Click here to view RT Assessment
advertisement

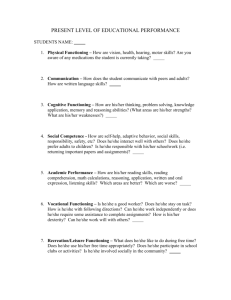
Tiffany Dean CASE STUDY WORKSHEET RT Assessment Identifying Data Client name (use alias for confidentiality) Baron Leone Age 51 y/o Gender ♂ Primary Diagnosis (* The dx/s that caused the admission of the client) LCVA in February 2008 and again in November 2009. HTN prior to strokes. Secondary Diagnoses (* Other dx/s that are still active – the person is still experiencing – that are not the primary reason for admission of the client) HTN, AFib, Gout, aphasia Past medical history (* Other dx/s that the client had in the past that are no longer active) CVA in Feb 2008 & Now 2009, HTN prior to stroke Education Attended Roman Catholic in Phila; entered Navy prior to graduation. Has tried working toward his GED within the past 2 years. City & State of residence Delaware County, PA Employment status & occupation Airplane mechanic for the Navy. After discharge worked as a mechanic for a clothing manufacturer in Kensington. Entered sales. Last employed in 2008 selling Phillies Visa credit cards. Currently unemployed & working on GED Social roles Son, brother, & brother in law 1° caregiver for elderly mother Lifestyle habits (smoking, ETOH, illegal drugs) (-) smoking, (-) illegal DRG, (+) occasional ETOH Other notations Believes that he needs glasses. Describes himself as a “homebody.” Navy veteran who attends the VA for therapy & Aphasia support group. Uses public transportation 100% I’ly. Reasons for Admission (*what is the main reason the person is at you particular facility; e.g., respite, decreased independence in functioning, rehabilitation) N/A Estimated length of stay (ELOS) N/A (*if in long term care, write “N/A, long term care”) Reason for referral to RT (*the reason for referral will vary by setting, please be sure to talk with your supervisor to find out the specific reason for RT treatment/services) Eval & tx Disability Review Review each of the client’s primary diagnoses and secondary diagnoses and answer the following questions in paragraph format (summarize, do not cut and paste): What is the disease/illness/disorder? What causes it? What are the symptoms? What is the prognosis? How is it treated? How do you foresee this information affecting/impacting your tx with the client. Use professional sources (journal articles, professional texts, national organization websites) and cite the sources (if using a website, provide the direct link and if using a journal article or text provide the full references in APA format) Primary Diagnoses LCVA is the loss of brain functions on the left side of the brain due to disturbance in the blood supply to the brain. It affects the ability to speak and understand language. It can be caused back lack of blood flow caused by blockage or a hemorrhage. Stroke symptoms include dysarthria, aphasia, memory loss, lack of reading and writing comprehension, loss of ability to write, and loss of vision. Disability affects 75% of stroke survivors enough to ↓ their employability. It can affect patients physically, mentally, emotionally, or a combination of all three. The results of stroke vary widely depending on size and location of lesion. It is treated by ensuring adequate fluid intake and nutrition, moving limbs at risk of contractures and placing them in appropriate resting positions, ambulation, rehabilitation, and exercise. This information can affect my tx c Baron because he is overweight & has a lack of physical activity which could ↑ the risk of having another CVA. Also, it makes me aware that Baron may have difficulty communicating some things to me because of speech impairment. Merck Manual Staff (2013). Overview of Stroke. Accessed via www.merckmanuals.com/professional/index.html Secondary Diagnoses Spastic dysarthria is a motor speech disorder that affects speech articulation & is caused by lesions of the corticobular tracts. It affects strength, speed, precision, range of motion, and coordination of speech musculature movements. It is treated c medication to ↓spasticity. This information affects my tx plan because pt may have some difficulty c participating in physical activities. Therefore, it is imperative that I refrain from implementing long & strenuous exercises & activities that may cause pain & flaring of gout in pt. Aphasia is a communication disorder characterized by the partial or complete loss of the ability to speak or communicate with written words. It can be caused by BI and can occur 2° losing oxygen during a stroke, brain tumor, or some infection of the brain. Some of the symptoms include speaking in incomplete sentences that do not make sense, inability to comprehend what others are saying, interpreting figurative language literally, and speaking unrecognizable words. Most pt c p CVA Aphasia improve. Tx includes speech exercises in groups & ind, grp thpy, technology assisted thpy, and RxDRG. This info can affect my tx plan because pt may struggle c comprehension and speech, trouble communicating which may cause frustration. Therefore, it is important that pt is in an environment in which he is comfortable & able to take his time while speaking. HTN (high blood pressure) is a chronic medical condition in which the blood pressure is elevated. HTN can be caused by smoking, stress, alcohol intake, potassium deficiency, obesity, salt intake, or family history of HTN. Some of the symptoms include headache, drowsiness, confusion, nausea, vision impairment, nose bleeding, and vomiting. The ↑the bp, the worse is the px, however, effective control of HTN prevents most complications and prolongs life. Tx includes weight loss, exercise, - smoking, -ETOH, eating fruits & vegetables, and salt intake. This information would impact my tx plan because pt may need motivation to eat healthier & incorporate more exercise in his daily living. Afib is the most common irregular heartbeat. It is a problem c the rate or rhythm of the heartbeat which means the heart can beat too fast, too slow, or just have an irregular rhythm. It may not cause any symptoms, but can be associated c fainting chest pains. It increases the risk of CVA. It is treated with a pacemaker, medication, and surgery. Some ways to prevent it include not smoking, drinking in moderation, engaging in physical activity, avoiding caffeine, and eating healthy. This will impact my tx c Baron because Baron will need to participate in more physical activities to ↑his health in order to improve his QOL. Gout is a medical condition usually characterized by recurrent attacks of acute inflammatory arthritis (swollen joint). It is caused by Hyperuricemia (uric acid in blood that is abnormal) Symptoms include joint pain and swollen joints. S tx, an acute attack of gout will usually resolve in 5-7 days, but 60% of people will have a 2nd attack c/in 1 yr. Gout is treated c medication & in order to ↓ symptoms, pt should rest the affected joints. This will impact my tx plan because although Baron needs more exercise & physical activity, his gout may cause fatigue & pain. Therefore, this health precaution is something that I must keep in mind. Medical Dictionary (2013). Spastic Dysarthria. Accessed via http://medical-dictionary.thefreedictionary.com/spastic+dysarthria Merck Manual Staff (2013). Overview of Aphasia. Accessed via www.merckmanuals.com/professional/index.html Merck Manual Staff (2013). Overview of Atrial Fibrillation. Accessed via www.merckmanuals.com/professional/index.html Merck Manual Staff (2013). Overview of Gout. Accessed via www.merckmanuals.com/professional/index.html Functional Skills Assessment Using the facility RT assessment tool, secondary sources (e.g. chart, family, etc.), and/or a standardized RT assessment tool, conduct a functional skills assessment of your client and list your assessment findings in the chart below. Areas of Client Functioning Assessment tool/source/method utilized (e.g., medical chart review, observation within activity, discussion with a specific team member/team/physician, client or family interview, standardized assessment tool, etc), along with a description of WHY you chose this tool/method. Do not cut and paste examples from A&D course. Explain your thought process and what you were hoping to gain from each particular source. Assessment Findings (Measureable Baselines) Write measureable baselines of assessment findings. Prior to each baseline, indicate the source where you obtained the information using the below codes: O = observation MC = medical record T = standardized assessment tool performed by you P = patient hx (anything told to you by the client, family, other team members, etc) Physical functioning Medical Chart Review: I looked in pt notes for info on pt’s MC: amb ~ 1mi mod I physical functioning, particularly Amb & AROM because pt had O: All RUE and RLE AROM WFL a L CVA & I anticipated that he would have difficulty in these O: Strength for R deltoid, biceps, wrist extensors, quadriceps, and areas. ankle dorsiflexion = 5 O: Dynamic standing balance in max ranges mod I – I Direct Request: I asked client to perform UE & LE AROM O: p 5 mins of bean bag catch client verbalized fatigue movements & balance to test functional abilities because I O: throwing the bean bag underhand seemed to be easier for pt anticipated physical impairment p CVA. opposed to overhand tossing. Bean Bag Toss: pt participated in bean bag toss game in order O: R Pincher grasp ¼ inch diameter item WFL to test balance, tolerance, stamina, and level of fatigue. O: R finger-thumb opposition WFL Ring Toss: pt played ring toss in order to test balance Cognitive functioning Medical Chart Review: Reviewed notes in p thx to obtain MC: Suffers from cognitive fatigue at the later part of the day. general overview of cognitive abilities because I anticipated MC: Understanding of complex, verbal ideas or instructions is cognitive impairments p CVA. compromised 50% of the time. MC: Numeric functions are disrupted; # recognition is intact but memorization of phone numbers & accounts is impaired. Ipad Games: Administered Cut the Rope Ipad app in order to O/T: pt required min vc to initiate reading & following written test written direction following/comprehension, new learning, directions on Ipad game (Cut the Rope). and strategizing skills. Administered Simon says app in order to O/T: reading simple instructions on Ipad game I test memory & color recognition. O: A &Ox3 P: pt reports functional ability to write intact, but spelling words are a challenge. Reading Passage: Asked pt to read Phillies passage of 4 O: Read size 14 font s difficulty sentences @ the 4th grade reading level in order to test pt’s O: Post reading 4 sentences @ 4th grade reading level, client able ability to read & ability to comprehend what he read. to recall 3 main points s difficulty. O: When playing the game Simon, pt able to follow 4 step pattern c 4 blocks I’ly. C ↑‘d blocks (↑‘d visual stimuli), concentration waned & only able to complete 2 step pattern. O/T: In Cut-the-Rope game, pt able to complete 1 step challenge I’ly. C ↑‘d challenges required to complete the task, pt’s concentration waned requiring max A. O/T: In Cut-the-Rope game, pt required max A for simple problem solving (didn’t change strategy based on outcome) O/T: Color recognition & ability to comprehend simple verbal directions in Simon game WFL Speech/communication Medical Chart Review: I looked in MC to obtain general MC: mild fluent aphasia functioning overview of pt’s speech pattern because I anticipated speech MC: mild to mod spastic dysarthria impairments p CVA. MC: possible mild apraxia MC: attends VA for tx MC: attends aphasia support group Direct Request/Observation: Asked pt to read Phillies passage O: production of multisyllabic words is a challenge of 4 sentences @ the 4th grade reading level in order to test O: speech production slow & shows signs of dysarthria/halting pt’s speech because I anticipated speech impairments p CVA. speech pattern O: rate & rhythm of speech is slow O: reduced intonation O: during activities, pt read directions, but did not communicate that he did not fully comprehend what was instructed in game directions (Cut the Rope). P: When pt gets frustrated or upset, it is difficult for him to speak clearer & others are unable to understand him. O: pt able to read 4 sentences @ 4th grade reading level. P: pt sometimes struggles c word finding Psychological/emotional Medical Chart Review: reviewed pt notes to obtain an P: Pt gets frustrated or upset when others are unable to functioning overview of pt psychological & emotional functioning because I comprehend what he is saying. When pt is frustrated, speech is anticipated that pt may experience some depression or ↓’d impaired. QOL p CVA. P: while pt acknowledges the loss of friendships p CVA, it appears that he has other support via family (sister & brother-in-law) & aphasia group. Client Interview/Observation: In order to get an idea of pt’s O: Phillies, art exhibitions, & gardening seem to make pt happy. psychological & emotional functioning, I asked questions O: Pt made a few jokes throughout the interview & joked about regarding stress, stress management, people in his life, & how being overweight/out of shape. He also laughed a few times. he feels about himself. This is important because self-esteem & O: Pt does not seem too happy about his life, but rather a little quality of life could have been effected p CVA. content. There are a number of things that he would like to get back to doing such as fishing, fixing computers, etc. O: Because pt is eager to meet new people & make friends, attending more social outings would most likely ↑psychological & emotional functioning. WHO-QOL-BREF: I used this tool to measure Baron’s Findings on the WHO-QOL BREF, when compared to norm- perception of his life in regards to his physical health, referenced scores for chronic CVA, indicate the client’s psychological health, environment, and social relationships. perception of his psychological health is significantly higher than Findings from this tool would help me to determine client’s the norm referenced scores (norm = 59.8, client’s score = 75). satisfaction c in various domains in his life. I expected that he Scores for perceived physical health (63), environment (69), might have issues c QOL due to impairments p CVA. overall perception of QOL (4), and overall perception of health (4) were in line with norm referenced scores. Social relationships however, were significantly lower compared to norm-referenced scores (norm = 62.1, client’s score = 56). Questions in this area related to his level of satisfaction with personal relationships, sex life, and support from friends. Sensory functioning Medical Chart Review: Reviewed notes in MC to obtain a MC: Sometimes presents c a vacant stare & flat affect, but does general overview of pt’s sensory functions because I have the capacity to demonstrate facial emotions. anticipated visual impairment p CVA. P: pt stated that he believes he needs glasses & is scheduling Cataract surgery soon. Ipad Vision Test App: Administered EyeXam app to test visual O/T: Binocular visual acuity test s glasses (Vision Test ipad app) acuity because I anticipated visual impairment p CVA. yielded a 66% indicating difficulty focusing. O: pt hearing & tactile sensation WFL O/T: pt was able to touch ipad screen to conduct EyeXam test Direct Request/Phillies Reading Passage: In order to test pt’s ability to see pt was asked to read 14 size font Phillies passage. Social functioning Medical Chart: Reviewed pt notes to get an idea about pt’s MC: pt describes himself as a “Homebody” social life & relationships c others. Typically, p CVA, people are MC: Attends Aphasia group @ Temple University no longer able to do things that they used to do prior to their P: Pt stated the loss of old friends p CVA, therefore, he no longer injury, therefore, social life & social functioning may be attends concerts c friends impaired. P: Pt stated that he goes out to events c other members of the Aphasia group. Client Interview: In order to get an idea of social skills such as P: Pt stated that he travels alone to & from events on Septa. eye contact, body language, social cues, & initiating & O: It seems that while he goes out c members of the Aphasia maintaining conversation, I interviewed pt. This was important group, I get the impression that he has not really made any because CVA could have affected social skills. friends. O: Throughout interview pt mentioned doing activities c brotherin-law & sister, but never mentioned a friend. O: Pt seems friendly & approachable when conversing c him, but others who do not know him may think otherwise due to the absence of facial expressions O: Pt’s ability to maintain & sustain conversation WFL O: Pt had good eye contact throughout interview O: Ability to read social cues WFL O: Although he seems to have some support from his brother-inlaw, sister, & the Aphasia group, it seems that Baron may need more support. Self-care functioning Medical Chart: Review notes in p thx to obtain general MC: ADLs I overview of pt’s dietary habits, weight, overall health, & I’ence. MC: Pt travels using Septa I’ly & walks to & from subway stations. This is important because being overweight & not eating MC: amb ~ 1mi before experiencing fatigue in which he needs to healthy can put pt @ risk for another CVA. sit & rest. MC: pt walks slower than normal P: Pt does a lot of walking Client Interview: asked pt about level of I’ence & ADLs because P: pt reports mod I ADLs ADL impairments are common post CVA. P: pt reports that he does not exercise as much as he should; lack of physical activities. Pt made jokes about being overweight during interview. P: Pt expressed that he was interested in joining the MOVE exercise program in order to lose weight. MC: health precautions for HTN & gout O: pt is overweight & did not make any statements about healthy eating. Leisure functioning Leisure Lifestyle Review: Explored pt’s current, past, and LLR: pt’s current leisure includes watching TV, listening to the (e.g., standardized future leisure interests to determine health of leisure lifestyle, rock music and the Phillies games on the radio, gardening, leisure assessment what activities motivate him, and what functional abilities are participating in the Active Living for Aphasia group and findings such as the needed for those activities; all of which will be helpful in community outings, and attending art events. He also does a lot LIM, LMS, LAM, LSM; creating a tx plan. of walking and uses Septa I’ly. Pt’s past leisure includes the Leisure Lifestyle repairing/building computers, reading and writing, playing for the Review (below) – be local baseball team, attending rock music concerts c friends, sure to interpret your going fishing c sister and brother in law @ the Jersey Shore, and overall clinical opinion making copies of pictures and disc to send to family members. of the client’s leisure Future interests include getting a chance to meet new people lifestyle; and facility during leisure activities, attending an art exhibit, joining the leisure assessment MOVE Program in order to lose weight, and taking pictures of Temple University’s Campus. P: Client stated, “When the weather is nice, I like to be outdoors.” Medical Chart: Reviewed p thx to see if any notes have been MC: Client’s favorite activities includes watching the Phillies, made regarding client leisure interests that can be explored gardening, attending the aphasia groups, and the community further during RT assessment. outings connected to the Active Living for Persons with Aphasia. Describes himself as a “homebody.” Leisure Motivation Scale (LMS): I used this tool to find out pt’s T: Findings from the Leisure Motivation Scale (LMS) indicate pt is motivation for engagement in leisure activity. During the client motivated to predominantly engage in leisure activities that interview, Baron stated that he enjoys being c others, yet he involve substantial mental activities such as learning, exploring, has a very small social circle. This tool will help determine what discovering, creating, or imagining (A= 53), followed by activities will motivate him to actually do what he enjoys. that require challenges and competition (C=45), and activities that promote friendship, and esteem from other people (B=44). The pt’s lowest motivator to engage in activity is the use of activities that allow him to escape and get away from over stimulating life situations (D=41). Free Time Boredom (FTB): I used this tool to find out the Findings from the FTB indicate that during the pt’s leisure time, degree to which the pt is bored in the four components that he has enough to think about and finds these thoughts make up boredom. During client interview, Baron expressed a emotionally satisfying (Mental Involvement= 4.4). However, pt few activities that he is involved in, but it seems that he has a had lower scores in Speed of Time (3.8), Meaningfulness (3.2), lot of idle time. Administering this tool helped me to measure and Physical Involvement (3.2) resulting in a score of low normal. the extent of boredom that Baron experiences, because if he is These results indicate that the pt does not have a focus or bored, he could be at risk for other health problems. purpose during his free time, that the pt does not have enough purposeful and satisfying activity to fill his time, and the pt does not have enough physical movement to satisfy him. Due to these low normal scores, the pt is possibly putting himself at risk for problems relating to boredom. His total score also reflected a low normal score (3.65). Leisure Lifestyle Review Identify leisure interests and activity patterns for your client. Each activity should be coded as a current, past and/or future interest. Current (C), Past (P), & Future (F) interests (list in this order) C Activity How often With who Where Other notations TV daily I/family members Home pt enjoys watching the Phillies’ games C Gardening/yardwork daily I Home Pt stated “When the weather is nice, I like to be outdoors.” C Active Living for Aphasia weekly Group C Listen to radio Friends in Aphasia Temple University group daily I pt uses Septa I’ly to & from Temple University Home pt enjoys listening to sports stations and Rock music Leisure Lifestyle Review cont. Identify leisure interests and activity patterns for your client. Each activity should be coded as a current, past and/or future interest. Current (C), Past (P), & Future (F) interests (list in this order) C Activity How often With who Where Other notations Local art exhibitions monthly I Philadelphia Pt just recently started visiting exhibitions & enjoys art. P Little League Baseball Daily friends N/A Pt was a part of the local softball team P Rock concerts N/A friends N/A Pt lost contact c friends p CVA P Fishing N/A Sister & brother-in-law Jersey Shore P/C/F Photography daily I Phillies games, Temple University Campus P Repairing/Building daily I Home N/A I N/A Computers F MOVE Exercise Program Pt wants to lose weight & believes that the program will be motivation to be healthier F Social Activities Weekly friends N/A Pt wants to get the chance to meet new people while participating in leisure activities.