Prostate Cancer
advertisement

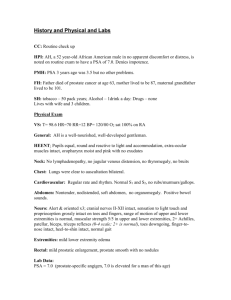
Carcinoma of the Prostate Prevention, Screening, Diagnosis, and Treatment Roland T. Skeel, M.D. Conflict of Interest Disclosure Neither I nor my immediate family members have any Financial Interests or Significant Relationships that might affect – or reasonably appear to affect – this presentation on “Prostate Cancer” Objectives List risk factors for prostate cancer, and discuss relative strength Discuss potential prevention strategies Discuss benefits and risks of prostate cancer screening, including expected survival rates Counsel patients about primary treatment options for local disease Recommend systemic therapy for advanced cancer. Carcinoma of Prostate Most common cancer in United States with exception of skin cancer Increases in new cases by 50% between 1980 and 1990 New cases in 2009 – 192,280 (Est.), 80 % early disease Deaths – 27,360 (Est.) Increasing number of “non-lethal” tumors being diagnosed 1 in 6 will be diagnosed, 1 in 35 will die from it. (10% of cancer related deaths in men.) Survival Rates – Prostate Cancer 5-year relative survival rate nearly 100% 10-year relative survival rate is 91% 15 year relative survival rate is 76% Risk Factors for Prostate Cancer Age – Rare before 40; 65% over the age of 65 Race - More common in African-American men; more likely diagnosed at advanced stage; 2x more likely to die of the disease; less common in Asian-American and Hispanic-American men than non-Hispanic whites. Family History - 1st degree relatives, father, brother Nationality - North America and NW Europe vs Asia, Africa, Central and South America Genetics – BRCA1 and BRCA2 increase risk, but account for very small percentage of prostate cancer Obesity, Diet, Exercise, prostatitis, STDs, Vasectomy – not much effect, BUT……. Risk Factors for Prostate Cancer Claimed by some studies Diet Red meat, high fat dairy products Fruits, vegetables, grains Exercise and maintaining healthy weight may decrease the risk Finasteride Chemoprevention for Prostate Cancer Finasteride = 5-alpha reductase inhibitor, blocks intracellular conversion of testosterone to dihydrotestosterone Based on solid evidence, chemoprevention with finasteride reduces the incidence of prostate cancer (6% absolute; 25% relative risk reduction), but the evidence is inadequate to determine whether chemoprevention with finasteride reduces mortality from prostate cancer. Harms: erectile dysfunction, loss of libido, gynecomastia, higher grade cancers. Thompson IM, Goodman PJ, Tangen CM, et al.: The influence of finasteride on the development of prostate cancer. N Engl J Med 349 (3): 215-24, 2003 Chemoprevention - Other The Selenium and Vitamin E cancer Prevention Trial was a large randomized placebo-controlled trial of Vitamin E and selenium, alone or in combination. It failed to demonstrate that these drugs reduce prostate cancer in relatively healthy men. Lippman SM, Klein EA, Goodman PJ, et al.: Effect of selenium and vitamin E on risk of prostate cancer and other cancers: the Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 301 (1): 39-51, 2009 Early detection and screening Digital rectal exam – Feel for nodules PSA – How high? Transrectal ultrasound – not for screening First two tests are convenient and inexpensive, but consequences may not be ACS, AUA, ACR, NCI Screening Recommendations No major scientific or medical organizations, including the American Cancer Society (ACS), American Urological Association (AUA), US Preventive Services Task Force (USPSTF), American College of Physicians (ACP), National Cancer Institute (NCI), American Academy of Family Physicians (AAFP), and American College of Preventive Medicine (ACPM) support routine testing for prostate cancer at this time. In 2008 the USPSTF concluded that the risks of screening for prostate cancer outweigh the benefits for men age 75 years or older. The ACS and AUA recommend that health care professionals offer the option of testing for early detection of prostate cancer to all men who are at least 50 years old (or younger if at higher risk). PSA and Prostate Cancer Risk When prostate cancer develops, the PSA level usually goes above 4. Still, a level below 4 does not mean that cancer isn't present -- about 15% of men with a PSA below 4 will have prostate cancer on biopsy. Men with a PSA level in the borderline range between 4 and 10, have about a 1 in 4 chance of having prostate cancer. If the PSA is more than 10, the chance of having prostate cancer is over 50% Confounding Factors for PSA Increase BPH Age Prostatitis Ejaculation Decrease Finasteride, dutasteride Some herbal mixtures Obesity Under investigation: PSA Density, PSA Velocity, % free PSA PSA Density - Normalized to prostate volume PSA Velocity - Change in PSA over time (e.g., more than 15% per year) Free PSA/Total PSA - lower ratio suggests cancer, since more free PSA from normal prostate is degradated (< 10% - biopsy) Presenting Symptoms of Prostate Cancer Decreased urinary stream Urinary frequency Hematuria Bone pain LE numbness or weakness Badder/bowel incontinence Prostate Cancer: Remarkably Common With Many Unanswered Questions Understood: • Natural history • Prevalence • Patterns of spread Questions: • Universal use of screening tests • Choices of therapy • Contributing factors ??? Sources: Nelson WG, DeMarzo AM, Isaacs WB. Prostate cancer. NEJM. 2003;349:366-381. Aging and Prostate Cancer • As men age, prostate cells are increasingly likely to turn cancerous • Autopsies reveal: - Age 30-40: 29% prevalence - Age 60-70: 64% prevalence Bad News: American male has a 16.7% risk of being diagnosed with prostate cancer Good News: In most cases, the cancer cells are slow growing and occur late in life – only 3.5% of U.S males die from prostate cancer Sources: Nelson WG, DeMarzo AM, Isaacs WB. Prostate cancer. NEJM. 2003;349:366-381. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level ≤4.0 ng per milliliter. NEJM. 2004;350:2239-2245. Why Has Diagnostic Progress Not Resulted In Greater Long-Term Survival Rates? Death rate is comparatively low considering prevalence • Lifetime risk of diagnosis: 1 in 6 • Lifetime risk of death: 1 in 33 • 5-year survival rate: 98% Diagnostic and therapeutic advances have improved quality of life, but not necessarily the years of life • Risk is tied to age - All ages: 17.7 cases per 100,000 - Age 75 to 84: 248 cases per 100,000 - Over 85: 591 cases per 100,000 Prostate cancer cells are generally less aggressive with increasing age, suggesting “many prostate cancers detected in routine practice may be clinically unimportant” Sources: Mayo Clinic.com. Prostate Cancer Guide. Available at: http://www.mayoclinic.com/health/prostate-cancer/PC99999. Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level ≤4.0 ng per milliliter. NEJM. 2004;350:2239-2245. Use of PSA Testing is a Double-Edged Sword Illustrates challenges of using imperfect markers/surrogates to indicate disease. “Although the use of PSA testing in the United States has led to earlier diagnosis and a marked shift in the stage at which prostate cancer is identified, it is unclear whether PSA testing reduces the rate of death from prostate cancer.” – Clinical experts Unresolved dilemma: Over-treating clinically unimportant disease revealed by PSA testing vs. Under-treating clinically important disease that goes undetected without extensive use of PSA testing Sources: Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, et al. Prevalence of prostate cancer among men with a prostate-specific antigen level ≤4.0 ng per milliliter. NEJM. 2004;350:2239-2245. PSA Levels and Their Predictive Value for Diagnosis Other conditions besides prostate cancer can increase PSA levels • infection • inflammation • benign growths 2004 Study of men: PSA never above 4ng/ml; no abnormal rectal exam Percent with prostate cancer 26% 24% 17% 10% 7% PSA level (ng/ml) 3.1 to 4.0 2.1 to 3.0 1.1 to 2.0 .6 to 1.0 less than .5 In those with cancer and low PSA levels, 12.5% had aggressive, rapidly multiplying high-grade tumors likely to spread. Sources: Cooner WH, Mosley BR, Rutherford CL Dr. et al. Prostate cancer detection in a clinical urological practice by ultrasonography, digital rectal examination and prostate specific antigen. J Urol. 1990;143:1146-52. Cited in Thompson IM, Pauler DK, Goodman PJ, Tangen CM, Lucia MS, et al. Krumholtz JS, Carvalhal GF, Ramos CG, et al. Prostate-specific antigen cutoff of 2.6 ng/mL for prostate cancer screening is associated with favorable pathologic tumor features. Urology. 2002;60:469-473. Economics of Treating and Screening For the Disease Cost of treating prostate cancer in California – $360 million per year Cost of universal screening (as previously recommended by ACS) – approximately $12.7 billion per year Savings from increased diagnosis at earlier stages, minus increased costs from pursuing false positives or occasional high-grade tumors with false negative PSAs remains to be explored. Against PSA Screening (all men 50+) American Urological Association American Cancer Society National Cancer Institute U.S. Preventive Services Taskforce Sources: Max W, et al. The economic burden of prostate cancer in California. Cancer. June 2002;94:2906-13. What Can We Learn? 1. Markers are imperfect predictors requiring a strong understanding of the upsides and downsides when used 2. Prevention requires screening — screening often relies on markers 3. Answer is not to throw away markers, but learn from and improve them Effect of Early Diagnosis Unknown: In areas where there is aggressive screening, the incidence in higher than where there is not; the death rate from prostate cancer is similar Randomized trials to test screening underway Conclusion: Do not screen over age 70, or if life expectancy < 10 years Do not screen under age 60, unless strong family history Recognize limitations age 60-70 Prostate Cancer Survival Related to Stage Grade Extent of tumor at diagnosis Local disease - Median Survival > 5 years Metastatic disease Median Survival 1-3 years, but individuals may survive 10 or more years Establishing a Diagnosis of Prostate Cancer DRE PSA/PSA velocity/percent-free PSA Transrectal U/S U/S- guided biopsy Evaluation of Abnormal PSA or Prostate Mass Ultrasound guided needle biopsies (6-12) If positive, Gleeson score (2 predominant histologies). Range - 2 (1+1) to 10 (5+5) 2-4 - Best 5,6 - Intermediate 7-10 - Worse PSA < 10, rarely have detectable metastatic disease What Does the Grade of the Tumor Mean? Grade of a tumor is predictive of its likelihood to spread beyond confines of the prostate, affecting curability. 12% of low-grade tumors (2-4) spread beyond prostate in 10 years 33% of medium-grade tumors (5,6) spread beyond prostate in10 years 61% of high-grade tumors (7-10) spread beyond prostate in 10 years Sources: Mayo Clinic.com. Prostate Cancer Guide. Available at: http://www.mayoclinic.com/health/prostate-cancer/PC99999. Prostate Cancer in California. Ed. Mill PK. Public Health Institute. 2000. Staging and Prognostic Factors TNM staging system Prognostic Factors Gleason grading DNA analysis by flow cytometry PSA level Predictive models for organ-confined versus non-organ confined disease Staging Prostate Cancer Abdominal and pelvic CT scans Chest x-ray Bone scan LFT’s Serum PSA and acid phosphatase Staging Prostate Cancer Stage I - T1a and grade 1 (Incidental, early) Stage II T1a and Grade 2-4; T1b,c (By biopsy only) T2 (Confined to Prostate) Stage III - T3 (Through prostate capsule) Stage IV - T4 (Invades adjacent structures), N1-3, M1 Recurrence Risk for Clinically Localized Prostate Cancer Low Risk: T1-T2a and Gleason score 2-6 and ng/ml PSA < 10 Intermediate Risk: T2b-T2c or Gleason score 7 or PSA 10-20 High Risk: T3a or Gleason score 8-10 or PSA > 20 Very High Risk: T3b-T4(locally advanced) Treatment Decisions for Clinically Localized Prostate Cancer Based on recurrence risk (Low, intermediate, or high) and Life expectancy (<10 years vs > 10 years). Prostate - Goals of Therapy Primary Therapy T1a - Except in very young (< 60), follow with no therapy T1b, T1c, T2 - radical prostatectomy or high dose radiation therapy. (May also observe if low-grade) T3 (Stage III) - Usually treated with radiation therapy Metastatic - Treat when symptoms. In high risk disease, may add hormonal therapy Radical Retropubic Prostatectomy (RRP) “Nerve Sparing” procedure developed by Walsh consisted of modified surgical technique to control blood and enhance visibility within surgical site. Allowed for the identification and potential preservation of the nerves that control erectile function (potency). Two neurovascular bundles on either side of the prostate that control erectile function. The Da Vinci Robot Surgeon operates from a console with a 3-D screen. Grasp controls to manipulate surgical tools within the patient. Robotic arms translate finger, hand, and wrist movements. Very High-Precision http://www.intuitivesurgical.com ? Radiation Therapy (RT) High-Powered X-Rays that damage DNA and kill prostate cancer cells. 1. External Beam Radiation Therapy (EBRT): X-rays aimed at prostate. 2. Brachytherapy: Radioactive seed implants into prostate. External Beam Radiation Goal: Maximize damage to the prostate and minimize damage to surrounding tissues (i.e. bladder and rectum) Seminal Vesicles Prostate Brachytherapy: Distribution Cross-Section of Prostate Urethra Uneven Distribution Ultrasound-guided bead placement for even distribution Image of Prostate With Radioactive Bead Implants RT: Complications EBRT Most symptoms occur during treatments and subside after completion. Diarrhea, rectal irritation, fatigue, frequent and painful urination, blood in the urine. Erectile dysfunction: less common than radical prostatectomy following treatment but slower recovery. RT: Complications Brachytherapy High initial dose of radiation that slowly fades over 1 year. Prostate inflammation and swelling, sometimes with severe urinary symptoms. Other, more rare symptoms include persistent urinary and bowel frequency and urgency. Erectile dysfunction: similar to EBRT. Watchful Waiting A.K.A. observation, expectant therapy or deferred therapy. Diagnosis of an early-stage (T1-T2), lowgrade tumor. No medical treatment is provided. Patient receives regular follow-up to monitor tumor. Why Wait? PSA and DRE can detect prostate cancer at a very early stage. Average doubling time of a prostate tumor is quite slow (2-4 years). Immediate radical therapy may constitute over-treatment and an introduce unnecessary urinary and potency risks. May be appropriate if the patient is elderly and/or in poor health, and will live out their life spans without the cancer causing problems. May also be appropriate for a younger patient who is willing to be vigilant and accept the risk of the cancer spreading. Treatment of Symptomatic Metastatic Disease 1. Hormonal Therapy - initial therapy for locally advanced or metastatic disease Orchiectomy Estrogens (No longer used) LHRH analogs (+/- anti-androgens) Antiandrogens + finasteride Second line therapies consist of one of therapies not used before, e.g., anti-androgens if used only LHRH analogs Hormone Therapy Prostate cells and prostate cancer cells are dependant upon androgens (male sex hormones) for survival and growth. Removal of androgens kills a majority of prostate cancer cells. Testosterone 95% Testes Prostate Growth and Function Adrenal Androgen 5 % Adjuvant Hormone Therapy Hormone therapy (androgen ablation) is a standard method of treating advanced and metastatic prostate cancer. However, for newly-diagnosed advanced cancers, androgen ablation may be performed prior to prostatectomy or radiation in order to shrink the tumor. The effectiveness of this technique is still under debate. Removing Androgens 1. 2. 3. 4. 5. Orchiectomy (castration): surgical removal of the testicles. Oral drug which has the same effect as castration. Blocks testosterone production. Include LHRH agonists and (oral estrogens). Anti-androgens which block the effects of testosterone. (Blocks binding of DHT to androgen receptors.) 5-α reductase inhibitor (enhances intracellular androgen blockade) Combination therapies. LHRH Analogs Goserelin (Zolodex) Leuprolide (Lupron) Available as every 1, 3, or 4 month injections Castrate levels of testosterone attainable in a few weeks Antiandrogens Flutamide Bicalutamide Nilutamide Combined androgen blockade not superior to LHRH therapy alone Higher cost and more side effects than LHRH therapy alone Primary value when starting LHRH to limit the flare reaction Finasteride and bicalutamide as primary hormonal therapy in advanced adenocarcinoma of the prostate Duration of control comparable to castration, with preserved sexual function in some patients With recurrence, some patients may still respond to LHRH agonists Tay, MH et al. Annals of Oncology 15:974, 2004 Results of Androgen Removal Impotence Loss of sexual desire (libido) Hot flashes Weight gain Fatigue Reduced brain function Loss of muscle and bone mass Some cardiovascular risks Hormone-Refractory Prostate Cancer (HRPC) Despite initial response rates of 80-90%, nearly all men with advanced prostate cancer develop hormone-resistant prostate cancer after 18-36 months. These “hormone-refractory” (HR) prostate cancer cells can grow in the absence of androgens. The behavior of HR prostate cancers differ widely between patients. Treatment of Symptomatic, Hormone Refractory Metastatic Disease 1. Cytotoxic chemotherapy Docetaxel (every three weeks) and prednisone improves pain and reduces need for analgesic agents Mitoxantrone Other agents have had limited effectiveness Continue hormone therapy to prevent flare with rising testosterone levels. 2. Bisphosphonates - decreases skeletal complications Treatment of Symptomatic Metastatic Disease 3. Radiation therapy External beam radiotherapy Radioisotopes, such as Strontium 89 Evaluation of Response PSA and Acid Phosphatase are useful in selected circumstances Bone scans are difficult, because increase can be seen in healing as well as worsening Complications of Systemic Prostate Cancer Therapy All hormonal therapies can cause sexual dysfunction and decreased libido; less with finasteride and anti-androgen Orchiectomy - rarely local infection or hematoma Anti-androgen - diarrhea, hepatic dysfunction Estrogen - thromboembolic disease, fluid retention, cardiac disease Chemotherapy - nausea, vomiting, mucositis, marrow suppression, and alopecia Management of Prostate Cancer Bone Metastases Goal: prevent pain, improve mobility, prevent complications such as fractures or compression. Goal: Maintain acceptable quality of life. Methods: bis-phosphonates, radiation of detected metastatic lesions, surgery. ? Conclusions Risk factors are age, family history, race, and possibly diet and exercise Overall survival excellent (many years) Early detection can find localized cancer, but survival benefits still uncertain Treatment depends on grade, extent and location of disease Surgery and radiation are equivalent therapeutic tools for localized prostate cancer Hormonal therapy is effective for metastatic prostate cancer Hormone refractory prostate cancer responds to chemotherapy, with occasional long term improvement. History of the Prostatectomy Hugh Hampton Young (Johns Hopkins) pioneered a systematic technique and performed the first radical perineal prostatectomy in 1904. 1943 - Theodore Millin introduced the retropubic prostatectomy approach. 1983 – Patrick Walsh described a modified “nerve-sparing” retropubic approach to preserve potency. The Nerve Bundles Cross-Section of Prostate Urethra Prostate Rectum Neurovascular Bundles of Walsh RRP: The Surgical Surgical Approach 1.5-4 hours, usually epidural anesthesia. Incision: Begins just below navel and extends to pubic bone. Remaining Urethra is sewn to bladder neck over a catheter. Approach Pelvic Bone (Pubis) Bladder Rectum Urethra Prostate RRP: Complications Severe or life-threatening complications are rare. Incontinence (Urinary Control): complete incontinence is uncommon, although a significant number of patients experience some stress-incontinence. Usually improves with time. Impotence (Erectile Dysfunction): if both neurovascular bundles were spared, potency rates range from 30-86%, depending on institution. Usually improves over time, and other ED treatments can work. RRP: Advantages Whole prostate - and thus the entire tumor can be examined histologically. Surgeon has access to regional lymph nodes to test if prostate cancer cells have left the tumor. Surgical margin can be examined. T Negative Surgical Margin OR T Positive Surgical Margin Not all of tumor removed Radical Perineal Prostatectomy Very similar to Retropubic protocol Pelvic (nerve sparing, sewing Bone of urethra, etc.) Prostate Bladder (Pubis) Rectum Incision: Between Anus and base of Scrotum. Urethra Surgical Approach Perineal Prostatectomy Comparison with RRP: Comparable cure rates as well as similar urinary and potency complications. Disadvantages: Cannot access regional lymph nodes Slight increase in risk of rectal injury and associated complications. Emerging Therapy: Laparoscopic Radical Prostatectomy Eliminates the need for a large incision by using a telescopic instruments called a laparoscopes. Small camera attached to the laparoscope allows the surgeon to view inside the abdomen. Laparoscopic Prostatectomy Advantages: Less blood loss. No large incision. Shorter hospital stay and earlier return to activities. Disadvantages: Longer procedure Variable surgical margins rates. Slower return of urinary continence. Variable potency rates. General Procedure: EBRT and Brachytherapy EBRT: 1. 2. Map precise area that will receive radiation. Multiple treatments ~5 days/week for ~8 weeks. Each treatment takes about 10 minutes and no anesthesia is required. Brachytherapy 1. 2. 40-100 rice-sized radioactive seeds are implanted into the prostate via ultrasound-guided needles. Anesthesia is required. All radiation inside the pellets is generally exhausted within a year. History of Radiation Therapy 1898 – The first use of newly discovered “Xrays” was to alleviate the pain of pelvic bone metastases. Early use of external beam radiation therapy was limited because of power necessary to reach deep-seated cancers such as prostate cancer. 1950’s – New and more powerful isotopes and machines were discovered and built. Today – Computers and improved radiation technologies allow high-dose and high-precision treatment of prostate tumors. History of Brachytherapy 1909 – Minet first placed a radium tube in a catheter to irradiate prostate cancer. 1970’s – Real interest occurred when Whitmore described an implant technique using I-125. Inconsistent dose distribution was a problem. 1985 – Holm and Ragde used TransRectal UltraSound (TRUS) to position Pd-103 implants and established a national brachytherapy implant course. Cryotherapy Destroys prostate cells by freezing tissue. Old idea that is making a comeback due to greater precision and better methods of imaging and temperature monitoring. Method: insertion of sub-zero cryoprobes into prostate perineally (between scrotum and anus). As yet unresolved how effective cryotherapy is compared to surgery or radiation.