Occupational Safety - College of Agriculture and Life Sciences
advertisement

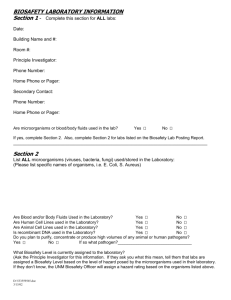
Biosafety in the Workplace PLS 4/595D /Regulations and Laboratory Management Spring Semester, 2006 Mark J. Grushka, M.S., CSP Manager, Biosafety and Biosecurity University of Arizona Main Topics Part 1 Introduction to Biological Safety Principles (Tuesday/April 11th) Part 2 Introduction to Regulatory Framework (Tuesday/April 11th) Part 3 Biosafety Program Management, Application of Project Management Techniques and Case Studies Part 1 Introduction to Biological Safety Principles Definitions Key Principles Data on Laboratory Acquired Infections Risk Assessment Biosafety Containment Levels Primary Containment Emergency Preparedness Introduction to Biosafety Principles Complex relationship between organisms and hosts. We are surrounded by countless microorganisms. Our bodies depend upon them for natural processes such as digestion. But most of time, we do not get sick because of natural defenses. Infectious (pathogenic) organisms must: – Attach and survive hosts defenses – Multiply – Create signs and symptoms of disease in host Definitions Safety Risk Biosafety Biosecurity Safety Freedom from harm Control of accidental losses involving – People – Property – Loss to process Risk The chance that something may or may not happen. Often defined as: – Frequency (how often) – Severity (how bad) Biosafety “Development and implementation of administrative policies, work practices, facility design, and safety equipment to prevent transmission of biological agents to workers, other persons or the environment” MMWR December 6, 2002 Biosecurity “Protection of high-consequence microbial agents and toxins, or critical relevant information, against theft, or diversion by those who intend to pursue intentional misuse” MMWR December 6, 2002 Koch’s Postulates 1890 Robert Koch Established List of Criteria to Judge Whether or Not a Given Microbe Was Responsible for a Given Disease – The organism must be present in every case of the disease – The organism must be isolated from the diseased host and grown in pure culture – The specific disease must be reproduced when the pure culture is inoculated into a healthy susceptible host – The organism must be recovered from the experimentally infected host Biohazardous Materials Include All Infectious Organisms (Bacteria, Chlamydiae, Fungi, Parasites, Prions, Rickettsias, Viruses) which can cause disease in humans or cause significant environmental or agricultural impact. Materials that may harbor infectious organisms such as human or primate tissues, fluids, cells, cell cultures. Key Principles of Biosafety Laboratory Practices and Techniques – Hand Washing Important – Manipulation of Material to Minimize Aerosols – Consistent Use of Personal Protective Equipment Safety Equipment (Primary Barriers) – Biological Safety Cabinets (BSC’s) Facility Design and Construction (Secondary Barriers/Room Design) – Room Pressure Negative to Corridor – Controlled Access to Non-Research Personnel Medical Surveillance Typical Routes of Entry for Viral or Bacterial Pathogens Inhalation Ingestion Injection – Needle sticks – Accidental cuts with sharp objects Skin or Eye Exposure Laboratory Acquired Infections Risk of Laboratory Associated Infections (LAI’s) is Real Historical Examples Include:Brucellosis, Q Fever, Hepatitis, Typhoid Fever, Tuberculosis, Hepatitis Of the 3921 LAI Only 703 (18%) Caused by Identifiable Accidents including needle sticks, broken glass, spills or sprays (R.M. Pike 1976) 40 Years of Data on Overt LAI’s Pike, R.M. 1978 Various Classes of Agents No. of Case No. of Deaths No. of Agents Involved No. of Published Cases Bacteria 1704 71 37 744 Viruses 1179 55 85 915 Rickettsiae 598 25 8 381 Fungi 354 5 9 313 Chlamydiae 128 10 3 71 Parasites 116 2 17 74 Totals 4079 168 159 2498 Agent Ten Most Frequently Reported LAI’s Pike, R.M. 1978 Past and Present Hazards of Agents Infection No. of Cases No. of Deaths Brucellosis 426 5 Q Fever 280 1 Hepatitis 268 3 Typhoid Fever 258 20 Tularemia 225 2 Tuberculosis 194 4 Dermatomycosis 162 0 Venezuelan Equine Encephalitis 146 1 Psittacosis 116 10 Coccidiodomycosis 93 2 Totals 2168 48 University’s Responsibilities To provide a workplace free of recognized hazards. UA Policy and OSHA Requirement To provide training to employees in order to recognize hazards and to protect employees against those hazards. Methods of controlling risk may include: – Building Design Including Containment Features (Primary/Secondary) – Policies/Procedures (SOP’s) – Personnel Protective Equipment – Medical Surveillance Programs Basic Risk Assessment Framework Hazard Identification Estimate Probability of Occurrence Decide on Acceptable and Non-Acceptable Practices Implement Practices Monitor Example of Risk Assessment for Cell Culture BELGIAN BIOSAFETY SERVER http://www.biosafety.be/CU/animalcellcultu res/mainpage.html – Introduction Bioline International http://www.bioline.org.br/request?by95008 Risk Assessment Flow Chart Employee Responsibilities If you don’t know, ask. If you have not been trained to do it, don’t! Follow established biosafety practices and procedures. Always ask Principal Investigator. Immediately inform Principle Investigator or Laboratory Manager if any accidents, spills, procedural issues/concerns or any questions arise about your safety or the safety of others. Biosafety Levels Defined BSL-1 BSL-2 BSL-3 BSL-4 Biosafety Level One (BSL-1) BSL-1 Work with Well Characterized Agents Not Known to Cause Disease in Healthy Adults. Standard Microbiological – Open bench tops acceptable with good standard microbiological practices – Laboratory not necessarily separated – Special containment equipment or facility design not required Examples include E. coli K-12, Bacillus subtilis Also Called “Bench Work”. Biosafety Level Two (BSL-2) BSL-2 Work with Moderate Potential to Affect Personnel and Environment. (Herpes, Influenza viruses, Legionella sp.) – Personnel are specifically trained to handle pathogenic agents – Lab access limited when work is conducted – Extreme precautions taken when handling contaminated sharp items (needles, scalpels) – Appropriate immunizations are administered when available and baseline serum samples encouraged – Certain procedures require biological safety cabinets Biosafety Level Three (BSL-3) BSL-3 Work May Cause Serious or Potentially Lethal Disease as a Result of Exposure to Inhalation Route. (M. Tuberculosis, Bacillus anthraces) – – – – Very specific training Biosafety Cabinets used Appropriate PPE and other clothing Specific engineering and design features Additional (BSL-3) Requirements Immunization and medical surveillance protocols required No open bench work Ducted exhaust air ventilation creates directional airflow from “clean” toward “contaminated” areas prior to discharge to outside High Efficiency Particulate Air (HEPA) filters may be required for room exhaust Biosafety Level Four (BSL-4) BSL-4 Work with dangerous and exotic agents which pose a high risk of aerosoltransmitted laboratory infectious and life threatening disease. Ebola, Marburg, – Special facility design features required – All activities confined to Class III biosafety cabinets (glove boxes), or Class II BSC’s used by workers using one piece positive pressure personnel suits ventilated by a life support system Identifying Biohazard Risks What am I Working With? How Can it Cause Disease and How do I Protect Myself? Routes of Entry Include Inhalation, Ingestion, Inoculation, Skin and Eyes Typical Risks of Exposure Include Contaminated Needles, Mouth-Pipetting, Splashing, Animal Bites How to Protect Yourself Knowledge and Understanding of the Biohazards You Are Working With How Can it Get Onto/Into My Body How to Protect Myself (Hierarchy of Control) – Containment Equipment – Techniques – Personal Protective Equipment Identifying Biohazard Risk is Key Accident/Incident Preceded Events Represented Only 18% of LAI’s Aerosols, Droplets and Fomites are Likely Sources Lab Techniques With High Potential for Exposure Include: – Centrifuges/Blenders, Opening Tubes/Bottles, Syringes/Needles, Inoculating Loops, Heating Over Flames Mammalian Tissue Culture Work Risks – Tissue culture may contain virus or bacteria capable of spreading to human host – Integrity of culture may be altered because of contamination from outside source How to Reduce Risks to Human and Cell Culture? – Manipulation of tissue cultures only under Class II Biological Safety Cabinets – Use care when doing any procedure using instruments that may break skin – Use proper PPE like latex gloves, eye protection Class II Biological Safety Cabinets Explained Main Function – Protects Worker – Protects Work (Tissue Cultures From Microbial Contaminants, i.e.. Integrity of Cultures) Features – High Efficiency Particulate Air (HEPA) Filter Minimizes Escape of Contaminants Within Cabinet Into Lab – HEPA Filtered Air Supply Bathes Work Surface, Protecting Work Certified Annually by Facilities Management Basis of Primary Containment Isolate the Laboratory Worker from Biological Agent With Ultra Filtered Directional Air Currents Class II Type B1 Biological Safety Cabinet Air Flow/HEPA Filter Placement Proper Use of Biosafety Cabinets Do’s – Become familiar about the equipment by reading users manual and asking PI. – Keep laboratory doors closed and minimize movement in front of cabinet to avoid disrupting airflow. Avoid rapid arm movement in and out of BSC. – Decontaminate work surfaces with disinfectant before and after working in a cabinet according to laboratory standard operating procedures (SOP’s). Proper Use of Biosafety Cabinets Don’ts – Do not use cabinets as a permanent storage area for supplies (disrupts airflow) – Do not work inside cabinet with UV lamp on, if so equipped. (skin/eye burns) – Do not rapidly insert or withdraw arms. (disrupts airflow) – Place required equipment or supplies for procedure inside before beginning work. (minimizes hand/arm withdrawals which can disrupt airflow) Eagleston Institute Biosafety Cabinet Clips What Does Your Lab Look Like? Advantages of Good Housekeeping Reduces Risk of Slip, Trip and Falls Protects Integrity of Biological Experiments by Providing Adequate Space and Reduce Contamination Potential Easier to Decontaminate Surfaces Saves Time by Being Able to Find Stuff Emergency Preparedness What Should I Do When Things Go Wrong? – Learn the types of emergencies that could happen Spills of liquids Equipment malfunctions Exposure to potential pathogens through inhalation, ingestion, skin including eye exposure, needle or other sharps – Learn how to respond to minimize exposure time and concentration – Contact your supervisor to protect your health and legal rights Biohazard Spills Each Lab Required to Have Spill Decontamination Plan PI Required to Have Cleanup/Decon Procedure for Specific Biohazards Found in Lab If Spill Occurs/General Guidelines – – – – Remove affected clothing/gloves Wash contaminated body areas with soap/H2O Secure area until cleanup completed Call UA Risk Management 621-1790 for technical assistance Summary Risks of Working with Biological Materials in Research are Real The Risks Can be Managed Through: – Properly Identifying and Assessing Biological Risks – Good Laboratory Practice and Technique – Correct Use of Safety Equipment (Primary Barriers) Including Biological Safety Cabinets – Facility Design, Construction and Maintenance (Secondary Barriers) Additional Resources are Available Through Institutional Biosafety Committee and Professional Staff Regulatory Framework PLS 4/595D /Regulations and Laboratory Management Spring Semester, 2006 Mark J. Grushka, M.S., CSP Manager, Biosafety and Biosecurity University of Arizona Part 2 Introduction to Introduction to Regulatory Framework What are the major regulations covering biosafety? How is the University of Arizona organized for biosafety compliance? What are the future implications for regulatory control of biosafety? Introduction The regulatory framework covering biosafety can be characterized as a combination of statutes, regulations, rules and guidelines from various federal and state agencies, private and public organizations and other interested parties such as manufacturers of containment equipment Federal Laws Occupational Health and Safety Act (OSHAct) Bloodborne Pathogens (29 CFR 1910.1030) Occupational Exposure to Hazardous Chemicals in Laboratories (29 CFR 1910.1450) Personal Protective Equipment (29 CFR 1910.132-139) Needlestick Standard National Institutes of Health NIH Office of Biotechnology Activities NIH Guidelines for Research Involving Recombinant DNA Molecules IBC Resources USDA APHIS USDOT HazMat Safety Hazardous Materials Regulations (49 CFR 100-185) US EPA Hazardous Waste Microbiology IAQ Select Agents All individuals who have access to Select Agents must undergo a Security Risk Assessment Acquisition, use, transfer and disposal of Select Agents is monitored by CDC/APHIS through issuance of registration How is the UA Organized to Comply? Compliance based at Vice President for Research Office Manager of Biosafety and Biosecurity Chairman of the Institutional Biosafety Committee Program Coordinator UA and Regulatory Reality Check Institution Governed by Many Internal Policies and External Laws/ Regulations – Provides a “Road Map” for Establishing and Monitoring Effectiveness of Biosafety Program – Keys to Success Accountability (Who is in Charge) Clear Goals and Objectives Periodic Monitoring Regulations and Guidelines for Biosafety at UA Occupational Safety and Health Act (OSHA) – Blood borne Pathogen Standard (Required Training for All Employees Who Work With Human Tissues, Blood or Other Bodily Fluids Must Take Course From UA Risk Management) University of Arizona Biosafety Handbook Biosafety in Microbiological and Biomedical Laboratories (CDC/NIH) NIH Guidelines for Research Involving Recombinant DNA Molecules Laboratory Specific Procedures (SOP’s) Institutional Biosafety Committee Requires a Written Plan from PI for These Types of Research Recombinant DNA Pathogenic Microorganisms Mammalian Cell Lines Gene Therapy Institutional Biosafety Committee Basics Reports to Vice President for Research Insures a safe working environment by minimizing exposure of personnel to harmful biological agents Peer Review of research conducted at or sponsored by the U of A for compliance with adopted policies, regulations and guidelines Where to Get More Information (IBC Website) http://www.ibc.arizona.edu (Risk Management Website) http://www. w3fp.arizona.edu/riskmgmt http://cdc.gov http://labor/osha.gov Mark J. Grushka, Manager, Biosafety and Biosecurity 621-5279 and Margaret Stalker, Program Coordinator 621-3441 Criteria for Review Use of Pathogenic Materials Use of rDNA techniques Use of Cell Culture Transgenic Plants Gene Therapy Memorandum of Understanding and Agreement Form Is the main risk assessment document submitted by Principal Investigators Submitted in on-line form Reviewed at least twice – Prereview – Committee Review Approval from IBC allows PI to conduct research at specific BSL level Auditing Function All BSL-3 laboratories audited annually by Manager of Biosafety All Select Agent laboratories audited annually by Manager of Biosafety All BSL-1 applications require an on-site inspection prior to consideration by IBC Other Resources Training – Bloodborne Pathogen and Shipping of Hazardous Materials by Air done by Risk Management and Safety On-line UA Biosafety Handbook Program Manager,Manager of Biosafety and IBC Chair available to respond to technical or regulatory questions Guidance Documents World Health Organization Biosafety Manual http://www.who.int/csr/delibepidemics/ WHO_CDS_CSR_LYO_2004_11/en/ 2nd Edition Primary Containment for Biohazards:Selection, Installation and Use of Biological Safety Cabinets http://www.cdc.gov/od/ohs/biosfty/bsc/bsc.htm Biosafety in Microbiological and Biomedical Laboratories (BMBL) 4th Edition http://www.cdc.gov/od/ohs/biosfty/bmbl4/bmbl4t oc.htm Part 3 Biosafety Program Management, Application of Project Management Techniques and Case Studies PLS 4/595D /Regulations and Laboratory Management Spring Semester, 2006 Mark J. Grushka, M.S., CSP Manager, Biosafety and Biosecurity University of Arizona How to Organize a Biosafety Management Program Goals Elements Risk Assessment Training Medical Surveillance Documentation Goals To prevent employees and their families from acquiring laboratory-associated infectious diseases To prevent contamination of the environment and promote environmental quality To comply with all National, International and Local regulations for the use of biohazards To conform to prudent Biosafety practices Slide2 ELEMENTS OF A BIOSAFETY PROGRAM Organization Biosafety Manual Registration and Inventory Control Risk Assessment and Control of Biohazards Biosafety Training Emergency Response Medical Surveillance Auditing Program Documentation Slide7 ELEMENTS OF A BIOSAFETY PROGRAM Organization Management Commitment Through Leadership Designation of a Biosafety Officer Management appoints an individual qualified by training and experience Role of Site Safety Teams Establish a mechanism to monitor and control the use of biohazards which can be done through the Site Safety Team Establishment of Responsibilities: Designate responsible individuals: Management Biosafety Officer (Site Safety Leader) Committees Supervisors Associates Slide 8a ELEMENTS OF A BIOSAFETY PROGRAM Organization Site Biosafety Committee(s) Biosafety Committee (CDC) – – – – Infectious Agents (Viruses, Bacteria, Parasites) Infected Materials (Human Blood, Body Fluids, Tissues) Animal Pathogens (live vaccine challenges) Zoonotic Agents (non-human primates, other animals) Institutional Biosafety Committee (NIH) – – – – – recombinant DNA (rDNA) Work with Restricted Agents Infectious Host Vectors Human Gene Transfer Experiments Transgenic Animals Cloning of Toxin Molecules Slide8b ELEMENTS OF A BIOSAFETY PROGRAM Biosafety Manual Develop a Biosafety Manual to include: – Engineering Controls Biosafety Cabinets (BSCs) [BSL-2/3] HEPA filtered glove boxes (BL-3) Sealed centrifuge cups – Work Practice Controls Decontamination of lab surfaces daily – Standard Operating Procedures for Work in the Microbiology Lab: Handling of Cultures/Samples Spill Response/Decontamination Biohazard Waste Decontamination/Disposal – Training Program and Documentation – Vaccination Program (as required) Hepatitis B Vaccine/ Vaccinia virus vaccine Slide9 ELEMENTS OF A BIOSAFETY PROGRAM Registration and Inventory Control Registration Identify Infectious Agents (e.g., Mycobacteruium tuberculosis, Brucella melitensis) Determine the Biosafety Level (BSL 1, BSL-2, BSL-3) Identify Procedures (description of work, aerosol generating, culture work, waste treatment, spill clean-up, etc.) Identify appropriate storage conditions (refrigeration, frozen at -20 or 70 degrees C, freeze-dried) Assign Responsibilities to designated individuals Inventory Control Document Physical Inventory Document Location of Infectious Agents Document Controls to be Used such as Biosafety Cabinets, special equipment (sealed centrifuge rotors, etc.) Document Assigned Responsible Individuals Slide10 BIOHAZARD RISK ASSESSMENT Identify Hazard Biohazard identity/name e.g., Mycobacteruium tuberculosis, Brucella melitensis Infectious to humans Humans are the primary host Infectious to animals Animals are the primary host or reservoir of agent Infectious for other living things in the environment Plants, algae, insects Slide11a BIOHAZARD RISK ASSESSMENT Quantify Risk What is the Biosafety Level (BL-1,BL-2,BL-3) What is the amount of infectious material present What is the infectious dose (amount of infectious material needed to cause infection in a normal person) What is the mode of infection – aerosol, percutaneous, ingestion, absorption What is the Portal of Entry – Nose via inhalation – Through the skin via injection or puncture – Mouth via eating or drinking – Directly on the skin or an abrasion of the skin Slide 11b BIOHAZARD RISK ASSESSMENT Quantify Risk (Continued) What is the Condition of the Host Immunocompromised because of drug therapy or illness Immunocompromised due to a primary infection and therefore more susceptible to secondary opportunistic infections What is the Availability of Vaccine Is there a vaccine available against the biohazardous agent What is the protective factor of the vaccine (is it effective for 60%, 80% or 100% of all individuals) What is the Availability of Drug Treatment Is the biohazardous agent susceptible to antibiotic treatment What is the resistance of the agent for antibiotic treatment (e..g., multi-drug resistant M. tuberculosis) Is there a drug therapy for viral agents (e.g., acyclovir, pencyclovir) Slide11c BIOHAZARD RISK ASSESSMENT Identify Controls Hierarchy of Controls Substitution/Elimination – Use a non-pathogen whenever possible Engineering Controls – Primary Containment • • Biosafety Cabinets, Glove Box Enclosures – Secondary Containment • Building Design Features negative air pressure floor to ceiling walls closed doors Slide 12a BIOHAZARD RISK ASSESSMENT Identify Controls Hierarchy of Controls (continued) Administrative Controls – – – – – Frequent hand washing Frequent changing of PPE Removal of PPE when leaving work area Prohibition of eating, drinking, smoking, chewing gum Limiting use of needles and sharps Personal Protective Equipment – Protective eyewear • Safety glasses with side-shields or facemask – Protective outer wear • Use of latex gloves, lab coats – Respiratory Protection • HEPA filter mask (Dust-mist, N95, N100, etc.) Slide 12b ELEMENTS OF A BIOSAFETY PROGRAM Biosafety Training Identify Agents to be Used – To ensure that workers know signs/symptoms of infection and pathogenicity of agent used Provide General Biosafety Training – To ensure that workers know the basics of Biosafety Practices: • Microbiological aseptic techniques • Proper techniques for decontamination/disinfection • Selection and use of Personal Protective Equipment Provide Task-Specific Training – Especially critical for work in BLS-2 and BLS-3 areas Provide Information on Appropriate Vaccination(s) – Workers need to know all about the vaccine(s) they will be using (e.g., efficacy, side effects, booster requirements, etc.) Evaluate Effectiveness of Training – Quizzes, Tests, Observations, Performance Evaluations Slide 15 ELEMENTS OF A BIOSAFETY PROGRAM Emergency Response Develop Written ER Procedures Ensure the ERP is accessible to all employees (located in critical areas) Ensure the ERP is communicated to employees and outside agencies Ensure Adequate Training Employees must be trained to the appropriate response level Ensure Use of Appropriate PPE Employees need to be involved in the selection process Employees need to be trained in the use and maintenance of PPE Supervisors need to encourage/enforce use of PPE Practice ER Drills The ERP needs to be practices (emergency evacuation, spill clean-up) Ensure Post-Exposure Medical Surveillance Injured responders must report injury and get medical attention/follow-up Slide 16 ELEMENTS OF A BIOSAFETY PROGRAM Medical Surveillance Baseline Physicals – Employee’s history, Family history, Serum banking Immunizations (as appropriate) – Vaccination, Titre checks Emergency First-Aid – Medication, Consultation, Medical Follow-up Adequate Training in Recognition of Symptoms – Provided to employees at risk Accident/Injury Reporting Procedure – Investigation, Root Cause Analysis Slide17 ELEMENTS OF A BIOSAFETY PROGRAM Auditing Program Types of Audits/Inspections Regular Self-Inspections conducted by designated employee(s) on a routine basis (daily/weekly) Supervisor Self-Inspection conducted by the supervisor on a weekly/monthly basis to reinforce regular employee inspections Site/Department Inspection Performed quarterly by a site team of employees, supervisors and site management representative(s) Periodic External Audit Performed annually by auditor outside of the site operations (e.g., Corporate staff, another site, an outside consultant) Inspection Follow-up Ensure corrective actions are taken to eliminate identified deficiencies Slide 18 ELEMENTS OF A BIOSAFETY PROGRAM Maintain Documentation Registration Approval Signed by the Investigator, the Department Director and the Biosafety Officer (Safety Coordinator) Medical Records For medical clearance, physicals, vaccinations, diagnostic test results, postexposure evaluations, annual check-ups Vaccination Records Include declinations where appropriate Date of vaccination, blood titers, booster requirements and completion of vaccination protocols Training Records Document initial training, supervisor training, refresher training Include dates, trainer qualifications, course syllabus, sign-in sheet, method of evaluation (tests/quizzes), certificates issued Auditing Records Ensure all inspections/audits are documented including actions taken Slide 19 Documentation Framework Policy Mandatory Global Goal Orientated Other equivalent Global Preferred means allowed Approach Not mandatory unless mandated by Standard Standards Auditable Codes (Management Systems) Audience Specific MSDS Tech Info Training Sector Guidance Specialist Reference Should vs. Shall Tools Product Info The Vice President for Research’s Walkabout for Biosafety Introduction In the spring of 2001, Vice President for Research and Graduate Studies, Dr. Richard Powell initiated a program to acknowledge excellence in research through successful integration of the principles and practices of biosafety management. The success of research depends on intelligent identification, evaluation, and control of risk. The following exemplifies how this is being accomplished at the University of Arizona. Examples of the Walkabout Dr. Friedman’s TB Lab Noted for Excellence in Biosafety Procedures May 2001 http://www.ahsc.arizona.edu/opa/ahsnews/may01/powe.htm Shubitz’s Valley Fever Lab Recognized for Biosafety Excellence July 2001 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/1/wa/LQPStoryDetails?ArticleID=39 22&wosid=UtPtDpXbJrhSbEVlsgCHxg VP Research Recognizes Three for Biosafety Excellence October 2001 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/wa/MainStoryDetails?ArticleID=438 4 VP Research Recognizes Biological Cabinet Maintenance Staff for Biosafety Excellence January 2002 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/wa/LQPStoryDetails?ArticleID=4 796 Examples of the Walkabout Sterling Parasitology Laboratories Recognized as a Model of Biosafety Excellence April 2002 http://ali.opi.arizona.edu/cgibin/WebObjects/UANews.woa/1/wa/LQPStoryDetails?ArticleID=53 24&wosid=dFxhwGQJUxgVVczUhMKgq0 VP Research Recognizes UA Unit for Managing Hazardous Waste July 2002 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/1/wa/LQPStoryDetails?ArticleID=58 80&wosid=fUuz5a8K0ndElr2pg4xHgM VP Research Recognizes Mirror Lab for Excellence in Health, Safety Leadership December 2002 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/5/wa/LQPStoryDetails?ArticleID =6521&wosid=CuIsRJGISTHGsQtpJ3cu30 http:// Examples of the Walkabout VP Research Focuses Walkabout on Microbiology and Biosafety April 2003 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/5/wa/LQPStoryDetails?ArticleID=72 25&wosid=gvjtwRNtmTIsrxIFWDDTig VP Research Recognizes Biosafety Excellence in Molecular Agriculture Research October 2003 http://uanews.org/cgibin/WebObjects/UANews.woa/wa/MainStoryDetails?ArticleID=810 3. University Animal Care, Research Labs Designed with Effectiveness, Safety in Mind January 2004 http://uanews.opi.arizona.edu/cgibin/WebObjects/UANews.woa/5/wa/LQPStoryDetails?ArticleID=86 04 Examples of the Walkabout Veterinary Diagnostic Lab Integral to Risk Assessment March 2004 http://ali.opi.arizona.edu/cgibin/WebObjects/UANews.woa/5/wa/LQPStoryD etails?ArticleID=8856 VP Research Highlights Excellence in UA Animal Hazards Program September 2004 http://ali.opi.arizona.edu/cgibin/WebObjects/UANews.woa/7/wa/LQPStoryD etails?ArticleID=9759 Scenario 1: The Dedicated Post-Doc Situation: – A new Post-Doc has just arrived from a prestigious University. He is working on improving the production of Interferon from a human cell line. Unfortunately the cell line also produces Human T-cell leukemia virus. He brings this cell line in from the University where he was working before and decides to grow it up in incubators in several labs without telling anyone else working in those labs that it is also co-contaminated with HTLV III. What How do you do? can this have been avoided? Slide 21 Scenario 2: The Helpful Lab Worker Situation: – A lab assistant in a private lab is working with a mouse cell line that has been genetically modified to produce the entire genome of HIV without the LTR sequences (so it is non-infectious). She has been contacted by a very prestigious colleague from another private institution in Europe and was invited to visit their lab. She decides to take along a vial of her cell line packaged in liquid nitrogen. To make sure there is no delay she is hand carrying the vial on the plane in her carry-on bag. Is this wrong? Why? How can this have been avoided? Slide 22 Scenario 3: The Reluctant Director Situation: – Your institution is just implementing a new Biosafety Program. Up until now no one has ever questioned the Laboratory Animal Sciences (LAS) Department about their work. The Director of LAS is reluctant to have his department participate in this newfangled program that is only going to hamper his group and make life more difficult for him and his people. What can you do to ensure that LAS participates in the program? Slide 23 Scenario 4: The Busy Scientist Situation: – A Nobel winning scientist is working in your company. He is a very important person and is much too busy to attend any Biosafety training sessions or let his assistants attend. Besides, what could you possibly show him? What do you do? How can you convince him of the need to attend training? How can this have been avoided? Slide 24