History, Assumptions, and Overview of CBT

Theory and Practice of
Cognitive Behavioral Therapy
Shona N. Vas, Ph.D
.
Department of Psychiatry & Behavioral
Neuroscience
Cognitive-Behavior Therapy Program
MS-3 Clerkship 2008-2009
Outline
What is Cognitive Behavior Therapy (CBT)?
What are the basic principles of treatment?
What is the course of treatment?
What are some examples of interventions?
Who is appropriate for CBT?
What is CBT?
Set of ‘talk’ psychotherapies that treat psychiatric conditions.
Short-term focused treatment.
Strong empirical support with randomized clinical trials.
As effective as psychiatric medications.
Recommended as critical component of treatment, particularly when medications are contraindicated or ineffective .
Why So Popular?
Clear treatment approach for patients
Assumptions make sense to patients
Based on patient’s experience
Encourages practice and compliance
Patients have a sense of control
CBT works!
Definition of Cognitive Therapy
CT is a focused form of psychotherapy based on a model stipulating that psychiatric disorders involve dysfunctional thinking.
Dysfunctional/distorted thinking arises from both biological and psychological influences
Individuals’ emotional, behavioral, and physiological reactions are influenced by the way they structure their environment.
J. Beck, 1995
Definition of CT (continued…)
Modifying dysfunctional thinking and behavior leads to improvement in symptoms.
Modifying dysfunctional beliefs which underlie dysfunctional thinking leads to more durable improvement
Definition of CT (continued…)
Cognitive therapy is defined by a cognitive formulation of the disorder and a cognitive conceptualization of the particular patient.
Cognitive therapy is not defined by the use of exclusively cognitive techniques. Techniques from many modalities are used.
CT also often referred to as Cognitive-Behavior
Therapy (CBT).
Rationale for CBT
Negative emotions are elicited by cognitive processes developed through influences of learning and temperament.
Adverse life events elicit automatic processing, which is viewed as the causal factor.
Cognitive triad: Negative automatic thoughts center around our understanding of:
– Ourselves
– Others (the world)
– Future
Focus on examination of cognitive beliefs and developing rational responses to negative automatic thoughts.
Beck et al., 1979
Cognitive Specificity Hypothesis
Distorted appraisals follow themes relevant to the specific psychiatric condition.
Psychological disorders are characterized by a different psychological profile.
– Depression: Negative view of self, others, and future. Core beliefs associated with helplessness, failure, incompetence, and unlovability.
– Anxiety: Overestimation of physical and psychological threats. Core beliefs linked with risk, dangerousness, and uncontrollability.
Cognitive Specificity
Negative Triad Associated with Depression
– Self “I am incompetent/unlovable”
– Others “People do not care about me”
– Future “The future is bleak”
Negative Triad Associated with Anxiety
– Self “I am unable to protect myself”
– Others “People will humiliate me”
– Future “It’s a matter of time before I am embarrassed”
Targeted Cognitions for Different
Disorders
OCD: appraisals of obsessive cognitions
Anorexia: control, worth, perfection
Panic: catastrophic misinterpretation of physical sensations
Paranoia: trust, vulnerability
Working Model of CBT
Event
Maladaptive
Behavior
Behavioral
Inclination
Appraisal
Affective and
Biological Arousal
Thase et al., 1998
Cognitive Model
Triggering Event
Bill goes to collection
Behavior
Avoidance; withdrawal
Appraisal
“I can never do anything right…”
Behavioral Inclination
“I don’t want to deal with it”
“It’s too stressful to think about it”
Bodily Sensations
Low energy, disruption of sleep, increased fatigue
Thase et al., 1998
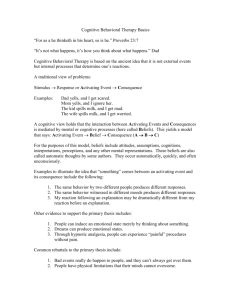
What are Automatic Thoughts?
What was going through your mind?
Happen spontaneously in response to situation
Occur in shorthand: words or images
Do not arise from reasoning
No logical sequence
Hard to turn off
May be hard to articulate
Stressful
Situation
Automatic Thoughts
Negative
Emotions
Cognitive Distortions
Patients tend to make consistent errors in their thinking
Often, there is a systematic negative bias in the cognitive processing of patients suffering from psychiatric disorders
Help patient identify the cognitive errors s/he is most likely to make
Types of Cognitive Distortions
– Emotional reasoning Feelings are facts
– Anticipating negative outcomes The worst will happen
– All-or-nothing thinking
– Mind-reading
All good or all bad
Knowing what others are thinking
– Personalization
– Mental filter
Excess responsibility
Ignoring the positive
Examples
Cognitive Distortions
– Emotional Reasoning: “I feel incompetent, so I know I’ll fail”
– Catastrophizing: “It is going to be terrible”
– Personalization: “It’s always my fault”
– Black or white thinking: “If it isn’t perfect, it’s no good at all.”
Core Beliefs
Core beliefs underlie and produce automatic thoughts.
These assumptions influence information processing and organize understanding about ourselves, others, and the future.
These core beliefs remain dormant until activated by stress or negative life events.
Categories of core beliefs (helpless, worthless, unlovable)
Core Beliefs Automatic Thoughts
Examples of Core Beliefs
Helpless core beliefs
– I am inadequate, ineffective, incompetent, can’t cope
– I am powerless, out of control, trapped
– I am vulnerable, weak, needy, a victim, likely to be hurt
– I am inferior, a failure, a loser, defective, not good enough, don’t measure up
Unlovable core beliefs
– I am unlikable, unwanted, will be rejected or abandoned, always be alone
– I am undesirable, ugly, unattractive, boring, have nothing to offer
– I am different, flawed, defective, not good enough to be loved by others
Worthless core beliefs
– I am worthless, unacceptable, bad, crazy, broken, nothing, a waste
– I am hurtful, dangerous, toxic, evil
– I don’t deserve to live
Cognitive Conceptualization
Physiology
Current
Situation
Automatic Thoughts
About self, world
And others
Feelings
Behavior
Childhood
And Early
Life Events
Underlying Assumptions and Core Beliefs
Compensatory
Strategies
Example 1
Situation
Partner says:
“I need time to be with my friends”
Automatic Thoughts
Automatic response:
“Oh no, he’s losing interest and is going to break up with me….”
Physiology
Heart racing
Lump in throat
Feelings
Sadness
Worry
Anger
Behavior
Seek reassurance
Withdraw
Cry
Childhood
Experiences
Parental neglect and criticism
Underlying Assumptions &
Core Beliefs
“I’m flawed in numerous ways, which means I’m not worthy of consistent attention and care.
People only care when they want something.”
Compensatory
Strategies
Be independent and you’ll be safe.
Watch out – people are careless with you.
Situation
Disappointing exam result
Childhood
Adversities
Parental standards reinforce academic achievement
Example 2
Automatic Thoughts
“I am not going to get through this program -
I’m not as smart as everyone else.
People will discover this and I will be humiliated.”
Physiology
Pit in stomach
Dry mouth
Feelings
Worry, shame,
Disappointment
Humiliation.
Behavior
Use alcohol,
Procrastinate with homework
Underlying Assumptions
“If I don’t excel in school, I’m a total failure”
Compensatory
Strategies
Work extra hard to offset incompetence.
Responding to Negative Thoughts
Define Situation
Clarify meaning of cognitive appraisal
– What was going through your mind just then?
– What did the situation mean for you?
Evaluate interpretation
– Evidence: For and against this belief?
– Alternatives: Any other explanation(s)?
– Implications: So what….?
Evaluating Negative Thoughts
What is the effect of telling myself this thought?
What could be the effect of changing my thinking?
What would I tell ___ (a friend/family member) if s/he viewed this situation in this way?
What can I do now?
Sample Thought Log
Situation
Going on vacation—Ask a colleague to do some work for me
Thoughts
She’ll say no…
I’m not doing a good job
The boss thinks I take too much time off
Emotions Rational
Response
Anxiety
(70%)
Guilt (40%)
Sadness
(20%)
I haven’t taken a day off in 6 months. We work as a team, so it’s also her job to track the samples.
Outcome
Anxiety (10%)
Guilt (0%)
Relief (40%)
Cognitive
Distortions:
All/nothing
Mindreading
Fortune-
Telling
Overgeneralization
Common Components of CBT
Establish good therapeutic relationship
Educate patients - model, disorder, therapy
Assess illness objectively, set goals
Use evidence to guide treatment decisions
Structure treatment sessions with agenda
Limit treatment length
Issue and review homework to generalize learning
3.
4.
1.
2.
7.
8.
5.
6.
Course of Treatment
Assessment
Provide rationale
Training in self-monitoring
Behavioral strategies
1.
Monitor relationship between situation/action and mood.
2.
Applying new coping strategies to larger issues.
Identifying beliefs and biases
Evaluating and changing beliefs
Core beliefs and assumptions
Relapse prevention and termination
Basic Principles
Change mood states by using cognitive and behavioral strategies:
– Identifying/modifying automatic thoughts & core beliefs,
– Regulating routine, and
– Minimizing avoidance.
Emphasis on ‘here and now’
Preference for concrete examples
– Start with specific situation (complete thought log)
Reliance on Socratic questioning
– Ask open-ended questions
Empirical approach to test beliefs
– Challenge thoughts not based on evidence
– Cognitive restructuring
Promote rapid symptom change
Behavioral Interventions
Breathing retraining
Relaxation
Behavioral activation
Interpersonal effectiveness training
Problem-solving skills
Exposure and response prevention
Social skills training
Graded task assignment
Cognitive Interventions
Monitor automatic thoughts
Teach imagery techniques
Promote cognitive restructuring
Examine alternative evidence
Modify core beliefs
Generate rational alternatives
Efficacy
Cognitive and behavioral approaches are effective
Supported by over 325 controlled outcome studies
State-of-the-art therapy, manualized
Applications of CBT
Mood Disorders
– Unipolar Depression (1979)
– Bipolar Disorder (1996)
– Dysthymia and Chronic MDD (2000)
Anxiety Disorders
– GAD (1985)
– Social Phobia (1985)
– Panic Disorder (1986)
– OCD (1988)
– PTSD (1991)
Emotional Disorders (2006)
Applications of CBT
(Continued…)
Eating Disorders (1981)
Marital Problems
Behavioral Medicine
– Headaches (1985)
– Insomnia (1987)
– Chronic Pain (1988)
– Smoking Cessation
– Hypochondriasis
– Body Dysmorphic Disorder
Controlled Outcome Studies on
CBT
Unipolar Depression
(~30)
Eating Disorders
– Anorexia (~5)
– Bulimia (~15)
Generalized Anxiety
Disorder (~12)
Social Phobia (~14)
Panic Disorder (~10)
Borderline P.D. (2)
Schizophrenia (~45)
C/A Depression (8)
Chronic Depression (1)
Conclusions
System of psychotherapies
Unified theory of psychopathology
Short-term treatment
Objective assessment and monitoring
Strong empirical support
As effective as pharmacotherapy
Questions? Comments?
Dr. Shona Vas
(773) 702-1517
Psychiatry Department Office: A-312 svas@yoda.bsd.uchicago.edu