emergency tracheostomy difficult • Degree of AW obstruction after blunt trauma to larynx inversely related to degree of calcification, putting children at highest risk Initial Management Control bleeding • Local pressure – Proximal and distal control • Balloon tamponade with Foley’s catheter – Two catheters in supraclavicular zone1 • Immediate ED thoracotomy with aspiration of air from RV if cardiac arrest immediately before or after arrival in ED Initial Management Pitfalls • Do not probe wounds – Platysma penetration mandates evaluation in controlled fashion • Controversy about NGT – Tube may migrate from esophagus – Valsalva by patient may dislodge clot – Bloodstained Initial Management Immediate Surgical Exploration • • • • • INDICATIONS Severe active bleeding Shock not responding to fluids Rapidly expanding hematoma Absent radial pulse Evolving stroke Initial Management Complete Primary Survey • Thorough examination – Vascular: Hard signs of vascular injury – Airway: Stridor hoarseness, dyspnoea, sc emhysema Initial Management Secondary survey • Digestive tract – Dysphagia – Odynophagia – Hematemesis – Subcutaneous emphysema • Neurological: focal signs Further Management Further Management • If no indication for immediate surgical exploration, subsequent intervention based on : – clinical exam • Hard signs • Soft signs • No symptoms or signs – diagnostic testing Hard Signs • • • • • Pulsatile bleeding Expanding hematoma Not responding to resus Absent distal pulses Distal signs – Cold, pale limb – Stroke • Bruit • Airway obstruction Soft signs • • • • • • • • Venous bleeding Stable hematoma Responding to resus Diminished peripheral pulses Proximity to major artery Peripheral nerve deficit (brachial plexus) Hemoptysis/hematemesis Dysphonia/dysphagia Diagnostic Strategies • • • • • • • Stable patient with hard signs: exploration (diagnostic strategies to plan) Stable patient with soft signs/ asymptomatic: mandatory vs selective exploration (diagnostic strategies to aid in diagnosis) Is physical examination reliable? Consider: Resources Potential for injury Ability to serially exam Consequences of missed injury Diagnostic strategies • X-Rays – Chest: PT/HT, widened mediastinum, mediastinal air, elevated hemidiaphragm, FB – Neck: prevertebral air or swelling, sc air, FB • Gastrograffin swallow – All penetrating neck injuries due to high incidence of occult injuries • Endoscopy – If swallow (-), enhances sensitivity for penetrating esophageal injury Diagnostic Strategies • Arteriogram – Diagnostic – To plan surgery – Therapeutic • Laryngoscopy/ bronchoscopy – Hemoptysis/ hoarseness/ sc emphysema/ laryngeal tenderness or deformity • CT neck – Useful for evaluating laryngeal injuries – May play a role in the future as screening modality in diagnostic evaluation of AW & vascular injuries in asymptomatic pt Diagnostic strategies Airway/resus/assessment Stable Unstable Active hemorrhage Zone 1 Zone 2 Zone 3 Expanding hematoma Swallow Evolving stroke Arteriogram Endoscopy Swallow Explore Arteriogram + Endoscopy - Observe + Explore Embolize Observe