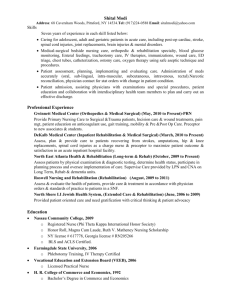
File - Bobbi Bowman Portfolio
advertisement

Grand Rounds NURS 441-Clinical Management of Rehabilitation Clients Purpose of Assignment To provide the student an opportunity to integrate previous knowledge from the sciences to the care of a client with a physical disability. Also, to provide the student with an opportunity to demonstrate critical thinking and independent judgments in managing care of a client with a physical disability Student Approach to Assignment The Clinical Management of Rehabilitation Client Grand Rounds Presentation offered me the opportunity to present a patient to my future colleagues and open dialogue up for a round table discussion atmosphere. The focus of the session was set by presenting past and pertinent health history, what the client’s chief reason for needing rehabilitation was and the psychosocial history that was relevant to her care. The notion of a working concept map was introduced in order to allow for other members of the group to provide input as to possible nursing diagnosis and rationale/ nursing interventions that were being utilized to support such diagnosis. Yet, another aspect of this presentation was to describe a diagnosis that has been a management problem and develop an alternative intervention. Reason for Inclusion of this Assignment in the Portfolio This essential portfolio presentation exemplifies some of the program's core behaviors that were met during my clinical rehabilitation experience. The following curricular objectives were highlighted: Critical Thinking Revises actions and goals based on evidence rather than conjecture Case in point: The patient utilized for this presentation has an wide-ranging past history which includes bronchitis, hypokalemia, anemia, morbid obesity, possible sleep apnea, fibromyalgia, chronic lymphedema, myasthenia gravis (diagnosed within last two years), atrial fibrillation with rapid ventricular response (diagnosed within the past year), obsessive compulsive disorder, chronic anxiety, depression, hyperlipidemia and congestive heart failure (also diagnosed within the past year). It should also be noted that she has an extensive history of falls. General debility was the admitting diagnoses with an increased focus towards lower extremity weakness and the inability to stand for periods greater than three minutes or ambulate with or without assistive devices for short distances. Her general debility is greatly related to the myasthenia gravis. The rehabilitation plan of action was to include physical therapy sessions to assistance with activity intolerance and occupational therapy sessions to assist with learning ways to accomplish active daily living tasks independently. The short term goals initially set for this client were to be able to stand with minimal contact assist for greater than three minute and to ambulate a distance greater than twenty feet at a time. During therapy sessions, one must continuously monitor SPO2% and heart rate due to periods of atrial fibrillation. During one session the preset goal for the day was to stand with minimal assistance for a period greater than two minutes. Through the monitoring of her vital signs it was noted that her heart rate increased to 255 beats per minutes and her SPO2% decreased to 85%. Actions and goals for the day were then modified to include bed rest and advocating to the physician for a change in her cardiac medications to allow for greater control of atrial fibrillation. Nursing Practice Applies appropriate knowledge of major health problems to guide nursing practice Case in point: As previously stated above, this client had a rather extensive list of medical diagnoses. Possessing the appropriate medical knowledge of how these disease processes were inter-related afforded me a better understanding of how to plan and manage her care. Recognizing that an increase in her heart rate and a decrease in her SPO2 levels may be an indication that she was experiencing atrial fibrillation and may need to have her cardiac medications re-dosed to meet her needs. Demonstrates an awareness of complementary modalities and their usefulness in promoting health Case in point: A complementary intervention that I was able to introduce and educate this patient on was the usefulness of visual imagery. By teaching her to focus her thoughts on an imagine that she enjoyed, while attempting to maintain standing unassisted, she was able to progress toward her goal of standing for three minute period of time. Teaching Evaluates the efficacy of health promotion and education modalities for use in a variety of settings with diverse populations Case in point: Within the presentation I addressed several aspects of health promotion. By utilizing the idea of a working concept map I was able to provide the group, which consisted of several of my peers and a clinical advisor that had earned her degree as a nurse practitioner, the opportunity to incorporate their thoughts and rationales into the process. Things such as medications, interventions, goals, studies completed and medical diagnosis were written on different color post it notes. These post-it notes were then disturbed to the audience. Members were encouraged to place the post it under the nursing diagnosis where they thought it applied best and provide a rationale as to why they placed it there. This proved to be very enlightening and educational to hear the differences in opinions and yielded a score of 99/100 fr the overall presentation grade. Research Applies research-based knowledge from nursing as the basis for culturally sensitive practice Case in point: The client presented within this assignment fell within multiple different cultures, the first of which was those of people who were morbidly obese. She was very aware of society’s views and admitted that she felt embarrassed and shameful in regards to the amount of weight that she had gained since being diagnosed with myasthenia gravis. She openly confessed that once she learned that a side-effect of prednisone was extreme weight gain, she used it as an excuse to eat comfort foods. The morbid obesity was a contributing factor to a great deal of her physical limitations. Another culture this client falls within would be that of the member who feels powerless. This client expressed on multiple occasions the difficulties that she faced with accepting help from others and the frustrations related to not having the physical ability to care for herself. She would often become tearful and apologetic for having to ask for assistance with what she termed “the simplest of tasks”. This client had also been diagnosed with obsessive compulsive disorder, chronic anxiety, depression and an extensive history of falls. The nursing research article applied to this presentation was titled “Nurses’ response time to call lights and fall occurrences”. Within the study it discusses an exploratory study that was conducted to prove that nurses will respond quicker to a patient that has a history of falls then to one who does not. The fall that occurred while in the facility was reportedly due to the call bell being out of reach – she relates that as she was reaching for it, she fell out of the bed and it took an extended amount of time for any of the nurses to acknowledge the bell after she rang it several times from the floor. This was the first incidence of a fall within the facility even though she had a documented history of prior to being admitted to rehabilitation. This incident contributed to the patient’s fears and insecurities relating to feeling helpless as well as not wanting to attempt other aspects of therapy due to complaints of increased back and knee pain. We as nurses may not have control over intrinsic factors such as mental status or reduced vision or unsteady gait, yet we do have some control over the extrinsic factors such as physical environment or responding to a call bell in a timely manner.