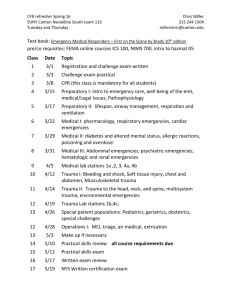
Trauma - Austin Community College
advertisement

TRAUMA Leigh Anne Wilmot RN, CEN, CLNC Lecture Adapted from Nancy Jenkins & Charlene Morris Types of Trauma Minor traumaCauses injury to a single part or system Treated in practitioners office, hospital, or ER Major or Multiple traumaSerious single system or multiple system trauma Immediate intervention with focus on survival Most often result of MVC Often require long periods of ICU Types of Trauma Blunt trauma MVC, falls, assaults and sports Can affect head, spinal cord, thorax, and abdomen Penetrating trauma Result of foreign objects set in motion Can affect internal organs Intestines, liver, spleen, and vascular system Ex: Gun shot wounds, shrapnel Other types of trauma Inhalation, thermal, & blast force Forensics Trauma victims are often victims and/or perpetrators of crime as well. Maintain the chain of evidence Work collaboratively with the Police Department Assessment of Trauma Victims Start with the ABCs: PRIMARY Survey A- airway obstruction- blood, teeth, tongue, or vomiting B-breathing-look for pneumothorax and tension pneumothorax C- circulation-look for signs of hemorrhage(external and internal) and hypovolemic shock Chest trauma-bleeding into pleural space Abdominal trauma-bleeding into abd. cavity Pelvic fracture-bleed into retroperitoneal space C – Cervical Spine Assessment of Trauma Victims Head to Toe ( SECONDARY Survey) Remember to Start with “D” for Disability Integumentary contusions, abrasions, punctures, lacerations. Consider risk for infection Abdominal-high risk for hemorrhage and peritonitis Bowel ischemia and infarction Rupture of large bowel-peritonitis Lacerate or compress solid organs – liver, spleen, pancreas Displacement of organs Assessment of Trauma Victims Musculoskeletal High priority if threatens life or limb Dislocated hip Pulseless extremity Significant blood loss from pelvic fracture Neurological Psychological- head and spinal cord injuries sudden death or serious injury Pre-hospital Care Injury identification-rapid assessment at scene Penetrating injuries to abdomen, pelvis, chest, neck or head Spinal cord with deficit Crushing injury to head, chest or abdomen Major burns Critical interventions providing life support, immobilizing the cervical spine, managing the airway, and treating hemorrhage and shock Rapid transport-ASAP to regional trauma center Triage Tag MIEMSS A V P U A V P U A V P U Patient Information Triage Status Tourniquet @ _______ Chief Complaint Extremity Splint Gauge Transportation Peel - off Bar Codes Transport Record Vital Signs History Treatment PASG Inflated at _______________ Gross Decon. Final Decon. TRIAGE TAG HOSP NOTIFIED Maryland Emergency Medical Services Maryland Department of Transportation Triage Status Section Universal color coding system Space provided for four individual evaluations Initial assessment - apply tag for priority assignment Secondary reassessment (in treatment area) Blank - can be used in the treatment area or during transportation Hospital Chief Complaint Section Major obvious injuries or illness can be circled Indicate injuries on the human figure Additional information is added on the comments line Emergency Room Paramedics communicate with ED Brief report about client with ETA Severity of condition determines ED response Champion Revised Trauma Scoring System Diagnostic Tests Blood type and cross Blood alcohol level Urine drug screen Pregnancy test What others can you think of? Diagnostic Tests cont. X-Ray, CT, MRI Diagnostic Peritoneal Lavage (DPL) Abdominal Ultrasound Focused Assessment with Sonography for Trauma (FAST) Medications 1. 2. Blood, crystalloids, (volume expanders) Inotropic drugs after IV fluids Dopamine, dobutamine, isoproterenol Increase myocardial contraction 3. Vasopressors dopamine, epinephrine 4. 5. Opioids - pain control Tetanus prophylaxis 1. 2. Toxoid Human toxin-antitoxin (TAT) Nursing Diagnosis Ineffective airway clearance Assess airway O2 sats – pulse oximeter = or > 92% LOC Risk for infection Impaired physical mobility Spiritual distress Risk for post-trauma syndrome Emotions range from fear, anger denial and shock. May experience flashbacks and nightmares Nursing Diagnosis Risk for post-trauma syndrome Emotions range from fear, anger denial and shock. May experience flashbacks and nightmares Disaster Management Natural Disasters/Severe Weather Chemical Emergencies Radiation Emergencies Bioterrorism Mass Casualties http://www.bt.cdc.gov/ Natural Disasters/Severe Weather Types: Geological Hydrological Climactic Fire Health & disease Space What events can you think of that have happened recently? Chemical Emergencies Release of a hazardous chemical that has the potential for harm Biotoxins Blood agents Pulmonary agents Nerve agents Treatment depends on chemical, some have no treatment Radiation Emergencies Can be incurred from handling of or exposure to radioactive materials Radiological technicians Weapons of Mass Destructions What do you think the S/Sx of radiation sickness are? Bioterrorism Mass Casualties What examples can you think of? What are the injuries you would expect to see, and why do they occur? Nursing Care in a Crisis Situation Assessments ABCs Skin Pain GCS Nursing Therapeutics First Secondary Mental Status Principles of Fluid Therapy aid concepts & pain management Initial wound care, fracture care Stabilization of patients SCI Shock Blast injuries Chemical exposures ARC Guidelines for Disaster Nursing Assessment and triage of patient’s condition for priority care Provision of care, treatment, and health protection Appropriate utilization of nursing service personnel Detecting changes in the event environment and organizing activities to modify or eliminate health hazards Dealing with mass casualties should it become necessary. http://www.redcross.org/services/nursing http://www.cdc.gov/masstrauma/guides