Facial Emergencies
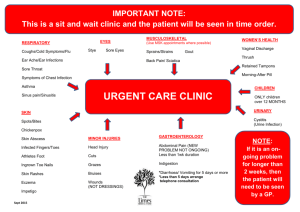
advertisement

Facial Emergencies General Strategy 1. Primary/ Secondary Assessment 2. Focused Assessment A. Subjective- HPI (pain, resp distress/ sensory changes) auditory- ear pain, hearing loss, ringing in ears visual- decreased tearing, blindness, visual field deficits tactile- dec sensation, facial pain gustatory- impairment of taste, loss of taste olfactory- loss of smell * facial asymmetry, rash, fever/chills, n/v, speech prob B. PMH B. Objective datageneral- LOC< VS, odors, hygiene, LOD inspection- drooling, symmetry, pupil reaction, vesicles palpation- sensory deficits, area of tenderness percussion- soft tissue over sinuses. 3. DiagnosticA. labs- cultures, CBC< coag profile, ABG B. Imaging- Facial bones, water’s view, Panorex, CXR, CT head 4. Planning/Intervention- priorities of care 5. Evaluation Pediatric considerations PEDIATRIC- 85% of foreign body aspirations occur in children <3. - Boys 2x > girls to aspirate. Peak incidence between 1-2 y/o. Foreign body ingestions = in boys & girls. - 20-38% children w/ esophageal FB ingestions have no symptoms. - irritability and lack of feeding ** potential sign of dental/ENT emergencies Pediatric “Pearls” Persistent cough/wheezing may indicate FB aspiration Difficulty feeding may indicate significant ENT emergency Abrupt onset upper respiratory and pulmonary symptoms suggest FB ingestion Geriatric considerations Aging related * Visual loss, hearing loss, decreased taste and sensitivity to touch. * Loss of STM, slower thought processing, incr pain threshold * muscle atrophy, decreased flexibility Elderly pt have chronic diseases that provide more limitations Geriatric “pearls” Malignant external otitis media and cholesteatoma is consideration for elderly patients c/o earache or recurrent ear infections. (especially those w/ DM) Falls, visual changes, MVC’s and assaults are the primary causes of dental/ENT trauma in the elderly Poor eyesight contributes to FB in the pharynx. Bell’s Palsy Bell’s Palsy One of the most common presentations of facial nerve paralysis syndrome Paralysis of all the facial muscles on one side of face, including forehead Usually preceded by URI (60%) or other viral illness Bell’s palsy is diagnosis of exclusion Symptoms thought to be caused by swelling of facial nerve, in narrow course through temporal bone, nerve becomes compressed and ischemic. Usually unilateral Usually in people >40 years old, and is self-limiting Herpes Zoster Oticis (Ramsay Hunt Syndrome) Viral infection involving external, middle, and inner ear and associated with unilateral facial paralysis. Herpetiform vesicular eruptions occur due to being a reactivation of varicella-zoster virus on the dermatome The eruptions are on the external ear, TM, soft palate, oral cavity, face, neck, and/or shoulder More painful than Bell’s palsy. Less incidence of full facial recovery & possibility of permanent hearing loss Assessment SubjectiveHPI- viral illness, paralysis, pain, drooling, loss of taste, n/v, sensitivity to noise PMH- DM, sarcoidosis, Lyme disease, VZV infection Objectivegeneral- LOC, drooling, LOD inspection- upward mvmt of eye on affected side when trying to close eye, facial paralysis, lid lag, dec lacrimation, drooping of mouth, no blink on affected side, vesicular lesions Diagnostic- lyme titer, mastoid xray, CT scan, Nursing DiagnosesPlanning/Intervention Meds- analgesics, steroids, antivirals, Educate- moist heat/facial massage, corneal protection, sunglasses, reassurance Evaluation- Sinusitis Inflammatory condition of mucus membranes lining the paranasal sinuses. Symptoms mild-severe, progresses over 7-10 days Bacterial disease suggested if worsening after 5 days, persistent symptoms after 10 days. Symptoms- nasal congestion, mucopurulent drainage, pressure over sinuses, malaise,, fever, facial swelling Complications- chronic sinusitis meningitis, orbital cellulitis, epidural abscess, orbtal abscess. Trigeminal Neuralgia Disorder of 5th cranial nerve Chief complaint- excruciatingly painful paroxysms. More common in women, usually 50-69 Exacerbated by exposure to cold and facial stimulus Parotitis Inflammation of parotid gland Usually caused by bacteria or virus, but can be caused by HIV,TB, and calculi formation Fractured tooth Most frequent dental emergency in ED. Can result from sports activity, MVC, falls, seizures, physical assault. Consider- 50% of physical trauma in child abuse is in head/neck region Assess for concurrent head injury. Watch for aspiration of tooth Classifications of tooth fractures Class I- most common, involving only enamel. Injured area is chalky white. Cosmetic restoration available w/i 24-48 hrs. Class II- pass through the enamel and expose dentin. Fracture appears ivory/yellow. Urgent for children b/c of lack of protective dentin and RF for bacteria to easily get in pulp causing infection or abscess if exposed >6hrs. Adults treated w/I 24 hrs. Class III- dental emergency. Injury to enamel, dentin, and pulp cause pink/bloody tinge to fracture. Exposure of pulp, exposes nerve. Tooth avulsion Dental emergency- if tooth torn from socket, tissue hypoxia develops, followed by eventual necrosis of pulp. Re-implantation w/I 30 min increases chance for reimplantation & healing. Tooth should be transported In milk, saline, or under pts tongue in cooperative pt. Ludwig’s angina Usually results from secondary dental infection involving the lower second & 3rd molars and can lead to airway mgmt problems. Bilateral diffuse swelling & extending cellulitis involving (Submandibular, submental, & sublingual) Neck & face swollen with protrusion and elevation of tongue, causes difficulty talking & swallowing. THE EAR The ear consists of 3 parts external- consists of auricle and external canal middle- air filled cavity inside temporal bone, contains tympanic membrane inner- contains bony labyrinth, holds sensory organs for equilibrium Foreign Object in the ear The object may have entered external canal accidentally or intentionally. Often in children it is not discovered until purulent drainage noted. Small insects that enter canal produce great discomfort due to mvmt & buzzing. Vegetable foreign bodies absorb moisture, result in enlargement, increased obstruction of ear canal, and offensive odor. Ear infections- definitions Acute Otitis Externa * “swimmer’s ear” * bacterial or fungal infection * RF- moisture in ear canal from retained H2O, or trauma resulting from Q tip or foreign object in ear Acute Otitis Media * bacterial or viral infection of middle ear *commonly preceded by URI. * more common in children due to narrower, shorter eustachian tubes. Acute Otitis Externa S/S- painful outer ear and canal, itchy ear, impaired or diminshed hearing, feeling of fullness in ear, discharge of ear canal, fever. HALLMARK SIGN- reproducible pain when earlobe manipulated interventions/ Monitoring- usually no systemic abx unless pt DM, usually abx ear gtts. Apply hot, moist compresses to external ear. Avoid swimming 7-10 days until cleared. Ear plugs should be encouraged. Epistaxis- assessment HPI- duration, frequency, amt of bleeding. Constant oozing ( anterior), posterior (more profuse, possible arterial hemorrhage), possible FB, trauma. PMH- HTN, artherosclerosis, bleeding disorders Physical assessment- LOC< BP, tachycardia, fear of dying. Inspect- bleeding, erythema and swelling or nasal mucosa, Blood in auditory canals. Diagnostic- CBC, coags, T&C, CT is tumor suspected Treatments Anterior bleeds- sitting position, leaning forward. Direct pressure. Posterior bleeds- direct pressure for at least 10 minutes, high fowler’s position, IV, ENT consult, assist with cauterization, monitor VS. Evaluation- bleeding, VS. Peritonsillar abscess s/s- severe sore throat, painful/difficult swallowing, trismus, and uvular deviation, muffled voice and unable to swallow own saliva usually Streptococci bacteria invades tonsillar capsule and areaolar tissue. Treatment- ABC’s, O2, IV, HOB 60-90 degrees provide warm saline throat irrigations prepare for I & D Meds (abx, topical anesthetics, analgesics, narcotics, antipyretics) Evaluation- airway, pain relief Epiglottitis Infection and inflammation involving epiglottitis. Frequently caused by HIB. Predominately child illness btwn 2-7 yrs old, decreased dramatically since Hib vaccine initiated. Abrupt onset fever and sore throat.