Diet Order Storyboards and Use Cases
advertisement

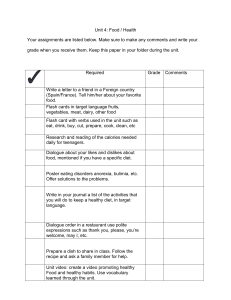
HL7 Version 3 Diet Orders Domain Analysis Model Use Cases and Storyboards Draft v 1.1 05/14/2011 Authors: Members of American Dietetic Association Nutrition Informatics Committee: Elaine Ayres Joan Hoppe Bill Swan Curt Calder Amy Miller Anne Lougher Margaret Dittloff Marty Yadrick Mary Jane Rogalski Lindsey Hoggle Jessie Pavlinac Nisha Jain Trudy Euler 1 Table of Contents Introduction ................................................................................................................................................ 4 Storyboard Sample Format ......................................................................................................................... 7 Storyboard Topic ..................................................................................................................................... 7 Storyboard Actors and Roles .................................................................................................................. 7 Pre-Condition .......................................................................................................................................... 7 Sequence of Events, Storyboard, Activities ............................................................................................ 7 Post Condition ......................................................................................................................................... 7 Diet Order Storyboards and Use Cases ....................................................................................................... 8 Use Case 1: Order New Diet—General/Healthful (unrestricted) Diet .................................................... 8 Use Case 2: Order New Diet with Quantitative, Nutrient-based Modifications .................................. 11 Use Case 3: Texture/Consistency Modifications ................................................................................. 13 Use Case 4: Diet Order change to ‘NPO for Tests’ ................................................................................ 15 Use Case 5: Pediatric Specialty Orders – NEED TO DOCUMENT .......................................................... 17 Use Case 6: Order Oral Nutritional Supplement .................................................................................. 19 Use Case 7: Order Enteral Nutrition (Tube Feeding) ........................................................................... 22 Use Case 8: Meal/Special Service Designation Order .......................................................................... 26 Use Case 9: Request RD/Nutrition Consult .......................................................................................... 28 Glossary ..................................................................................................................................................... 37 References and Acronyms ........................................................................................................................ 39 Appendix: Storyboard naming standards ................................................................................................ 40 2 3 Introduction Computerized Food and Nutrition Service Management Systems (FNMS) used by dietetics and foodservice departments in hospitals and long-term care facilities depend on HL7 interfaces to exchange data with hospital information systems (HIS), electronic health records (EHR) and computerized physician order entry (CPOE) systems. The core function of these interfaces is the electronic transmission and exchange of medically-based diet orders, tube feeding and nutritional supplement orders, dietary intolerances and food allergies along with patient/resident food preference information required to provide inpatients with nutritionally/culturally appropriate meals. The orders interface capabilities of different FNMS varies by vendor; the majority support one-way, inbound messages while some may support bi-directional interfaces. The procedure for acknowledging nutrition orders also varies among institutions; for instance, in many institutions the order is verified by nursing prior to transmission to the FNMS. Diet and nutritional supplement orders are an important part of the medical nutrition therapy. This coded information is used by nutrition software systems to control and customize the foods that get offered and served to patients/residents as part of their plan of care. A hospital or long-term care facility Food & Nutrition Services department needs a diet order to notify them that a patient is able and allowed to eat. A diet order is comprised of one or more diet specifications (often called diet codes, modifications or restrictions). A patient can have only one effective diet order at a time. The composite list of diet specifications in a diet order indicate what foods a patient should or should not receive. This may involve controlling the type, texture and/or quantity of foods and nutrients that the patient should receive. Often a complete diet order consists of a single diet code, such as ‘General Healthy/Standard’ which is unrestricted in the amount or type of foods offered. Diet codes can govern foods in a number of ways. In some cases, such as a gluten-free diet or a diet code representing a food allergy, certain foods are contraindicated. In other cases, the diet implies a recommended amount of one or more nutrients. “Some diet codes can combine to make a single diet order. A 1500-Calorie restriction and a 2-gram sodium (NA2GM) restriction can coexist since they do not address the same nutrient.” Certain kinds of diet codes cannot be combined with other codes, such 4 as NPO (Nothing by mouth) or use of more than one code for a given quantity of a nutrient, e.g., 1500Calorie and 2000-Calorie. It is impossible to feed a patient at two different calorie levels at the same time. “These constraints are not defined in the table, but rather are implied by the semantics of the codes.”(Chapter 4: Order Entry Page 4-98 Health Level Seven, Version v2.5.1 © 2007.) A recognized standard or controlled vocabulary of diets or diet codes does not currently exist. Each hospital institution or group will define a list of diet codes for use at their facility. However, most localized diet descriptions or codes can be categorized as requiring either qualitative adjustments such as texture modifications to assist a patient with chewing or swallowing disorders; or quantitative modifications to control the amount of certain nutrients per day. Nutrient-based diets are ordered in amounts per 24 hours and may then be arbitrarily divided up among multiple meals and/or between meal snacks according to the patient’s typical eating behavior or the operational processes of each medical facility. A dietitian may recommend that a patient receive a nutritional supplement or protein sandwich between main meals to help the patient meet the daily nutrient totals for a diet. Suggested diet taxonomy (see appendix #) compiled by the Nutrition Care Process/Standardized Language Committee of the American Dietetic Association includes the following basic categories of diets: Oral Diets o General/Healthful (to include age-appropriate modifications, e.g., toddler) o Texture/Consistency Modified o Allergy/Intolerance – to eliminate or limit foods with specific ingredients i.e. gluten-free o Quantitative Nutrient-based Modifications Energy Modified Carbohydrate Modified Protein & Amino Acid Modified Fluid Modified (Restricting or limiting consumption of total fluids) Mineral Modified (sodium, potassium, phosphorus, etc.) Medical Nutritional Supplements o Ordered b y Generic Description of Product Formulation, e.g., High Protein/2.0 Kcal formula o Ordered by Specific Product/Manufacturer ID Enteral Nutrition (for tube feedings) Parenteral Nutrition (as these are generally pharmacy orders, they will not be addressed here) 5 Diets are typically ordered by a physician (or other licensed independent practitioner – LIP) or in some cases by a licensed dietitian/nutritionist with clinical privileges, delegated authority or per established protocols. Diet orders should designate a start time or meal for which the new diet order is to take effect. This start time may be a specific time (either now or in the future) or for a designated meal or snack period. Under certain circumstances, a diet order will have a specified end date/time or expiration time if it is part of transitional orders for diet progressions or required for certain medical procedures or tests. More often a diet order will have no end or stop date/time and will continue so the patient is fed until the order is cancelled, revised or a replaced by a new order. The intent of this document is to describe the diet and nutrition order storyboards, use cases and flow of information needed to model nutrition orders in HL7 version 3. 6 Storyboard Sample Format Storyboard Topic The purpose of the story board is to illustrate the communication flow and documentation of a . . . Storyboard Actors and Roles Triage Nurse Trauma Physician Etc. Pre-Condition To be inserted Sequence of Events, Storyboard, Activities To be inserted Post Condition To be inserted. 7 Diet Order Storyboards and Use Cases Use Case 1: Order New Diet—General/Healthful (unrestricted) Diet Use Case Description The purpose of this use case is to illustrate a physician or LIP ordering a diet in the patient record. This diet order information needs to be shared with other care providers and hospital departments which have specialized computer systems. Typically a physician will order a diet by selecting from a list of diet modification codes defined at each hospital facility. The addition of a diet order is the trigger event that will initiate meal service for a patient who is admitted to the hospital. The Food & Nutrition Services department needs a diet order to notify them that a patient is able and allowed to eat. The order should designate a start time or meal at which the new diet order is to take effect. This start time may be a specific time (now or in the future) or meal. Upon receipt of the diet order information, the Food & Nutrition Services operation will prepare and serve the patient diet-appropriate foods according to the facility’s meal service policies. A diet order may have an expiration or end point time such as a special diet needed for a specific test, but this is not common. Conditions This use case applies to the entry of any new diet order for a patient. The order should take effect at the designated start time or meal specified in the order and should remain in effect until it is cancelled, suspended, or superseded by a subsequent new diet order. Preconditions 1. The patient has been admitted to an inpatient nursing unit of an acute care hospital 2. Admission nutrition screening has already been completed on the patient 3. The acute care hospital uses an electronic health record (EHR) 4. The acute care hospital uses CPOE 5. The acute care hospital uses an electronic food and nutrition management system (FNMS) 6. The acute care hospital EHR and FNMS share information via HL7 interface, either one-way or bidirectional. 8 7. The licensed entity (LIC) registered nurse (or Healthcare Provider (PROV-RN)), registered dietitian or (Healthcare Provider (PROV-RD)) and the diet clerk all have access to the EHR. The diet clerk (DC) and the registered dietitian also have access to the FNMS. Actors/Roles Aaron Attending (Attending Physician - LIC/Author) Adam Everyman (Patient) Nancy Nightingale (Registered Nurse - PROV-RN) Connie Chow (Dietitian - PROV-RD) Diet Clerk (Need a name to assign) Foodservice Worker (Need a name to assign) Use Case Sequence of Steps 1. Physician enters an order into CPOE system for a new diet selecting ‘General/Healthful’ diet code for patient Adam Everyman that is to begin immediately. 2. The Diet Order is sent to Food & Nutrition Services via HL7-compliant interface to the department’s food & nutrition management software system (FNMS). 3. FNMS automatically acknowledges the new diet order electronically (e.g., sends an ACK message to the CPOE sending system) and the FNMS patient record for Adam Everyman is updated with the new diet order details. 4. Food & Nutrition department prepares a meal tray with foods appropriate for the ordered diet for the patient according to the facility’s meal service procedures, which may be at the next scheduled meal service or for on-demand hotel-style meal delivery. 5. Meal tray is delivered to the patient. Use Case Scenario Adam Everyman, a 40-year old male with a fractured femur, is admitted to room 234 of GHH Inpatient (orthopedic) Unit at Good Health Hospital at 16:30. Adam Everyman tells nurse Nancy Nightingale he is hungry and wants to know when he can eat. Dr. Aaron Attending assesses the patient and determines that he has no other medical conditions or complications at this time. Dr. Aaron Attending enters a new diet order for a ‘General/Healthful’ diet without any therapeutic modifications to start now (16:30) and to continue with no end date/time specified into the CPOE system of Good Health Hospital. The diet order information is electronically transmitted to the Nutrition Services department’s computerized food and nutrition management system (FNMS) which automatically 9 acknowledges receipt of the order transaction at 16:45 and updates the patient record for Adam Everyman matching the diet code for ‘General/Healthful’ diet and sets that start time of that diet order as of 16:30, which will allow Adam Everyman to receive a dinner meal tray. A diet clerk in the Nutrition Services department uses the FNMS to generate tray tickets for dinner. Foodservice trayline workers assemble a meal tray for Adam Everyman that includes food appropriate for General/Healthful dinner meal. Adam Everyman receives his dinner meal tray according to the department’s meal service delivery schedule. 10 Use Case 2: Order New Diet with Quantitative, Nutrient-based Modifications Use Case Description The purpose of this use case is to describe the flow of information that will initiate meal service for an admitted patient who requires a diet with multiple quantitative nutrient modifications such as that required for a diabetic patient undergoing renal dialysis treatment. • Example: 80 gm Protein + Consistent Carb + 2g Sodium + 2g Potassium + 800-1000 mg Phosphorus + 1500 mL Fluid Restricted Conditions This use case applies to the entry of any new diet order for a patient requiring one or more diet modifications that specify a quantity or range of a given nutrient. The order should take effect at the designated start time or meal specified in the order and should remain in effect until it is cancelled, suspended, or superseded by a subsequent new diet order. Preconditions Same as previously stated Actors/Roles Harold Hippocrates (Physician - Author) Eve Everywoman (Patient) Nancy Nightingale (PROV-RN) Connie Chow - Dietitian (PROV-RD) Diet Clerk Foodservice Worker Use Case Sequence of Steps 1. A patient with diabetes and chronic kidney disease (CKD) on dialysis (stage 5) is admitted to the hospital with edema. The patient weighed 72 kg at admission. 2. Registered Dietitian (RD) completes a nutritional assessment documenting the patient’s usual weight as 69 kg and a diet history that reveals that the patient’s typical food intake exceeds her recommended sodium, and potassium levels and her carbohydrate intake varies considerably contributing to uncontrolled blood glucose values. The RD calculates the patient’s protein needs given her dialysis treatments, e.g., 1.2 grams protein/kg body weight, and recommends a protein level diet of 80 gm protein/day. Protein level diets at Good Health Hospital are ordered in 10 gram 11 3. 4. 5. 6. 7. increments, e.g., 60 gm pro, 70 gm pro, 80 gm pro, etc. The RD documents her nutrition recommendations in the EHR. After reviewing the RD’s recommendations, the physician enters a new diet order for 80 gm protein + Consistent Carbohydrate + 2g sodium + 2g potassium + 800-1000mg Phosphorus + 1500 mL Fluid Restricted by selecting from the available diet codes in the CPOE system. The diet order is sent to Food is sent to Food & Nutrition Services via HL7-compliant interface to the department’s FNMS. FNMS automatically acknowledges the new diet order electronically (e.g., sends an ACK message to the CPOE sending system) and the FNMS inserts the new diet order details into the existing admission record patient record for Eve Everywoman. Food & Nutrition department prepares a meal tray with appropriate foods to ensure that nutrients are within the prescribed quantities for the patient served according to the facility’s meal service operation procedures. Meal tray is delivered to the patient. Use Case Scenario Eve Everywoman, a patient with diabetes and chronic kidney disease requiring dialysis is admitted to the hospital with an infection and edema. Eve’s usual weight is 69 kg and her admit weight was recorded as 70.5 kg. Connie Chow, the registered dietitian, completes a nutritional assessment for Eve including a diet history that reveals Eve has been eating foods high sodium and potassium while not controlling her carbohydrate intake. Connie documents her assessment findings and nutrition prescription recommendations in the EHR. 12 Use Case 3: Texture/Consistency Modifications Use Case Description The purpose of this use case is to notify a Food & Nutrition Services department of an order that relates to resident/patient texture modification. Texture modification is part of the diet order, and may have different textures ordered for different food groups, e.g., ground meat, or individual foods for one resident/patient. In addition, texture modification could include snacks and meals at different consistencies recommended by the Speech and Language Pathologist (SLP) and/or the physician which must be communicated to the Food & Nutrition Services department or resident/patient care staff. Preconditions 1. The patient has been transferred from a nursing home and is admitted to an inpatient nursing unit of an acute care hospital 2. Admission nutrition screening has already been completed on the patient 3. The acute care hospital uses an electronic health record (EHR) 4. The acute care hospital does not have a CPOE. 5. The acute care hospital uses an electronic food and nutrition management system (FNMS) 6. The acute care hospital EHR and FNMS share information via HL7 interface, either one-way or bidirectional. Use Case Sequence of Steps 1. Resident/Patient swallowing status warrants a texture modification per the recommendations of the Speech/Language Pathologist. 2. The Speech/Language Pathologist per protocol writes an order for Puree diet. Since this particular order is not for a specific day or meal, it applies to all days and meals. Note: For multiple texture modifications for one resident/patient the SLP or authorized provider may write orders designating that the modification is for certain days, meals, or specific food groups/foods. 3. The written order is transcribed and entered into the EHR 4. Puree order is sent to Food & Nutrition Services via HL7-compliant interface to the department’s food & nutrition management software system. 5. Once in the Resident’s/patient’s record, any tray ticket or snack/nourishment label printed from the FNSM for that patient will print with Puree listed. 13 Actors Adam Everyman (Patient) Harold Hippocrates (Physician) Nancy Nightingale (Registered Nurse) Ellen Enter (Transcriptionist) Foodservice Staff Worker (need name) Texture Modifications Adam Everyman has been diagnosed with a Transient Ischemic Attack (TIA). Dr. Harold Hippocrates writes an order for a Puree diet based on the recommendations of Speech Pathologist. Ellen Enter transcribes the order into appropriate EHR screen where she selects Puree from a distinct drop-down menu of Diet - Texture Modification options. When prompted for respective Days or Meals, Anne enters ALL and ALL, since this order is not unique to a particular day or meal. Alternatively this could be entered to begin now (0800) with no end or expire date-time. Once entered, this order is sent via interface to the Food & Nutrition Services department’s nutrition management software system where it automatically populates the appropriate area of the resident/patient record within that software system. As the next meal approaches, Joe Foodservice Worker executes functions in the department’s software system that produces tray tickets for that meal. Smith Patient’s tray ticket prints with Puree the designated area of the tray ticket. Joe’s co-workers who assemble resident/patient trays immediately recognize that this order means that only puree items are to be served on the resident’s/patient’s tray. 14 Use Case 4: Diet Order change to ‘NPO for Tests’ Use Case Description The purpose of this use case is to describe the situation where a patient’s diet order must be changed to ‘NPO’ to indicate that the patient is not allowed to eat or drink anything for a specified period of time in preparation for medical tests that will be conducted. For patient safety reasons, this scenario relies on entry of a separate, new diet order once the tests are completed indicating to foodservice that the patient may resume eating rather than modeling this using an order with an explicit expire time or suspending/holding the previous diet order. Use Case Sequence of Steps 1. Admitted patient, Adam Everyman, is transferred to the cardiac unit of the hospital and has an active diet order for a ‘General/Healthful’ diet 2. Doctor orders lab tests (e.g., Lipid Profile) for tomorrow at 0600 that require an 8-hour fast. Doctor changes the diet to ‘NPO for tests’ diet to be effective from 2200 after the evening meal service. He also authorizes nursing to enter a new order diet order to resume the ‘General/Normal’ diet after tests are completed. Orders are transmitted to FNMS of the Nutrition Services Department. 3. FNMS automatically acknowledges the new diet order electronically (e.g., sends an ACK message to the CPOE sending system) and the FNMS patient record for Adam Everyman is updated with the new diet order details. 4. The patient receives a meal service tray with appropriate foods according to the hospitals meal service policies for the evening (dinner) meal. 5. The patient is not allowed to order any additional food or beverages after 2200 hours per the ‘NPO for Tests’ diet order. 6. In the morning, the blood draw for the lab is delayed, so the patient should not be allowed to order food until that is completed and the new diet order is sent. This is one reason food and nutrition professionals responsible for patient meal do not want order to have a set expire time as many 15 7. Patient’s blood is drawn by the lab tech at 0735 and the patient is hungry, so per the physician’s authorization the nurse enters a new diet order to resume the ‘General/Healthful’ diet effective immediately. 8. FNMS receives the new diet order for ‘General/Healthful’ diet so the patient is once again allowed to order/receive meals. 9. Nutrition Services department prepares and delivers a breakfast tray to the patient. 16 Use Case 5: Pediatric Specialty Orders – NEED TO DOCUMENT Use Case Description The purpose of this use case is to describe the information required for typical pediatric diet orders. Such orders will include orders for breast feeding and infant formulas including any necessary additives or fortifiers. Components of an infant formula order: Infant formula and/or fortified breastmilk orders are placed by the physician or dietitian based upon the nutrient and caloric density required by infant. The caloric concentration of standard manufacturer infant formulas is 20 kcal/oz (0.67 kcal/mL). Hospitalized infants often require higher caloric concentrations, so formulas are mixed using high-calorie concentrated liquids (40 kcal/oz or 1.33 kcal/mL) or high-calorie ready-to-feed (22- or 24-kcal/oz) formulas to prepare the total volume of formula required. Base Formula Product by caloric density in kcal/oz (US/Canada) or kcal/30mL (Australia/Canada) or kJoules/30mL(Australia) (Need to verify this with international representatives) o Standard caloric densities – 20 kcal/oz (kcal/30mL), 22, 24, 26, 27, & 30 ProductA, 24 kcal/oz Modular Additives – Additional components may be mixed with the base formula in specific amounts or to add a certain number of kcals, carbohydrate, protein, and/or fat, such as “plus Glucose Additive to 27 kcals/oz.” Carbohydrate Additive (Liquid or Powder - 2 kcal/mL) Total caloric density (sum of base + additives) in kcals or kJoules per oz or 30mL or 100 mL To total of 27 kcal/oz Feeding frequency – e.g. every 3 hours or 8 feedings/day Volume per feeding – 3 oz (90 mL) o Total volume of feeding required per day – 24 oz (720 mL) Infant Formula Example: Formula Product A (24 kcal/oz) + CHO Additive = 27 kcal/oz 60 mL x 7 feedings/day 17 Conditions Preconditions Same as previously stated Actors/Roles Karen Kiddler (Pediatrician) Kari Kidd (Patient) Nancy Nightingale (PROV-RN) Connie Chow - Dietitian (PROV-RD) Formula Room Technician Use Case Sequence of Steps Use Case Scenario Karen Kidd is a 2-week old infant in the Neonatal Intensive Care Unit (NICU) at Good Health Hospital. 18 Use Case 6: Order Oral Nutritional Supplement Use Case Description The purpose of this use case is to notify a Food & Nutrition Services department of an order that relates to the provision of an oral nutritional supplement. Conditions This use case applies to oral beverage supplements including commercial products which are often vitamin/mineral modified and house-made preparations such as shakes made from milk and ice cream products. Specifications may be by name or by desired nutrient composition. Use of a supplement may be in addition to other diet orders or be the sole source of oral nutrient intake. Exclusions This use case does not include use of commercial or house-made supplements for tube-feedings. Products used may be identical, but this use case will only address those for oral consumption. The use case does not address herbal or encapsulated dietary supplements dispensed by pharmacy or brought by patients from home. Preconditions 1. The patient has been admitted to an inpatient nursing unit of an acute care hospital 2. Admission nutrition screening has already been completed on the patient 3. The acute care hospital uses an electronic health record (EHR) 4. The acute care hospital uses CPOE 5. The acute care hospital uses an electronic food and nutrition management system (FNMS) 6. The acute care hospital EHR and FNMS share information via a one-way or bi-directional interface. 7. The licensed entity (LIC) registered nurse (or Healthcare Provider (PROV-RN)) and registered dietitian or (Healthcare Provider (PROV-RD)) have access to the EHR. The diet clerk (DC) and the registered dietitian have access to the FNMS. Actors/Roles Rachel Resident (Physician - Author) Connie Chow (Dietitian – PROV(RD) Nancy Nightingale – (Registered Nurse - PROV(RN) 19 Adam Everyman (Patient – PAT) DC – Chris Clerk (?role code for non-providers) SDLOC – service delivery location Use Case Sequence of Steps 1. Trigger: Patient requires additional source of calories/protein/carbohydrate/fat. 2. LIC (role) enters supplement (entity) as medical order (act) into EHR a. (Alternative) RN or RD enter medical order into EHR and LIP countersigns order b. (Alternative) RN or RD enter service order into EHR 3. Order sent to FNMS via interface a. PAT role b. Service location role c. Act – diet code based on quantity, status, timing d. Entity – general statement about the supplement, material state 4. Order received and fulfilled by DC in FNMS 5. Order fulfillment sent by FNMS to EHR 6. Order resulted in EHR 7. PAT receives supplement 8. Alternate act states for cancellation, suspension Use Case Scenario Adam Everyman is admitted to Good Health Hospital with second degree burns. A high-calorie diet is ordered but the RD notes that the patient is still not consuming adequate calories. The RD confers with the LIP and they agree that a liquid oral supplement should be provided to Adam Everyman. The LIC enters a supplement order into the EHR. The order contains the following information: 1. 2. 3. 4. 5. 6. The patient name The patient identifier Prescriber Patient location Date/Time of order The name of the supplement (commercial canned or house-made) or the desired nutrient composition of the supplement 7. Start Date/Stop Date 8. Start Time/Stop Time or meal/nourishment association 9. Quantity per administration 20 The order is then electronically passed from the EHR to the FNMS. The FNMS acknowledges receipt of the order. The FNMS places the new order information into its patient record. The RD (or DC) reviews the order to ensure it is accurate and appropriate, or the FNMS has the ability to determine if the supplement is appropriate based on other diet orders. The DC then utilizes the FNMS to issue the desired supplement from inventory (or preparation instructions) and a delivery ticket to accompany the supplement to the patient location. Once a delivery ticket is generated,, the FNMS then returns an electronic message to the EHR to result the order with the following information: 1. 2. 3. 4. The patient name The patient identifier Date/Time of order fulfillment The name of the supplement provided Adam Everyman receives his supplement. 21 Use Case 7: Order Enteral Nutrition (Tube Feeding) Use Case Description The purpose of this use case is to notify a Food & Nutrition Services department that a patient requires an enteral tube feeding. ASPEN (American Society for Enteral and Parenteral Nutrition) defines “enteral nutrition” as “nutrition provided through the gastrointestinal tract via a tube, catheter, or stoma that delivers nutrients distal to the oral cavity.” Best practices for enteral nutrition (EN) orders recommend that all of the following are documented in the EN order request: (1) patient identifiers/demographics including age and weight, (2) formula and/or modular components required to meet the patient’s specific nutritional needs, (3) identification of enteral access delivery site and device (route and access), and (4) administration method and rate. Conditions This use case applies to enteral or tube feeding orders that require one or more products, whether commercially pre-prepared formula or mixed on site to include modular components, for administration through an enteral access device which is defined as a “tube placed directly into the gastrointestinal tract for the delivery of nutrients or drugs” (ASPEN Enteral Nutrition Practice Recommendations, JPEN 2009). Use of a tube feeding may be in addition to an oral diet order and/or total parenteral nutrition; or EN may be the sole source of nutrient intake for an individual unable to consume food or beverages by mouth. Exclusions This use case does not include nutritional supplements that a person would consume orally although some products used for enteral/tube feeding formulas are also suitable as oral supplements; nor does it include parenteral nutrition orders that require intravenous administration of nutrients. Note: Infant enteral formulas are a special sub-case of this main enteral nutrition order use case (to be added later). Preconditions 1. The patient has been admitted to an inpatient nursing unit of an acute care hospital 2. Patient has had an enteral access device (tube) successfully placed and has been assessed and deemed ready to initiate enteral feedings 22 3. The acute care hospital has established a formulary of available enteral formulas specific to the institution based upon patient population needs 4. The acute care hospital uses an electronic health record (EHR) 5. The acute care hospital uses CPOE (Computerized Provider Order Entry) 6. The acute care hospital uses an electronic food and nutrition management system (FNMS) 7. The acute care hospital EHR and FNMS share information via HL7-compliant interfaces 8. The licensed entity (LIC) registered nurse (or Healthcare Provider (PROV-RN)) and registered dietitian/nutrition support specialist or (Healthcare Provider (PROV-RD)) have access to the EHR. The Formula Room Technician (FT) and the registered dietitian have access to the FNMS.. Actors/Roles with class codes Aaron Attending (Physician - LIC) Connie Chow (Registered Dietitian/Nutrition Support Specialist - PROV (RD)) Nancy Nightingale (Registered Nurse - PROV(RN)) Adam Everyman (Patient - PAT) FT – Francis Tech (What is the name and role code for non-providers?) SDLOC – service delivery location (patient’s admit location – unit-room-bed) Use Case Sequence of Steps – New Enteral Nutrition Order 1. Enteral access device (Nasogastric tube) placement is confirmed and patient is assessed and ready to begin enteral nutrition feeding. (Pre-condition) 2. LIC (role) enters the enteral nutrition order (entity) as medical order (act) into CPOE/EHR a. LIP (or LIC as used her) would enter directly into EHR b. RN or RD/CNSD enter medical order into EHR as per hospital policy 3. EN order sent electronically to FNMS via interface a. PAT role b. Service location role c. Entity – d. Act – status, timing, data about the entity i. Mood – Request (RQO)) e. Act Class – Substance Administration 4. Order is received by FNMS and order receipt is acknowledged a. FNMS needs to correlate this EN tube feeding order with the medical diet order (Note: The FNMS needs to be notified if this patient is to receive solely tube feedings or whether he also requires food; this needs to be communicated in conjunction with diet order information.) 23 5. FNMS user (Formula Room Technician) prepares or assembles the required enteral products for delivery to the patient’s unit (service delivery location). FNMS generates patient-specific labels as required. 6. Enteral products for this patient are delivered to the unit to fulfill this order. 7. Upon receipt of proper formula and at the designated order start time, PROV-RN (role) begins the enteral feeding at the initial rate. 8. Initiation of EN is documented in the EHR. 9. PROV-RN advances feedings (rate and/or volume increases) as directed by the EN order protocol and documents each increase in EHR and any signs of feeding complications. a. (Is this Substance Admin or Observation?) 10. Adjustments to various components (rate, formula, etc) of enteral nutrition orders are very common as patients may experience complications or may not fully tolerate the feedings. Use Case Scenario Adam Everyman, a 55-year old male motor vehicle accident victim with multiple rib fractures, major lung contusions and haemothorax that has been drained is admitted to the Intensive Care Unit of Good Health Hospital from the Emergency Department for ventilator support. A nasogastric enteral access device has been placed and radiograph (X-ray) has confirmed proper placement. The patient has been assessed is now haemodynamically stable enough to begin enteral nutrition feedings while he awaits further surgery. After consultation with the nutrition support dietitian, a standard, polymeric enteral formula was selected from the hospital’s established formulary and a total energy target of 20-25 kcal/kg body actual weight with 1.2 – 1.5 grams protein/kg ideal body weight has been set. Aaron Attending designates a diet order of NPO (no oral food intake) and the following enteral nutrition order using City Hospital’s EN order set protocol that directs advancement of the feedings from initiation to the target goal rate within the CPOE system (see sample Adult EN Order Form): Name: Thomas Trauma MRN: 00999 DOB: 1/9/1956 Room: ICU – 10 Dosing Weight: 83.2 kg Formula: Standard* Delivery Site * Could be generic description of types or product-specific e.g., Osomolite Route: Gastric Access: Nasogastric Method of Administration: Pump-assisted Rate:_20__Initial mL/hour Advance by: 10 mL/hour every _4_hour(s) to goal of 70 mL/h Order Start Date/Time: 20110109 @ 1400 The NPO diet and EN orders are received electronically in the FNMS. Francis Technician verifies the orders received in the FNMS. She prepares and labels the required amount of enteral formula 24 products for transport to the unit. Upon receipt of the product at the unit, Nancy Nurse verifies the formula against the enteral nutrition orders and starts the tube feeding at the initial rate of 20 mL/hour following normal administration protocols (sterile water for flushing the tube, elevated head of bed, etc.) recording the date and time the formula is spiked/hung on the product label and in the EHR. After 4 hours if there are no observed feeding complications or contraindications, Nancy Nurse will increase the pump rate to 30 mL/hour and continue that process over the next 24 hours until the goal rate is achieved or the EN orders are modified. 25 Use Case 8: Meal/Special Service Designation Order (Note: Needs work – need to revise actor names and abbreviations and put into above format.) Use Case Description The purpose of this use case is to notify a Food & Nutrition Services department of an order that relates to patient tray delivery. As opposed to a diet order, a Meal/Special Service Designation is a message either about delivery time (eg, Hold Tray, Late Tray, Early Tray), adaptive equipment (eg, Built-up Spoon, Plate Guard), staff assistance (eg, Cut Up Meat, Open Cartons), or isolation precautions (eg, Isolation Tray, Disposable Dishes). In addition, a Meal/Special Service designation could include messages such as Tray to Nurse’s Station, VIP, Suicide Precautions, or any other messaging relevant to and desired by the Food & Nutrition Services department or patient care staff. Use Case Sequence of Steps 1. Patient’s diagnosis warrants isolation precautions; physician writes/enters order for Isolation Tray. 2. Since this particular order is not for a specific day or meal, ALL is selected for Days and Meals. 3. Isolation Tray order is sent to Food & Nutrition Services, either via HL7-compliant interface to the department’s food & nutrition management software system, or via a printout in the department. 4. Once in the patient’s record, any tray ticket or snack/nourishment label for that patient will print with Isolation Tray listed. For sensitive messages (eg, Suicide Precautions), rather than printing on the patient’s tray ticket as such, either a departmentally-defined code could be used (eg, ******) or the particular services could be set to not print on the tray ticket. Staff could instead obtain a list of respective patients via an ondemand report and adjust trays accordingly. Actors Prescott Patient Daniel Doctor Uma Unit Secretary Frank Foodservice Staff Worker 26 Use Case Scenario for Meal/Special Service Designation Prescott Patient has been diagnosed with H1N1 influenza. Daniel Doctor gives a verbal order for Isolation Tray (Disposable Dishes) to Uma Unit Secretary. Uma Unit Secretary proceeds to the appropriate EHR screen where she selects Isolation Tray from a distinct drop-down menu of Meal/Special Service options. When prompted for respective Days or Meals, Uma enters ALL and ALL, since this order is not unique to a particular day or meal (as opposed to, for example, Early Tray for tonight’s dinner only). Once entered, this order is sent via interface to the Food & Nutrition Services department’s nutrition management software system where it automatically populates the appropriate area of the patient record within that software system. As the next meal approaches, Frank Foodservice Worker executes functions in the department’s software system that produce tray tickets for that meal. Prescott Patient’s tray ticket prints with Isolation Tray in large font in the designated area of the tray ticket. Frank’s co-workers who assemble patient trays immediately recognize that this order means that only paper or plastic dishes and utensils are to be used for this patient’s tray. Prescott Patient is served his tray on entirely disposable materials. After Prescott finishes consumption of his meal, the staff member discards the entire tray and all its contents. 27 Use Case 9: Request RD/Nutrition Consult Use Case Description The purpose of this use case is to place an order for a dietitian to consult on a hospital inpatient and the subsequent fulfillment of that order request. Summary: 1. LIC instantiates dietitian consultation order in the EHR. 2. Order is communicated to RD directly via EHR reports/alerts as well as via an interface to the FNMS. 3. RD receives order, completes requested service and documents service. Actors/Roles with class codes LIC – Daniel Doctor PROV-RD (Registered Dietitian/Nutritionist Healthcare Provider) Hospital Unit Clerk (Data Entry) Preconditions: 1. The patient has been admitted to an inpatient nursing unit of an acute care hospital 2. A need for RD consultation is determined by the LIC 3. The RD is authorized to provide all nutrition-related consultation services requested by the LIC 4. Nutrition-related consultation services include, but are not limited to: Patient nutrition assessment, follow-up evaluation, education assessment, patient counseling, patient education, discharge assessment, calorie count, TPN order recommendation, enteral feeding recommendation. 5. Admission nutrition screening has already been completed on the patient 6. The acute care hospital uses a electronic medical record or EHR. 7. The acute care hospital also uses an EOS 8. The LIC, RD and HUC are authorized users of the EOS 28 9. The acute care hospital also uses an EDS 10. The LIC, RD and HUC are authorized users of the EDS 11. The acute care hospitals EDS and EOS share information via a bi-directional interface (or may be integrated as one EHR). 12. The acute care hospital does not use CPOE Glossary: Term Definition AF1 Alternate Flow 1 AF2 Alternate Flow 2 AF3 Alternate Flow 3 Communication Device: A regular telephone, cellular phone, pager, radio, or CD other communication hardware by which one individual communicates a message to another individual verbally or using readable text. Communication Output: A record by which the results of communication from one individual can be viewed by another individual. May include, but is not CO limited to: Automated computer print-out, computer report viewed on print output or on-screen, or paper message delivered by hand/pneumatic tube system or other means. CPOE Computerized Physician Order Entry EDS Electronic Documentation System EHR Electronic Health Record EOS Electronic Ordering System HUC Hospital nursing Unit Clerk LIC Licensed Independent Practitioner: Physician, Physician Assistant, Nurse Practitioner, or other licensed individual authorized to place patient orders. NSD Nutrition Services Department PMR Paper Medical Record RD Registered Dietitian 29 RDCO Registered Dietitian Consult Order TPN Total Parenteral Nutrition Basic Flow: Line 1 2 Actor Action System Response LIC writes order in PMR for RDCO In reviewing PMR for orders, HUC finds RDCO. 3 HUC logs into EOS HUC log-in authenticated 4 HUC enters RDCO into EOS EOS confirms entry of RDCO 5 HUC initials PMR to affirm that RDCO has been processed. 6 NDS receives RDCO via CO 7 NDS communicates RDCO to RD via CD 8 RD receives RDCO 9 RD completes requested service(s) 10 RD logs into EDS 11 RD selects patient for whom service(s) was/were provided. RD log-in authenticated EDS displays appropriate patient EDS prompts RD to affirm that 12 RD documents service(s) provided documentation is correct and to electronically sign documentation. RD clicks on appropriate button to 13 affirm electronic signature for EDS confirms signed documentation documentation. 14 15 EDS communicates completed RDCO to EOS RD signs out of EDS Post Conditions: 30 The requested service for the patient has been completed and the nutrition staff takes this service into consideration in planning for any additional care for the patient. Alternate Flows: AF1 – EHR with Full CPOE Preconditions: 1. Assume basic flow preconditions # 1-5 2. Acute care hospital has EHR with fully functioning CPOE 3. The LIC, RD and HUC are authorized users of the EHR Line System Actor Action System Response 1 LIC logs into EHR LIP log-in authenticated 2 LIC selects appropriate patient EHR displays appropriate patient 3 LIC enters RDCO EHR confirms entry of RDCO EHR automatically communicates RDCO to 4 RD via CD. 5 RD receives RDCO 6 RD completes requested service(s) 7 RD logs into EHR 8 RD selects patient for whom service(s) was/were provided. RD log-in authenticated EHR displays appropriate patient EHR prompts RD to affirm that 9 RD documents service(s) provided documentation is correct and to electronically sign documentation. RD clicks on appropriate button to 10 affirm electronic signature for EHR confirms signed documentation documentation. 11 RD signs out of EHR Post Conditions: 31 The requested service for the patient has been completed and the nutrition staff takes this service into consideration in planning for any additional care for the patient. AF2 – EHR + Order Set Preconditions: 1. Assume basic flow preconditions # 1-6 2. Acute care hospital has EHR with CPOE that generates printed order sets 3. The LIC, RD and HUC are authorized users of the EHR Line System Actor Action System Response 1 LIC logs into EHR LIP log-in authenticated 2 LIC selects appropriate patient EHR displays appropriate patient 3 LIC enters RDCO EHR confirms entry of RDCO 4 EHR prints copy of order set 5 LIC logs out of EHR 6 LIC places order set in PMR 7 In reviewing PMR for orders, HUC finds RDCO. 8 HUC logs into EHR HUC log-in authenticated 9 HUC enters RDCO into EHR EHR confirms entry of RDCO EHR automatically communicates RDCO to 10 11 RD via CD. HUC initials PMR to affirm that RDCO has been processed. 12 RD receives RDCO 13 RD completes requested service(s) 14 RD logs into EHR 15 RD selects patient for whom service(s) was/were provided. RD log-in authenticated EHR displays appropriate patient 32 EHR prompts RD to affirm that 16 RD documents service(s) provided documentation is correct and to electronically sign documentation. RD clicks on appropriate button to 17 affirm electronic signature for EHR confirms signed documentation documentation. 18 RD signs out of EHR Post Conditions: The requested service for the patient has been completed and the nutrition staff takes this service into consideration in planning for any additional care for the patient. AF3 – Simple PMR Preconditions: 1. Assume basic flow preconditions # 1-6 Line 1 2 3 4 System Actor Action System Response LIC writes order in PMR for RDCO In reviewing PMR for orders, HUC finds RDCO. HUC communicates RDCO to NDS via CO or CD. HUC initials PMR to affirm that RDCO has been processed. 5 NDS receives RDCO via CO 6 NDS communicates RDCO to RD via CD 7 RD receives RDCO 8 RD completes requested service(s) 9 RD documents service(s) provided; 33 signs and dates documentation. Post Conditions: The requested service for the patient has been completed and the nutrition staff takes this service into consideration in planning for any additional care for the patient. Questions: What other use cases are connected to the RDCO? The calorie count service requires interim work by diet technicians, nursing or others before the RD can document completion. The TPN recommendation service requires assessment and calculation work on the part of the dietitian as well as possible collaboration with pharmacy. How many additional alternate flows are possible? Only 4 variations are shown in order to highlight some of the most common situations, however numerous iterations are possible based on the combination of systems and work flows available in different hospitals. How would other task list, messaging and alerting functionality of systems affect the use case? Many EHR’s available today offer more sophisticated work flow processing with these tools. Story Board: - Provider writes order for dietitian consult in paper medical record; signature and date/time written by provider. 34 - While processing new patient orders from the paper medical record, unit clerk finds the dietitian consult order, enters it in the ordering section of the electronic health record (EHR) and initials the order in the paper medical record. - The dietitian consult order is communicated through the EHR to the Nutrition Services Department (print out, page, text message to cell, periodically printed report). - The Nutrition Services Department contacts the dietitian responsible for the patient on which the order was placed and communicates the details of the consult order. - The dietitian completes the requested service, and then documents the care in the EHR with appropriate signature, date and time. 35 Sequence and Activity Diagrams DIET ORDER SEQUENCE MD diet order, supplements, RD consult, VO orders, assigns magmt of TPN or TF others CPOE or paper chart EMR NURSING Order flavor of supplement, VO orders hold diet for test, allergies, late or early tray Dietitian input Limited access for VO or clinical privileges Limited access for info HL7 interface Documentation of care plan, educ. And order labs, TPN and adjusts electrolytes FNMS FOOD & NUTRITION MGT SYS Diet Clerk food preferences, allergies, intolerances; notifies diet consult, corrects diet order errors; inputs nourishment requests Diet Supplement Flow Chart Electronic Health Record ORDER Supplement 1000 Calories per Day PAT Role, Service location, Diet Code, Entity Food and Nutrition Management System LIC Order Received and Approved by Provider or Diet Clerk PROV Order Resulted PAT Order fulfilled with available supplement that meets criteria Supplement Provided to Patient 36 Glossary (Need to merge with existing HL7 Glossary + EHR Functional Model + Nutrition CME sources) Diet – (V3) A supply Act dealing specifically with the feeding or nourishment of a subject. The detail of the diet is given as a description of the Material associated via Participation.typeCode = “product”. Medically relevant diet types may be communicated in Diet.Code, however, the detail of the food supplied and the various combinations of dishes should be communicated as Material instances. Examples – gluten free, low sodium. From HL7 Glossary: A diet consists of the diet codes, supplements, and preferences effective at a given time. These three specifications govern which foods a patient will receive. Diets generally do not have a stated ending time to ensure that the patient always receives food. Diet Code - A diet code defines which foods a patient may receive; a patient must have at least one diet code to receive food. Dietary Orders - An order for a patient diet. A patient may have only one effective dietorder at a time. Diet.energyQuantity (PQ): deprecated concept. Convey quantity using a content relationship with an attribute expressing “calories”. The physical quantity SHOULD be convertible to 1 kcal/d (or 1 kJ/d). Diet.carbohydrateQuantity (PQ): express content relationship to an entity with a code of “carbohydrate” and a quantity attribute on the content relationship e.g. the supplied amount of carbohydrates per day. Convey carbohydrate restriction in the carbohydrateQuantity. Use case in grams, but not constrained to this unit of measure. EHR – Electronic Health Record: A comprehensive, structured set of clinical, demographic, environmental, social, and financial data and information in electronic form, documenting the health care given to a single individual.(ASTM E1769, 1995) Various, including DC.1 Material (MAT): A subtype of Entity that is inanimate and locationally independent. Example – food. ODS - (New with Version 2.2) Dietary orders, supplements and preferences segment. ODT - (New with Version 2.2) Diet tray instructions segment. OMD - Dietary order message. ORD - Dietary order - General order acknowledgement message Order - An order is a request for a service from one application to a second application. The second application may in some cases be the same, i.e., an application is allowed to place orders with itself. Usually orders are associated with a particular patient. Order Detail Segment - One of several segments that can carry order information. Examples are OBR and RXO Supply (SPLY): provision of a material by one entity to another. Provide Material class Trigger Event The event that initiates an exchange of messages is called a trigger event. The HL7 Standard is written from the assumption that an event in the real world of health care creates the need for data to flow among systems. The real-world event is called the trigger event. For example, the trigger event “a patient is admitted” may cause the need for data about that patient to be sent to a number of other systems. There is a one-to-many relationship between message types and trigger event codes. The same trigger event code may not be associated with more than one message. 37 38 References and Acronyms HL7 Healthcare Development Framework Version 1.5 Release 1 Acronym Meaning EHR Electronic Health Record EMR Electronic Medical Record HDF HL7 Development Framework PHR Personal Health Record Note The HL7 development methodology 39 Appendix: Storyboard naming standards Table 5: Patient Information for Storyboards Cast Family Given MI Gender SSN patient, female Everywoman Eve E F 444-22-2 patient, male Everyman Adam A M 444-33-3 patient, child Kidd Kari K F 444-55-5 family, daughter Nuclear Nancy D F 444-11-4 family, husband Nuclear Neville H M 444-11-1 family, son Nuclear Ned S M 444-11-3 family, wife Nuclear Nelda W F 444-11-2 next of kin (parent) Mum Martha M F 444-66-6 next of kin (child) Sons Stuart S M 444-77-7 next of kin (spouse) Betterhalf Boris B M 444-88-8 next of kin (other) Relative Ralph R M 444-99-9 contact person Contact Carrie C F 555-22-2 Cast Family Given MI Gender SSN healthcare provider Seven Henry L M 333-33-3 assigned practitioner Assigned Amanda A F 333-44-4 physician Hippocrates Harold H M 444-44-4 primary care physician Primary Patricia P F 555-55-5 admitting physician Admit Alan A M 666-66-6 attending physician Attend Aaron A M 777-77-7 referring physician Sender Sam S M 888-88-8 intern Intern Irving I M 888-22-2 resident Resident Rachel R F 888-33-3 chief of staff Leader Linda L F 888-44-4 authenticator Verify Virgil V M 999-99-9 specialist Specialize Sara S F 222-33-3 allergist/immunologist Reaction Ramsey R M 222-22-3 anesthesiologist Sleeper Sally S F 222-66-6 Table 6: Healthcare Staff for Storyboards HL7 Version 3 Domain Analysis Model: Diet and Nutrition Orders Draft Release 1.0 – Use Cases and Storyboards January 2010 WGM Page 40 HL7 Version 3 Diet Orders 41 Cast Family Given MI Gender SSN cardiologist Pump Patrick P M 222-33-4 cardiovascular surgeon Valve Vera V F 222-33-5 dermatologist Scratch Sophie S F 222-33-6 emergency medicine specialist Emergency Eric E M 222-33-7 endocrinologist Hormone Horace H M 222-33-8 family practitioner Family Fay F F 222-33-9 gastroenterologist Tum Tony T M 222-44-2 geriatrician Sage Stanley S M 222-44-3 hematologist Bleeder Boris B M 222-44-3 infectious disease specialist Pasteur Paula P F 222-44-5 internist Osler Otto O M 222-44-6 nephrologist Renal Rory R M 222-44-7 neurologist Brain Barry B M 222-44-8 neurosurgeon Cranium Carol C F 222-44-9 OB/GYN Fem Flora F F 222-55-2 oncologist Tumor Trudy T F 222-55-3 ophthalmologist Vision Victor V M 222-55-4 orthopedic surgeon Carpenter Calvin C M 222-55-5 otolaryngologist (ENT) Rhino Rick R M 222-55-6 pathologist Slide Stan S M 222-44-4 pediatrician Kidder Karen K F 222-55-7 plastic surgeon Hollywood Heddie H F 222-55-8 psychiatrist Shrink Serena S F 222-55-9 pulmonologist Puffer Penny P F 222-66-2 radiologist Curie Christine C F 222-55-5 rheumatologist Joint Jeffrey J M 222-66-3 surgeon Cutter Carl C M 222-77-7 urologist Plumber Peter P M 222-66-4 physician assistant Helper Horace H M 222-66-5 registered nurse Nightingale Nancy N F 222-88-8 nursing assistant Barton Clarence C M 222-99-9 chiropractor Bender Bob B M 222-66-6 HL7 Version 3 Diet Orders 42 Cast Family Given MI Gender SSN dentist Chopper Charlie C M 222-66-7 orthodontist Brace Ben B M 222-66-8 optometrist Specs Sylvia S F 222-66-9 pharmacist Script Susan S F 333-22-2 podiatrist Bunion Paul B M 222-77-2 psychologist Listener Larry L M 222-77-3 lab technician Beaker Bill B M 333-44-4 dietician Chow Connie C F 333-55-5 social worker Helper Helen H F 333-66-6 occupational therapist Player Pamela P F 222-77-6 physical therapist Stretcher Seth S M 222-77-8 transcriptionist Enter Ellen E F 333-77-7 Pastoral Care Director Sacerdotal Senior S M 333-77-7 Chaplain Padre Peter P M 333-77-7 Informal Career Comrade Connor C M 333-77-7 Electrophysiologist Electrode Ed E M 333-77-7 Laboratory Specimen Processor Spinner Sam S M 333-45-4 IT System Administrator Admin I. T. M 333-33-3 Table 7: Organizations for Storyboards HL7 Version 3 Diet Orders 43 Organizational Roles Role Name Phone Address City State healthcare provider organization Level Seven 555-555- 4444 Ann Arbor MI Healthcare, Inc. 3001 Healthcare Ann Arbor MI Ann Arbor MI Ann Arbor MI Drive healthcare insurer #1 healthcare insurer #2 employer Health Authority HC Payor, Inc. Uare Insured, Inc. Work Is Fun, Inc. 555-555- 5555 Insurers 3002 Circle 555-555- 8888 Insurers 3015 Circle 555-555- 6666 Worker 3003 Loop 555-555- 22 Wordy Way Ann Arbor MI Health Authority West terminology provider Titan Terminology 3099 Table 8: Facilities for Storyboards Role Name Phone Address City State healthcare provider Community Health 555-555- 1000 Enterprise Ann Arbor MI and Hospitals 5000 Blvd Good Health 555-555- 1000 Hospital Ann Arbor MI Hospital 3004 Lane GHH Inpatient Unit 555-555- hospital hospital unit (e.g., BMT) 3005 (ext 123) hospital ward GHH Patient Ward 555-5553006 (ext 456) hospital room GHH Room 234 555-5553007 (ext 789) emergency room GHH ER 555-5553008 (ext 246) HL7 Version 3 Diet Orders 44 Role Name Phone operating room GHH OR 555-555- Address City State Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI 3009 (ext 321) radiology dept. GHH Radiology 555-5553010 (ext 654) laboratory, in-house GHH Lab 555-5553011 (ext 987) pharmacy dept. GHH Pharmacy 555-5553012 (ext 642) outpatient clinic GHH Outpatient 555-555- Clinic 3013 (ext 999) urgent care center physical therapy clinic home health care clinic chiropractic clinic optician clinic pharmacy, retail laboratory, commercial nursing or custodial care facility Community Urgent 555-555- 1001 Village Care 4001 Avenue Early Recovery Clinic 555-555- 1010 Village 4006 Avenue Home Health Care 555-555- 1030 Village Clinic 4008 Avenue Bender Clinic 555-555- 1040 Village 4009 Avenue See Straight 555-555- 1050 Village Opticians 4010 Avenue Good Neighbor 555-555- 2222 Village Pharmacy 4002 Avenue Reliable Labs, Inc. 555-555- 3434 Industrial 4003 Loop Green Acres 555-555- 4444 Retirement Home 4004 Nursinghome Drive residential treatment facility Home Away From 555-555- 5555 HL7 Version 3 Diet Orders 45 Role Name Phone Address Home 4005 Residential City State Ann Arbor MI Ann Arbor MI Ann Arbor MI Ann Arbor MI Lane satelite clinic satelite clinic satelite clinic satelite clinic Lone Tree Island 555-555- 1001 Lone Tree Satellite Clinic 5001 Rd Stone Mountain 555-555- 1000 Mountain Satellite Clinic 5002 Way Three Rivers 555-555- 1000 River Satellite Clinic 5003 Drive Bayview Satellite 555-555- 1000 Lakeside Clinic 5004 Drive