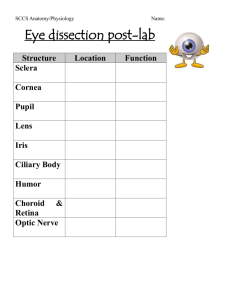
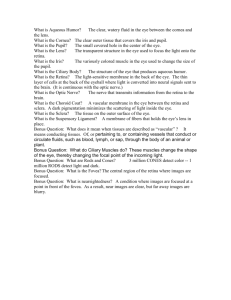
Ch16.Special.Senses.Part1
advertisement

SENSORY RECEPTORS & THE SPECIAL SENSES Leonardo Da Vinci, The Mona Lisa Human Anatomy Sonya Schuh-Huerta, Ph.D. Peripheral Sensory Receptors • 2 main categories of sensory receptors – Free nerve endings of sensory neurons • Monitor general sensory information – Complete receptor cells specialized epithelial cells or small neurons • Monitor most types of special sensory information Peripheral Sensory Receptors • Sensory receptors also classified according to: – Location – Type of stimulus detected – Structure Classification by Stimulus Detected • Mechanoreceptors respond to mechanical forces – Touch, pressure, stretch, vibration, & itch – Baroreceptors monitor blood pressure (detect pressure/stretch in walls of vessels) • Thermoreceptors respond to temperature changes (heat/cold) Classification by Stimulus Detected • Chemoreceptors – Respond to chemicals in solution • Photoreceptors respond to light – Located in the eye • Nociceptors – Respond to harmful stimuli that result in pain Classification by Location • Exteroceptors sensitive to stimuli arising from outside the body – Located at or near body surfaces – Include receptors for touch, pressure, pain, & temperature Classification by Location • Interoceptors receive stimuli from internal viscera – Located in digestive tube, bladder, & lungs – Monitor a variety of stimuli • • • • Changes in chemical concentration Taste stimuli Stretching of tissues Temperature Classification by Structure • General sensory receptors – Widely distributed – Nerve endings of sensory neurons monitor: • • • • • • • Touch Pressure Vibration Stretch Pain Temperature Proprioception Classification by Structure • General sensory receptors are: – Divided into 2 groups • Free nerve endings • Encapsulated nerve endings Free Nerve Endings • Abundant in epithelia & underlying CT • Respond to pain & temperature (several types) Free Nerve Endings • 2 other specialized types of free nerve endings – Merkel discs (= Epithelial tactile complexes) • Consist of tactile epithelial cell innervated by sensory nerve ending • Slowly-adapting receptors for light touch – Hair follicle receptors wrap around hair follicles • Detect hair-deflection/pulling • Rapidly-adapting receptors General Sensory Receptors – Unencapsulated (Free) Encapsulated Nerve Endings • Consist of 1 or more end fibers of sensory neurons enclosed in connective tissue • Mechanoreceptors – Include 4 main types: • • • • Tactile (Meissner’s) corpuscles Pacinian (Lamellar) corpuscles Bulbous corpuscles (Ruffini endings) Proprioceptors Encapsulated Nerve Endings • Tactile (Meissner’s) corpuscles – Spiraling nerve ending surrounded by Schwann cells – Occur in the dermal papillae remember this? – Rapidly-adapting receptors for discriminative touch (also light pressure, low freq vibration) – Occur in sensitive, hairless areas of the skin General Sensory Receptors Tactile corpuscle (touch, light pressure) Epithelial tactile complexes (light touch) Free nerve endings (pain and temperature) Epidermis We’ll view under the microscope Dermis and hypodermis Lamellar corpuscle (deep pressure) Bulbous corpuscle (pressure) Hair follicle receptor (hair movement) Encapsulated Nerve Endings • Pacinian (Lamellar) Corpuscles – Single nerve ending surrounded by layers of flattened Schwann cells – Occur in the dermis, hypodermis, & CTs, joints, etc. – Sensitive to deep pressure rapidlyadapting receptors General Sensory Receptors Tactile corpuscle (touch, light pressure) Epithelial tactile complexes (light touch) Free nerve endings (pain and temperature) Epidermis We’ll also view these under the microscope Dermis and hypodermis Lamellar corpuscle (deep pressure) Bulbous corpuscle (pressure) Hair follicle receptor (hair movement) Encapsulated Nerve Endings • Bulbous Corpuscles (= Ruffini endings) – Located in the dermis, hypodermis & joints – Monitor continuous pressure on the skin adapt slowly General Sensory Receptors Tactile corpuscle (touch, light pressure) Epithelial tactile complexes (light touch) Free nerve endings (pain and temperature) Epidermis Dermis and hypodermis Lamellar corpuscle (deep pressure) Bulbous corpuscle (pressure) Hair follicle receptor (hair movement) General Sensory Receptors – Encapsulated Encapsulated Nerve Endings • Proprioceptors – Monitor stretch in locomotory organs muscles, tendons, joints, & ligaments – Send inputs on body movement to the CNS – 3 types of proprioceptors 3 Types of Proprioceptors • Muscle spindles measure the changing length of a muscle (=muscle stretch) – Imbedded in the perimysium between muscle fascicles • Golgi tendon organs located near the muscle-tendon junction – Monitor tension within tendons (= tendon stretch) • Joint kinesthetic receptors – Sensory nerve endings within joint capsules – Monitor stretch & pain/nociception Structure of Proprioceptors Secondary sensory endings (type II fiber) Efferent (motor) fiber to muscle spindle Efferent Primary sensory endings (type Ia fiber) (motor) fiber to extrafusal muscle fibers Extrafusal muscle fiber Muscle spindle Connective tissue capsule Intrafusal muscle fibers Sensory fiber Golgi Tendon organ Tendon General Sensory Receptors – Proprioceptors The Special Senses (Ch 16) The Special Senses! • Sight, hearing, balance, taste, & smell • Special sensory receptors: – Localized confined to the head region – Receptors are not free endings of sensory neurons – Special receptor cells! • Neuron-like epithelial cells or small peripheral neurons – Transfer sensory information to other neurons in afferent pathways that lead to the brain The Eye & Vision • Visual organ the eye – 70% of all of the body’s sensory receptors are in the eyes – 40% of the cerebral cortex is involved in processing visual information! – Only 1/6 of the eye’s surface is visible Accessory Structures of the Eye • Eyebrows coarse hairs on the superciliary arches • Eyelids (palpebrae) separated by the palpebral fissure – Meet at the medial & lateral angles (canthi) – Lacrimal caruncle reddish elevation at the medial canthus – Tarsal plates connective tissue within the eyelids – Tarsal glands modified sebaceous glands Accessory Structures of the Eye • Conjunctiva = transparent mucous membrane Levator palpebrae superioris muscle Orbicularis oculi muscle Eyebrow Tarsal plate Palpebral conjunctiva Tarsal glands Cornea Palpebral fissure Eyelashes Bulbar conjunctiva Conjunctival sac Orbicularis oculi muscle (b) Lateral view; some structures shown in sagittal section Accessory Structures of the Eye • Lacrimal apparatus keeps the surface of the eye moist – Lacrimal gland produces lacrimal fluid – Lacrimal sac fluid empties into nasal cavity – Can you see why, when you cry you get a leaky nose?... Lacrimal sac Lacrimal gland Excretory ducts of lacrimal glands Lacrimal punctum Lacrimal canaliculus Nasolacrimal duct Inferior meatus of nasal cavity Nostril Extrinsic Eye Muscles • 6 muscles that control movement of eye – Originate in the walls of the orbit – Insert on outer surface of the eyeball • The 6 extrinsic eye muscles are: – Lateral rectus & medial rectus – Superior rectus & inferior rectus – Superior oblique & inferior oblique – Yes, you have to know them all Extrinsic Eye Muscles Superior oblique muscle Trochlea Trochlea Superior oblique tendon Superior rectus Superior rectus muscle Lateral rectus Superior oblique Medial rectus Lateral rectus muscle Inferior oblique Common tendinous ring Inferior rectus muscle Inferior oblique muscle (a) Lateral view of the right eye (b) Anterior view of the right eye Inferior rectus Summary of Muscle Actions Muscle Lateral rectus Medial rectus Superior rectus Inferior rectus Inferior oblique Superior oblique Action Controlling cranial nerve Moves eye laterally Moves eye medially Elevates eye and turns it medially Depresses eye and turns it medially Elevates eye and turns it laterally Depresses eye and turns it laterally VI (abducens) III (oculomotor) III (oculomotor) III (oculomotor) III (oculomotor) IV (trochlear) (c) Summary of muscle actions and innervating cranial nerves Anatomy of the Eyeball • Components of the eye – Protect & support the photoreceptors – Gather, focus, & process light into precise images • Anterior pole most anterior part of the eye • Posterior pole most posterior part of the eye • External walls composed of three tunics (= layers) • Internal cavity contains fluids (= humors) The Fibrous Layer • Most external layer of the eyeball – Composed of 2 regions of connective tissue • Sclera posterior 5/6 of the tunic – White, opaque region – Provides shape & an anchor for eye muscles • Cornea Anterior 1/6 of the fibrous tunic • Limbus junction between sclera & cornea • Scleral venous sinus allows aqueous humor to drain Medial View of the Eye Ora serrata Ciliary body Ciliary zonule (suspensory ligament) Cornea Iris Pupil Anterior pole Sclera Choroid Retina Macula lutea Fovea centralis Posterior pole Optic nerve Anterior segment (contains aqueous humor) Lens Scleral venous sinus Posterior segment (contains vitreous humor) Central artery and vein of the retina Optic disc (blind spot) (a) Diagrammatic view. The vitreous humor is illustrated only in the bottom part of the eyeball. The Vascular Layer • The middle coat of the eyeball • Composed of choroid, ciliary body, & iris • Choroid vascular, darkly pigmented membrane – Forms posterior 5/6 of the vascular tunic – Brown color from melanocytes – Prevents scattering of light rays within the eye • Choroid corresponds to the arachnoid & pia maters The Vascular Layer • Ciliary body thickened ring of tissue, which encircles the lens • Composed of ciliary muscle – Ciliary processes posterior surface of the ciliary body – Ciliary zonule (= suspensory ligament) • Attached around entire circumference of the lens • Suspend the lens & allow it to change shape when focusing on near & far objects Medial View of the Eye Ora serrata Ciliary body Sclera Ciliary zonule (suspensory ligament) Choroid Retina Macula lutea Cornea Iris Fovea centralis Pupil Posterior pole Anterior pole Optic nerve Anterior segment (contains aqueous humor) Lens Scleral venous sinus Central artery and vein of the retina Posterior segment (contains vitreous humor) Optic disc (blind spot) (a) Diagrammatic view. The vitreous humor is illustrated only in the bottom part of the eyeball. The Iris • Visible colored part of the eye –several genes code for its color! • Attached to the ciliary body • Composed of smooth muscle • Pupil the round, central opening in iris – Sphincter pupillae muscle – Dilator pupillae muscle • Act to vary the size of the pupil – Pupillary light reflex • Protective response pupil constriction when a bright light is flashed in the eye or you go out into direct sunlight The Inner Layer (Retina) • Retina the deepest tunic • Composed of 2 layers – Pigmented layer single layer of melanocytes – Neural layer sheet of nervous tissue • Contains 3 main types of neurons: – Photoreceptor cells – Bipolar cells – Ganglion cells Microscopic Anatomy of the Retina Photoreceptors Ganglion cells Bipolar cells Rod Cone Nuclei of ganglion cells Outer segments of rods and cones Choroid Amacrine cell Horizontal cell Pathway of signal output Pathway of light Pigmented layer of retina (b) Cells of the neural layer of the retina Axons of ganglion cells Nuclei Nuclei of of bipolar rods and cells cones (c) Photomicrograph of retina Pigmented layer of retina The Retina • Photoreceptor cells activate bipolar cells • Bipolar cells activate ganglion cells to generate nerve impulses • Axons from ganglion cells run along internal surface of the retina – Converge posteriorly to form the optic nerve Posterior Aspect of the Eyeball Neural layer of retina Pigmented layer of retina Pathway of light Choroid Sclera Optic disc Central artery and vein of retina Optic nerve (a) Posterior aspect of the eyeball Photoreceptors • 2 main types – Rod cells more sensitive to light • Allow vision in dim light (black & white) – Cone cells operate best in bright light • Enable high-acuity, color vision • Considered neurons! Photoreceptors • Rods & cones have an inner & outer segment – Outer segments are receptor regions • Light absorbing pigments are present • Are continuously shed & replaced over time • Light particles (photons) modify the visual pigment, which causes a change in the flow of ions in/out of the cell, & generates a nerve impulse in the photoreceptor Photoreceptors Process of bipolar cell Synaptic terminals Inner fibers Mitochondria Outer fiber Connecting cilia Outer segment Inner segment – rhodopsin (in rods) – 3 opsins in cones detect green, red, blue – primates are trichromats what does this mean? Nuclei Cone cell body Pigmented layer • Visual pigments in the rods & cones that allow you to see: Rod cell body Rod cell body Apical microvillus Discs containing visual pigments Discs being phagocytized Melanin granules Pigment cell nucleus Basal lamina (border with choroid) Photoreceptors • Photoreceptors – Vulnerable to damage by light or heat – Cannot regenerate if destroyed – But continuously renew & replace their outer segments – Look closely at the retina where exactly are the photoreceptors (which layer of cells are they?) Regional Specializations of the Retina • Ora serrata retinae – Neural layer ends at the posterior margin of the ciliary body – Pigmented layer covers ciliary body & posterior surface of the iris • Macula lutea contains mostly cones • Fovea centralis contains only cones – Region of highest visual acuity!!! • Optic disc where optic nerve emerges from retina – blind spot! Medial View of the Eye Ora serrata Ciliary body Sclera Ciliary zonule (suspensory ligament) Choroid Cornea Iris Pupil Fovea centralis Anterior pole Optic nerve Retina Macula lutea Posterior pole Anterior segment (contains aqueous humor) Lens Scleral venous sinus Central artery and vein of the retina Posterior segment (contains vitreous humor) Optic disc (blind spot) (a) Diagrammatic view. The vitreous humor is illustrated only in the bottom part of the eyeball. Blood Supply of the Retina • Retina receives blood from 2 sources – Outer 1/3 of the retina supplied by capillaries in the choroid – Inner 2/3 of the retina supplied by central artery & vein of the retina Central artery and vein emerging from the optic disc Macula lutea Optic disc Retina Internal Chambers & Fluids • The lens & ciliary zonules divide eye • Posterior segment (cavity) – Filled with vitreous humor • • • • Clear, jelly-like substance Transmits light Supports the posterior surface of the lens Helps maintain intraocular pressure Internal Chambers & Fluids • Anterior segment – Divided into anterior & posterior chambers • Anterior chamber between the cornea & iris • Posterior chamber between the iris & lens • Filled with aqueous humor – Renewed continuously – Formed as a blood filtrate – Supplies nutrients to the lens & cornea Internal Chambers & Fluids Cornea Lens Posterior segment (contains vitreous humor) Iris Lens epithelium Lens Cornea 2 Corneal epithelium Corneal endothelium Aqueous humor Anterior chamber 1 Aqueous humor is formed by filtration from the capillaries in the ciliary processes. 2 Aqueous humor flows from the posterior chamber through the pupil into the anterior chamber. Some also flows through the vitreous humor (not shown). Anterior segment Posterior chamber (contains aqueous humor) Ciliary zonule (suspensory ligament) 3 Scleral venous sinus Ciliary processes Corneoscleral junction Ciliary muscle Bulbar conjunctiva Sclera 3 Aqueous humor is reabsorbed into the venous blood by the scleral venous sinus. 1 Ciliary body The Lens • A thick, transparent, biconvex disc – Held in place by its ciliary zonule • Lens epithelium covers anterior surface of the lens • Lens fibers form the bulk of the lens – New lens fibers are continuously added – Lens enlarges throughout life The Eye as an Optical Device • Structures in the eye bend light rays • Light rays converge on the retina at a single focal point • Light bending structures (refractory media) are: – lens, cornea, & humors • Accommodation curvature of the lens is adjustable – Allows for focusing on nearby objects The Eye as an Optical Device Sympathetic activation Nearly parallel rays from distant object Lens Ciliary zonule Ciliary muscle Inverted image (a) Lens is flattened for distant vision. Sympathetic input relaxes the ciliary muscle, tightening the ciliary zonule, and flattening the lens. Parasympathetic activation Divergent rays from close object Inverted image (b) Lens bulges for close vision. Parasympathetic input contracts the ciliary muscle, loosening the ciliary zonule, allowing the lens to bulge. The Eye as an Optical Device Myopic eye (nearsighted) Hyperopic eye (farsighted) Focal point Eyeball too long Uncorrected Focal point is in front of retina. Corrected Concave lens moves focal point further back. Eyeball too short Uncorrected Focal point is behind retina. Corrected Convex lens moves focal point forward. Visual Pathways • Most visual information travels to the cerebral cortex • Responsible for conscious “seeing” • Other pathways travel to nuclei in the midbrain & diencephalon Visual Pathways to the Cerebral Cortex • Pathway begins at the retina – Light activates photoreceptors – Photoreceptors signal bipolar cells – Bipolar cells signal ganglion cells – Axons of ganglion cells exit the eye in the optic nerve – Some axons cross over to the opposite side of the brain – they run through the optic chiasma (remember this?) Visual Pathways to the Cerebral Cortex • Then optic tracts send axons to: – Lateral geniculate nucleus of the thalamus • Synapse with thalamic neurons • Fibers of the optic radiation reach the primary visual cortex Visual Fields & Visual Pathways to the Brain Both eyes Fixation point Right eye Left eye Optic nerve Suprachiasmatic nucleus Pretectal nucleus Lateral geniculate nucleus of thalamus Optic chiasma Optic tract Uncrossed (ipsilateral) fiber Crossed (contralateral) fiber Optic radiation Occipital lobe (primary visual cortex) (a) The visual fields of the two eyes overlap considerably. Note that fibers from the lateral portion of each retinal field do not cross at the optic chiasma. Superior colliculus Visual Pathways to Other Parts of the Brain • Some axons from the optic tracts – Branch to midbrain • Superior colliculi (remember this on the brain?) • Pretectal nuclei Disorders of the Eye & Vision • Age-related macular degeneration (AMD) – The macula begins to degenerate or lift off retina – Involves the build-up of visual pigments in retina – Blurred vision to blindness • Retinopathy of prematurity – Blood vessels grow within the eyes of premature infants – Vessels have weak walls cause hemorrhaging & blindness • Trachoma contagious infection of the conjunctiva • Blindness – Congenital or acquired; Causes: cataracts, glaucoma, AMD, corneal opacity, diabetic retinopathy, childhood blindness, trachoma, etc. Questions…? What’s Next? Lab: PNS & Special Senses Histology & Eye Models Mon Lecture: Special Senses II Mon Lab: Cow Eye Dissection!