Health, Accident, and Retirement Benefits 2010
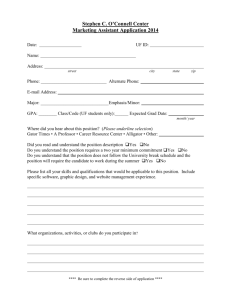
advertisement

Health, Accident, and Retirement Benefits February 20, 2010 Sharon Goldsand, CPA, CPP Payroll Manager 815-754-6548 Sharon.goldsand@Tegrant.com Types of Benefits Offered by Most Employers Health Insurance Sick Pay Worker’s Compensation Insurance Retirement and Deferred Compensation Plans Health Insurance Traditional Health Insurance Plans Health Maintenance Organizations (HMOs) Preferred Provider Organizations (PPOs) Tax Treatment of Accident and Health Insurance Contributions Non-Taxable Contributions Contributions made by an employer Contributions made under a Section 125 Cafeteria Plan If employer reduces salary and then reimburses premium to employee, then the premium is taxable to the employee Premiums must be for Employee, Spouse, Dependents (on 1040) For purposes of this provision dependent will continue to apply to a person who is receiving more than ½ his/her support from the taxpayer even if he/she earnings more than the annual exemption. Tax Treatment of Accident and Health Insurance Contributions Premiums for life partners are federal taxable unless recognized as a spouse under state law. If the employee’s domestic partner is of the same sex as the employee, the partner does not qualify as the employee’s spouse for federal tax purposes regardless of the state law. The partner may qualify as a dependent if partner receives more that ½ support from employee, lives with employee, and the relationship does not violate local law. Tax Treatment of Accident and Health Insurance Contributions What Taxes are Involved Federal Income Tax Employment Taxes Social Security Medicare FUTA Illinois follows the federal government – some state and local jurisdictions do not. Tax Treatment of Accident and Health Insurance Contributions In Order to exclude from employment taxes (Social Security, Medicare and FUTA) Must be under a plan – based on one of the following Plan is written Referred to in employment contract Employees contribute to the plan Employer contributions are made to a separate fund Employer is required to contribute Tax Treatment of Accident Health Insurance Benefits Benefits received directly or indirectly reimbursing the employee for medical expenses incurred are not included in employee’s income Any reimbursements in excess of actual expenses are taxable income to the employee Payments for loss of limb or disfigurement as part of AD&D are not included in income (payments must not be related to time lost from work). Nondiscrimination Requirements for Health Insurance If insurance is provided through third party insurance company there is no requirement. If employer is self-insured (reimbursing employees’ medical expenses from its own funds), employer may not discriminate in favor of highly compensated employees in either benefits or eligibility. IRS Code Section 105(h) Discriminatory Plan Amounts paid to highly compensated employees must be included in taxable income Who is Highly Compensated 5 highest-paid officers Owner of more than 10% of employer’s stock Top-paid 25% of employees Discriminatory Plan Although discriminatory reimbursements are taxable to the highly compensated employees receiving them, they are not subject to federal income tax withholding or employment taxes. Long Term Care Insurance Treated as accident and health insurance under “Health Insurance Portability and Accountability Act of 1996” Employer provided coverage is excluded from income Benefits are excluded from income If per diem – excludible limit is $290/day in 2009 (indexed for inflation) Excess will be excluded to the extent of actual cost of care Long Term Care Insurance Restrictions Not subject to COBRA Cannot be part of Cafeteria Plan If part of flexible spending arrangement it is included in employee’s taxable income Consolidated Omnibus Budget Reconciliation Act of 1985 (COBRA) Requires health plan sponsors to provide employees and their beneficiaries with the opportunity to elect continued group health coverage for a given period should their coverage be lost due to “qualifying event” Applies to employers with 20 or more employees (FTEs) on typical business day. Coverage period generally is 18 to 36 months. COBRA Coverage same as provided to similarly situated beneficiaries who have not suffered the qualifying event. Employees who purchased health care coverage under a cafeteria plan (including flexible spending) are eligible for COBRA continuation at level of coverage before event. Long Term Care Insurance is not included in COBRA COBRA Qualifying event – period of coverage Death of covered employee – 36 months Covered employee’s termination of employment or reduction in work hours (other than gross misconduct) – 18 months If the reason for absence is employee’s military service – 24 months If another qualifying event occurs (other than employer’s bankruptcy) period extends to 36 months. Qualified beneficiary (employee or dependent) is disabled under Social Security Act during the first 60 days of continued coverage - 29 months Another qualifying event during 29 months (other than employer bankruptcy) extends coverage to 36 months COBRA Qualifying event – period of coverage Employer’s bankruptcy Coverage is life of retiree or retiree’s spouse. Once retiree dies – 36 months for retiree’s spouse and children from date of retiree’s death Divorce or separation of covered employee (date of divorce is the qualifying event) – 36 months Dependent child losing that status – 36 months COBRA Premium Requirements Can be up to 102% of the group premium paid for similar coverage under the plan by the employer and employees. The maximum premium increases to 150% for disabled qualified beneficiaries after the 18th month of continuation coverage. Premium payment may not be required earlier than 45 days after the qualified beneficiary elects continuation of coverage COBRA Election and notice provisions Election period must last at least 60 days from the date when coverage was terminated or the qualified beneficiary receives notice – which ever is later. Plan must provide written notice of COBRA continuation coverage when coverage begins Employee or Employer must notify plan administrator of qualifying event, responsibility and timing depends on the event Once aware of the qualifying event, plan administrator has 14 days to notify qualified beneficiaries of their rights. COBRA Penalties for Noncompliance Employers subject to $100 per day penalty for each qualified beneficiary (maximum $200 per day per family affected by same qualifying event). Penalty will not be imposed if failure is due to reasonable cause and is corrected within 30 days of discovery Unintentional failures due to reasonable cause – maximum penalty is lesser of 10% of employer premiums for group health plans during preceding taxable year to $500,000 Savings Plans and Reimbursement Accounts for Medical Expenses Archer MSA (Medical Savings Accounts) Health Reimbursement Arrangements (HRA) Health Savings Accounts (HSA) Medical Savings Accounts (Archer MSA) Established by Health Insurance Portability and Accountability Act (HIPA) of 1996 Small Employers (no more than 50 employees). Eligibility can continue for all employees until the year after the employer has 200 employees. At that point only employees currently enrolled can continue to contribute Employee must be covered only by high deductible health insurance plan. For 2009 annual deductible $2,000 – $3,000 for individual $4,000 $6,050 for family. Maximum out-of-pocket expenses can be no more than $4,000 for individual coverage and $7,350 for family coverage. Cannot be part of Cafeteria Plan Tax Treatment of Archer MSA Contributions can be made by employer or employee (not both) Employee contributions are deductible from income on personal tax return. They are subject to federal income tax withholding and employment taxes. Employer contributions are excludable from income. Limitations on Contributions to Archer MSA Employee deduction cannot exceed employee’s compensation Deduction or Contribution is limited to 65% of the plan deductible for individual coverage or 75% of the plan deductible for family coverage. Employer contributions must be the same amount for each employee based on either dollar amount or percentage of applicable deductible. Employer contributions in excess are included in income. Archer MSA – Tax Treatment of Distributions Distributions from MSAs are excluded from income if they are for medical expenses incurred by employee or his/her dependents. Person for whom expenses are incurred must be covered only by high deductible health plan. Distributions included in income are subject to an additional 15% tax unless made after age 65, disability, or death. MSA Trustee or Custodian is not required to determine use of distributions; this is the responsibility of the account holder. Archer MSA – Information Reporting Requirements Employer Contributions Employee Deductions Box 12 R on W-2 Plan trustees report on 5498-MSA Reported on employee’s personal tax return Box 1, 3 and 5 on W-2 Employee takes deduction on personal income tax return for amount contributed Plan trustees report on 5498-MSA Distributions Plan trustees report on 1099-MSA Health Reimbursement Arrangements (HRA) Paid solely by employer (not salary reduction election or cafeteria plan) Not limited by number of employees or only to employees who have High Deductible health plans. Reimburses employee for medical care expenses – for employee, spouse & dependents. Reimbursements up to maximum dollar amount with unused portion carried forward to subsequent coverage periods. HRA Benefits under HRA – generally excluded from employee’s gross income Qualifications for exclusion May only reimburse expenses for medical care as defined in IRC section 213(d) Expenses must be substantiated Expenses may not be for prior taxable year, incurred before date the HRA began, or before employee enrolled in HRA HRA Qualifications for exclusion No person may have right to receive cash or any benefit other than reimbursement of medical care expenses. If any person has such a right currently or in an future year, all distributions to all persons under HRA in current year are included in gross income (even amounts paid to reimburse medical care expenses). HRA Qualifications for exclusion Arrangements formally outside HRA that provide for adjustment of employee’s compensation will be considered in determining eligibility for exclusion. If bonus at retirement is related to HRA balance or severance is paid only to employees who have HRA balance, then all reimbursements for all participants are disqualified. HRA Qualifications for exclusion Reimbursements can be to former employees and retirees up to the unused balance. Employer may reduce maximum balance after retirement or termination for any administrative costs of continuing coverage. Employer may or may not provide an increase in amount available after an employee retires or terminates employment. If HRA allows payment of medical benefits to designated beneficiary other than the employee’s spouse or dependents payments are not excludable from income – effective 8/14/06 (delayed until 2009 for HRA provisions created before 8/14/06) HRA HRAs and Cafeteria Plans Employer contributions to an HRA may not be attributable to salary reductions or provided under a section 125 cafeteria plan to be excluded from taxable income Look at all circumstances in determination If salary reduction election for coverage period exceeds the actual cost of the accident or health plan coverage for that period, salary reduction is attributable to HRA – Look to COBRA rates for this. If correlation between maximum reimbursement amount available and amount of salary reduction election for accident and health plan then reduction is attributable to HRA HRA HRAs and Flexible Spending Accounts (FSAs) Amount credited to HRA must not be directly or indirectly based on amount forfeited under FSA If medical expenses are reimbursable under HRA and FSA, HRA must be exhausted before FSA Before FSA plan year begins, the plan document can specify coverage under HRA is available only after amount under FSA has been exhausted. In no case can HRA and FSA reimburse the same medical care expenses. HRA Nondiscrimination rules applicable to HRAs Section 105(h) same as for self-insured medical reimbursement plans HRA is subject to COBRA If individual elects COBRA continuation coverage HRA must provide for continuation of maximum reimbursement with increase at same time and same increment as similarly situated non-COBRA beneficiaries Plan can provide for continued reimbursement regardless of election of continuation coverage (not mandatory) No Reporting Requirement for HRA. Health Savings Accounts (HSA) Created by the Medicare Prescription Drug Improvement and Modernization Act of 2003 Effective for Taxable years beginning after 12/31/03 Tax-exempt trust or custodial account created exclusively to pay for qualified medical expenses of the account holder (employee) and his or her spouse and dependents. Subject to rules similar to those for IRAs HSA Qualifications for exclusion Individuals must be only in high deductible health plan (HDHP) Annual deductible for 2009 must be at least $1,150 for individual coverage and $2,300 for family coverage with out of pocket expense limits no more than $5,800 for individual coverage and $11,600 for family coverage. If family coverage, no amounts are payable from HDHP until the family has incurred medical expenses in excess of minimum annual deductible. An HDHP can have a smaller deductible or none at all for preventive care. HSA Qualifications for exclusion cont’d The insurance can be a PPO or POS – in which case the annual out-of-pocket limit is determined by services within the network. HSA Contributions Contributions can be made by the employer and employee – All contributions are aggregated for purposes of maximum contribution limit. Contributions to Archer MSAs reduce the limit available for HSA for tax exclusion Any amount over the limit is includable in gross income There is a 6% excise tax for excess individual and employer contributions in addition to all federal taxes. HSA Contributions Maximum annual contribution is the lesser of 100% of annual deductible Maximum deductible permitted same as Archer MSA For 2009 maximum is $3,000 for an individual and $5,950 for a family Catch up is allowed for individuals at least 55 years old on the last day of the tax year. For 2009 and beyond $1,000 HSA Contributions No contributions can be made once the individual is eligible or Medicare (65 years old). Amounts can be rolled over from an Archer MSA and IRA, or another HSA Employer contributions must be the same for everyone with comparable coverage either at the same amount or percent of deductible Comparability is applied separately to part-time workers (normally less than 39 hours per week). HSA HSA and HDHP can be included in a Cafeteria Plan HSAs are not subject to COBRA continuation coverage HSA Distributions Excluded from gross income if for qualified medical expenses of employee, spouse or dependents. If not used for qualified medical expenses then it is included in gross income and subject to additional 10% tax unless after death, disability, or the employee reaches 65 years old. HSA Distributions Qualified medical expenses Generally health insurance premiums are not qualified except: Qualified long term care insurance COBRA health care continuation coverage Health insurance premiums while the individual is receiving unemployment compensation benefits Individual over 65 for Medicare premiums and employer share of premium for employer provided health insurance Cannot use HSA funds to pay premiums for Medigap policies. HSA Distributions Employers are not required to determine whether HSA distributions are used for qualified medical expenses. Employee makes determinations and must maintain records to substantiate. Employers can provide eligible individuals with debit, credit or stored-value cards – same guidance as under HRAs HSA – Reporting Requirements Employer contributions and salary reductions contributions (pre-tax deductions) Employer contributions over limits Box 12W on W-2 Box 1,3, and 5 on W-2 with taxes in boxes 2, 4, and 6 Employee contributions not made by salary reduction Box 1, 3, and 5 on W-2 Employee can deduct up to the annual limit on personal tax return Sick Pay Paid by employer from regular payroll account Taxable as regular income Separate plan (STD, LTD) Premiums paid by employee on after tax basis – benefits are not taxable Premiums paid by employer or on pre-tax basis – benefits are fully taxable. Premiums paid by employer and employee (after-tax) – portion of benefits attributable to employer-funded portion is taxable. Sick Pay Responsibility for income withholding and employment taxes Employer pays and is self-insured Employer withholds taxes based on employee’s most recent W-4 Employer withholds and pays employer share of Social Security, Medicare, and FUTA taxes for all payments made within 6 calendar months after the end of the last month during which the employee worked. If employee returns to work, new six-month period begins if employee is later on disability Sick Pay Responsibility for income withholding and employment taxes Payments made by employer’s agent – employer is self insured. Agent may withhold FIT at 25% in 2009 Employer retains responsibility for Social Security, Medicare, and FUTA unless agreement with agent to take on this responsibility. Sick Pay Responsibility for income withholding and employment taxes Payments are made by an insurance company who receives premiums for disability coverage. Third party not required to withhold FIT from payments unless requested by disabled employee (W-4S) IRS allows for fixed amount or percentage (W-4S has no provision for percentage) Third party withholds and remits Social Security and Medicare taxes or advises employer who pays the taxes and includes in 941. Sick Pay Permanent Disability benefits Payments subject to income tax to extent premiums were paid by employer or with pre-tax dollars Payments are not subject to Social Security, Medicare, or FUTA Workers’ Compensation Insurance Form of insurance employers are required to buy to insulate them from lawsuits brought by employees who are hurt or become ill while working. Benefit payments – not included in gross income or subject to any employment taxes Premium payments – paid by employer based on specific earnings and classifications. Retirement and Deferred Compensation Plans Qualified Pension and Profit Sharing Plans IRC 401(a) Cash or Deferred Arrangements IRC 401(k) Tax-Sheltered Annuities IRC 403(b) Deferred Compensation Plans for Public Sector and Tax-Exempt Groups IRC 457 Employee-Funded Plans IRC 501(c)(18)(D) Individual Retirement Accounts (IRA) Retirement and Deferred Compensation Plans Simplified Employee Pensions IRC 408(k) Savings Incentive Match Plans for Employees of Small Employers (SIMPLE Plans) Employee Stock Ownership Plans Nonqualified Deferred Compensation Plans Qualified Pension and Profit Sharing Plans 401 (a) Defined Benefit Plans Benefit to employee based on age, compensation level and length of service Defined Contribution Plans Account for each employee, with set amount being contributed. Employee’s retirement benefit depends on the amount of money in the account at retirement. Qualified Pension and Profit Sharing Plans 401 (a) Defined Contribution Plans Money Purchase Pension Plan - Employer makes contributions each year based on employee’s compensation. Profit Sharing Plan – Employer contributions are substantial and recurring, although they may be discretionary to some degree Qualified Pension and Profit Sharing Plans 401 (a) Annual Compensation and Contribution Limits Set by Economic Growth and Tax Relief Reconciliation Act of 2001 (EGTRRA) For 2009 annual compensation limit is $245,000 (indexed annually to the next lowest multiple of $5,000). Annual contributions and other “additions” to defined contribution plans is limited under IRC 415 to the lesser of $49,000 in 2009 (indexed annually) or 100% of employee’s annual compensation. Pre-tax elective deferrals to 401(k), 403(b), 457, 125, 132(f)(4) are included in employee’s contribution to determine the limit. Qualified Pension and Profit Sharing Plans 401 (a) Tax Treatment of Pension and Profit Sharing Plans Qualified Plan – meets certain requirements under IRC 401(a) regarding participation, vesting, contribution limits, benefit limits, and nondiscrimination in favor of highly compensated employees. Employer contributions are excluded from wages and are not subject to federal income tax withholding, or Employment taxes. Employee after-tax contributions are included in income and taxable whether voluntary or required. Qualified Pension and Profit Sharing Plans 401 (a) State Tax Treatment of Pension Payments 1996 Law (HR394) prohibits states from imposing income tax on the “retirement income” of nonresidents. Cash or Deferred Arrangements (CODA) Voluntary Salary Reduction Plan – 401(k) Pension Protection Act of 2006 put ability to automatically enroll employees in 401(k) plan into the law for plan years starting after 12/31/07 Must provide specific schedule of automatic contribution. It must be at least 3% at hire and may stay at that level until the beginning of the second year after hire. Increases must be at least 1% each year up to 6% for fourth. The arrangement can specify larger percents up to 10% of compensation. If employer matches contributions, the plan must provide 100% match for first 1%; plus 50% for contributions between 2% and 6% or non-elective contribution of at least 3% of compensation – cannot contribute at high percent for highly compensated employees and cannot match contributions over 6%. When hired employees must have 90 days to withdraw from automatic elections and recover contributions from the plan. Employees can change or stop future contributions at any time. CODA Contribution Limits for 401(k) Tax Treatment of 401(k) contributions 2009 contribution limit is $16,500 Adjusted for inflation in $500 increments for future years Not taxable for Federal Income Tax (an most states) Taxable for Employment Taxes Reporting for 401(k) contributions on W-2 Not in box 1, but in boxes 3 & 5 In box 12 with a “D” Retirement box is checked in there were any deductions in the tax year. CODA “Catch-up” contribution began in 2002 Under EGTRRA – Applies to plans 401(k), 403(b), SEP, Simple, and 457 plans Employee must be at least 50 years old in the current year Limits of “catch-up” for all but SIMPLE 2009 catch-up limit is $5,500 Limit will be adjusted for inflation in $500 increments for future years SIMPLE “catch-up” limit is $2,500 in 2009. Limit will be adjusted for inflation in $500 increments for future years. CODA Non Discrimination Testing Must not discriminate in favor of highly compensated employees 5% owner of stock or capital Annual compensation over $110,000 (2009) or top paid 20% of employees Other Contributions can be included “Catch-up” Contributions are not counted. At least 70% of non-highly compensated employees must be eligible or the % of non-highly compensated eligible employees is at least 70% of the percentage of eligible highly compensated employees. CODA Non Discrimination Testing Other ways to meet non-discrimination testing Employer matches 100% of elective deferrals for not highly compensative employees up to 3% and 50% up to 5% Employer is required to contribute at least 3% of salary for non highly compensated employees regardless of the employee’s participation in 401(k) CODA Failure of ADP (Actual Deferral Percentage) Test Must distribute some elective deferrals and earnings to highly compensated employees within certain period and report on 1099-R CODA Holding period for 401k contributions In 1996 the Labor Dept. shortened the maximum holding period for 401(k) contributions from 90 days to the 15th business day of the month following the month during which the amount would have been paid to the employee. Employers who cannot meet the deadline can have an extra 10 business days, but must provide reasons for the delay. CODA Early Distribution Penalty If employee receives a distribution before retirement (with exceptions) there is a 10% excise tax on the taxable portion of the distribution. Veterans can make deferrals for years spent in military service Extra deferrals can be made for up to three times the period of military service (not to exceed 5 years) Separate reporting requirements Not included in non-discrimination tests. Roth 401(k) Starting in 2006 employers may permit employees to designate some or all of the contributions as Roth 401(k) The contributions are made with after-tax dollars. The earnings from the eventual distribution will be tax exempt. All 401(k) contributions (both pre-tax and Roth) are taken into account for limits and antidiscrimination testing. Roth 401(k) Reporting of Roth 401(k) on W-2 The amount contributed in boxes 1, 3 & 5. The amount contributed in box 12 with “AA” Tax-Shelter Annuities 403(b) Who can offer Public Schools, Tax Exempt Charitable, Religious, and Educational Organizations Automatic salary reductions Can qualify as elective deferrals Newly hired employee, who does not make an election can have automatic 4% deductions toward purchase of annuity. At hire employee must receive notice of auto election and right to elect to change the amount or opt out altogether. Every year employee notified of reduction percentage and their right to change it, including procedure and timing for doing so. 403(b) Requirements Annuity contract may not be purchased through a qualified annuity plan under Section 403(a) Employee’s rights must be non-forfeitable unless employee fails to pay premiums Plan (other than church plan) must meet non-discrimination requirements. Plan must offer all employees the chance to defer at least $200 annually if one employee is given the opportunity. The elective deferral limits must be met if plan provides for salary reduction agreement. 403(b) Requirements and Taxability Has many of the same requirements as 401(k) Employer contributions (e.g. match) are not included in wages or subject to withholding Employee contributions are not Taxable for Federal Income Tax and most state income taxes. Employee contributions are Taxable for employment taxes 403(b) Reporting on W-2 Contributions not in box 1 but in boxes 3 & 5. Contributions also show in box 12 with an “E” Box 13 Retirement plan is checked if there are any contributions for the tax year Catch-up special rule For employees with as least 15 years of service with employer. 403(b) Catch-up special rule Amount of catch-up limited to the lesser of $3,000 additional contribution in any year (same as catch-up for those at least 50 years old) $15,000 reduced by any amounts contributed under this special provision in previous years. $5,000 x years of service less total elective deferrals from previous years. If eligible for both special and over 50 catch-up cannot go over $5,500 – first dollars considered under special rule. Deferred Compensation Plans for Public Sector and Tax-Exempt Groups (IRC 457) Who can Offer Eligibility Only individuals performing services for the employer are eligible (including independent contractors) Nondiscrimination Testing State and local government employers and tax-exempt organizations (other than churches) 457 plans can be discriminatory. Deferral Limits Same as 401(k) IRC 457 Catch-up Contributions – new in 2002 Special rule near retirement Same as 401(k) For last 3 years before normal retirement, maximum deferral is lesser of twice the normal deferral or the current year limit plus the limits from previous years, reduced by participant’s deferrals for those years. Cannot use both Catch-up and Special Rule IRC 457 Rules Funds and earnings in tax-exempt trust for exclusive benefit of employees and beneficiaries Funds must be transferred within 15 business days after the month when would have been paid to employees. Deferrals and earnings remain assets of the employer subject to employer’s general creditors IRC 457 Tax Treatment Not subject to federal income tax withholding Are subject to Social Security, Medicare, and FUTA as soon as there is no substantial risk of forfeiture of right to the benefit Reporting Not in Box 1 of W-2, but in Box 3 and 5 with Social Security and Medicare taxes in Boxes 4 and 6 respectively and in Box 12 preceded by Code “G.” Employer should not mark check box in Box 13 “Retirement plan” based on 457 deferrals IRC 457 Distributions – Changes made by Economic Growth and Tax Relief Reconciliation Act (EGTRRA) of 2001 No distributions before employee reaches age 70-1/2, separation from employment (retirement) or the employee faces an unforeseeable emergency. Plan may allow early distribution if total amount payable is no more than $5,000 and no amount has been deferred within 2 years of the distribution. Distributions are considered pension Entity distributing has responsibility for withholding and remitting income taxes Individual Retirement Accounts (IRAs) Employer sponsored IRA must be in writing and created for exclusive benefit of employees and beneficiaries. Contribution Limits 2009 $5,000 After 2009 adjusted for inflation to next multiple of $500 IRA Catch-up Provision Participant must be at least 50 by the end of the year. Can deduct an additional $1,000 in years 2009 and beyond. IRA Tax Treatment Contributions are deductible Reduced if employee or spouse is an active participant in a qualified retirement plan Amount of reduction is based on adjusted gross income. For 2009 the reduction begins for married employees filing a joint return at $89,000; single $55,000; married filing separately $00. Employee not active participant (but spouse is) reduction starts at $166,000 for 2009 (married filing joint return) Taxability for deduction totally eliminated at $10,000 over the above limits ($20,000 for joint filers beginning in 2007). Roth IRA Contributions Established by Taxpayer Relief Act of 1997 Contributions are Taxable –There are no phase-outs because of active plan participant status, but the amount allowed is reduced by an contributions by the individual to other IRAs for that year For 2009 the amount that can be contributed is phased out once individual’s adjusted gross income exceed $166,000 for joint filers or $105,000 for single filers in 2008 (adjusted annually for inflation). Contributions are completely phased out at $176,000 for joint filers and $120,000 for single filers. Roth IRA Employers can allow direct deposit of contributions No contribution allowed by employer Participation Voluntary No endorsement by employer allowed IRA sponsors publicize direct to employees Contributions are remitted to IRA sponsor Employer does not receive any kind or consideration. Roth IRA Distributions Distributions are not included in gross income If made no sooner than 5 years after first contribution and Made on or after age 59-1/2, death, disability, or used for a first time home purchase. Employee Stock Ownership (ESOP) Defined Contribution Plan Stock bonus plan or combined stock bonus and money plan designed to invest primarily in the employer’s stock. Same general requirements as IRC 401(a) ESOP Tax Treatment Employer contributions are not wages and not subject to federal income tax withholding, Social Security, Medicare, or FUTA. Limit 200p – lesser of $49,000 or 100% of compensation. Nonqualified Deferred Compensation Plans Employer plan to defer compensation to a later date, which may or may not coincide with retirement. Plan does not meet requirements of 401(a) No limits Can be discriminatory Nonqualified Deferred Compensation Plans Tax Treatment The majority of these plans are unfunded – employee has only employer’s promise; the funds are not protected from the employer’s creditors or successors. When unfunded, the amounts are not subject to federal income tax, but are subject to Social Security, Medicare, and FUTA. When distributions are made later, the deferrals and the subsequent interest are subject to federal income tax, but not Social Security, Medicare, or FUTA Nonqualified Deferred Compensation Plans Requirements Written plan Employee has a legally binding right to compensation that has not been actually or constructively received and that is payable in a later year. Nonqualified Deferred Compensation Plans Reporting Requirements Amounts deferred into unfunded plan are reported in Box 3 and 5 Such deferrals are reported in Box 11, but only if they are for prior year services. Amounts distributed are reported in Box 1 only The amounts should be reported in Box 11, if there were no deferrals in the year of distribution. Family and Medical Leave Act (FMLA) Guarantees employees (in workplaces with 50 or more employees) unpaid leave in a 12month period for specific reasons. Employer decides what constitutes a 12-month period. If employer fails to make decision clear, the 12-month period applied is the one most favorable to the employee. FMLA – Reasons for FMLA 12 weeks in a 12 month period To be with a newborn or newly adopted child To take care of a seriously ill child, spouse, or parent. To care for themselves if they are seriously ill. Any qualifying exigency (i.e. need) arising out of the fact that the employee’s spouse, son, daughter, or parent is a covered military member on active duty or has been notified of an impending call to active duty in support of a contingency operations. FMLA – Reasons for FMLA 26 weeks in a “single12 month period” To care for military service member with serious injury or illness suffered in the line of duty if the employee is the employee is spouse, son, daughter, parent, or next of kin of covered service member. If employee does not take full 26 weeks remainder is forfeited. No more than 26 weeks can be taken even if there is another reason during the 12 month period beginning on the first day the employee takes leave. FMLA - Eligibility Has been employed by employer for at least 12 months (not necessarily consecutively) And has worked at least 1,250 hours within the previous 12-month period. Exempt employees who have been employed one year are deemed to meet the hours worked requirement unless employer can prove otherwise (A part time exempt employee scheduled to work less than 24 hours per week). FMLA – Paid vs. Unpaid Leave Employers can require eligible employees to use any paid leave as part of guaranteed leave. Employer must designate time off as paid or unpaid FMLA within 2 business days of receiving notice. FMLA – Notice Requirement Employee must give employer 30 days notice If not foreseeable – whatever notice is possible under the circumstances. If foreseeable and not notified, employer can deny leave request for up to 30 days after notice is provided. FMLA – Notice Requirement Employer must advise eligibility within 5 days of notice or when employer becomes aware that employee may qualify for FMLA If employee is not eligible the employer must give at least one reason for the denial Employer must provide separate notice as the same time of FMLA rights including How 12 month period was determined Certification Requirements Requirement to take paid leave Premium payment requirements for health benefits Job Restoration rights including effect of “key employee” designation Potential liability for health insurance premiums if employee does not return to work FMLA – Job Guarantee Upon return employee is entitled to previous job or “equivalent” with no loss of pay or benefits. Employee is not entitled to accrue any benefits or seniority during an unpaid FMLA leave Any benefit increases or improvements not dependent on seniority must be made effective upon return FMLA time must be treated as continuous service under pension and retirement plans for vesting and qualification purposes. Intermittent FMLA Several Days Working reduced hours If reduced hours, employer can deduct from exempt employee’s salary without converting employee to non-exempt under FLSA FMLA – Loophole and Recordkeeping Coverage Loophole The law requires employers to allow leave if there are 50 employees employed by the employer within 75 miles of the employee’s worksite when leave is requested. Recordkeeping requirements Basic payroll records regarding hours worked, rate of pay, deductions, details of dates and amounts of FMLA leave taken; copies of notices and documents related to FMLA leave. FMLA/Health Insurance FMLA guarantees continuation of employee’s health benefits while on leave. Employer can require employee’s premiums Can be paid before, during or upon return Pre-paid cannot be only option Catch-up can be sole option only if it is the only option offered to employees on unpaid non-FMLA leave. If during leave, payments are missed, the employee can be dropped after 30 days. Notice must be provided to employee and 15 days allowed before coverage is dropped. FMLA/Medical Flexible Spending Offered under Cafeteria Plan Employees must be allowed to: Continue coverage including health FSA while on FMLA leave Revoke coverage or to continue coverage but discontinue paying premiums during the leave. Reinstate health FSA coverage upon returning to work from unpaid FMLA leave Employer can require reinstatement if required of employees on unpaid non-FMLA leave. FMLA/COBRA Qualifying event is deemed to occur on the last day of FMLA leave if employee terminates employment at the end of FMLA leave. Maximum continuation coverage period is measured from that date or the date coverage is lost whichever is later. FMLA – Key Employees Employer may deny reinstatement to “key employees” if necessary to prevent “substantial and grievous” economic injury to the employer’s operations. Key Employee Salaried person among the highest 10% of all employees within 75 miles of the employee’s worksite. Employee must be informed of possibility upon request and must be notified in writing (in person or certified mail) as soon as the determination is made within 5 days of request for leave. Cafeteria Plans Specific type of flexible benefit plan authorized by Section 125 of the Internal Revenue Code Must contain at least one Taxable (cash) and one Non-Taxable (qualified) benefit. Participation must be restricted to employees and must be maintained for their benefit. Cafeteria Plans Examples of Qualified Benefits Accident and health insurance plans Dependent care assistance Group-term life insurance Qualified adoption assistance Cafeteria Plans Funding Flex Dollars or Flex Credits Salary Reduction Prohibition – Deferred Compensation Carry over unused contributions or benefits from one plan year to another. Use contributions from one plan year to purchase benefits employer will provide in later plan year. Cafeteria Plan Requirements Written Permanent Plan Description of benefits and period of coverage Plan’s rules for eligibility Procedures for elections Manner in which contributions are made Maximum amount of employer contributions available to any participant Definition of plan year Cafeteria Plans – Qualifying Event Change in status that allows employee to revoke or change an election during plan year Marital status Change in number of dependents Employment status change – employee or spouse Change in dependent status Residence change – employee, spouse or dependent Adoption Cafeteria Plans – Qualifying Event Cost-driven change that allows change in election during plan year Cost of qualified benefits increases or decreases New benefit option Dependent Care - cost change imposed by nonrelative care provider Spouse change – different enrollment period or change in cost of benefits available to spouse Cafeteria Plans – Changes to 401(k) Elections Cafeteria plan may permit an employee to change or revoke election deferrals to 401(k) plans or employee contributions governed by 401(m). The election revocation restrictions of Section 125 to not apply to these plans. Cafeteria Plans – Non-Discrimination Testing Non-discrimination Testing Plan must not discriminate in terms of eligibility, contributions, or benefits in favor of highly compensated individuals, participants, or key employees. Cafeteria Plans – Non-Discrimination Testing Non-discrimination Testing Eligibility Eligibility must not exceed 3 years Length of service requirement must be the same for all employees Contributions and benefits test Each participant must have an equal opportunity to select non-taxable benefits Highly compensated participants must not disproportionately select non-taxable benefits. Tax Treatment of Cafeteria Plans Employer contributions or pre-tax contributions are not subject to federal withholding or employment taxes to the extent that they are used to purchase nontaxable benefits. After-tax contributions toward benefits are fully taxable – the benefits purchased are excluded from employee’s income. Cash – if employee chooses cash, it is fully taxable. Tax Treatment of Cafeteria Plans Discriminatory plans No negative tax consequences to non-key employees Key employees have taxable income equal to the highest amount of taxable benefits they could have selected. Flexible Spending Arrangements (FSAs) Can be offered as part of a cafeteria plan Coverage requirements Specified expenses incurred by employees subject to maximums and other reasonable conditions. Maximum reimbursement amounts cannot be more than five times the total premium for employee’s coverage (life, health, dental, vision). Health Care FSA Elections must be made before year begins Cannot allow compensation to be deferred beyond the plan year or used for another benefit. Excess premiums in health FSA that exceed all reimbursements of claims and administrative costs can be used to reduce employees’ required premiums as a dividend or premium refund. Must be allocated on uniform basis. Starting in 2006 employers can allow a 2-1/2 month grace period for employees to spend money in their FSA – this will affect employees ability to elect HSA Health Care FSA Maximum amount of reimbursement selected by participant must be available at all times during the plan year. Amount available is reduced by reimbursement claims The premium payment schedule cannot be accelerated because of claims or employee separation from employment. Health Care FSA Reimbursements Medical FSAs can only reimburse medical expenses incurred during coverage period – cannot reimburse premiums Medical expenses must be substantiated by third party and a statement from employee that the expense is not reimbursable under any other coverage is required. Reimbursements can only be made for expenses actually incurred during period of coverage – when medical care if provided. Dependent Care FSA Not subject to uniform coverage rule – reimbursements are only made up to the amount already deducted. Employees can be reimbursed up to $5,000 of dependent care expenses. Employees must reduce any dependent care tax credit they receive dollar for dollar by any amounts contributed to Dependent FSA Amount deducted for Dependent FSA goes in Box 10 on the W-2 State Taxation Starting on page 4-126 – table of State Taxability Illinois Deferrals under Section 125 or 401 are not taxable for state income tax, though they are taxable for SUI Deductions used to purchase medical or life insurance are not taxable for state income tax or SUI.