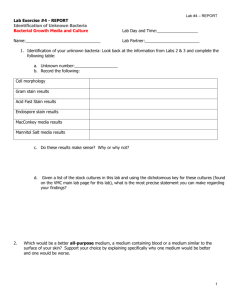
5a Lab Instructions
advertisement

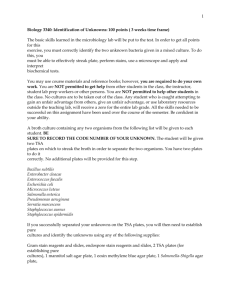
Lab 5 Instructions Chapter 26 (Hand scrubbing)…see lab manual Chapter 45: Skin Bacteria The dry keratin layers of the epidermis of the skin are not easily colonized by most microbes. Sebum from oil gland and salts in perspiration inhibit the growth of most microbes. Therefore, the skin is an inhospitable environment for most microbes. Only a few types of bacteria (normal resident microbiota) can tolerate the dry keratin and the hypertonic environment of the skin (which is caused by salt in our perspiration). The most common types of bacteria found on the skin are Gram positive, salttolerant organisms such as Staphylococcus aureus. More bacteria are found in moist areas, such as the axilla and the sides of the nose. Transient microbes may be present on the hands and arms because of contact with the environment, but they do not live on our skin for long. Propionibacterium live in hair follicles on sebum produced by our oil glands. The propionic acid they produce maintains the acidic pH of our skin (pH 3-5), which suppresses the growth of other bacteria. Streptococcus is also part of the normal microbiota of the skin. Mannitol salt agar (MSA) is selective for salt-tolerant organisms and it is also considered to be a differential media because mannitol-fermenting organisms will produce acid, turning the pH indicator in the media yellow. Staphylococcus aureus is part of the normal microbiota of the skin and is a pathogen. If the skin becomes broken, it can invade and cause disease. Both pathogenic and non-pathogenic species of Staphylococcus produce catalase and collagenase, and they are all oxidase negative. Staph aureus makes an enzyme called coagulase, which clots the blood (clumping), whereas other species of Staphylococcus do not produce this enzyme and are not pathogenic. If MSA grows an organism, we know it is Staphylococcus, but then we do a coagulase test to see if it is Staph aureus or not. Each INDIVIDUAL takes one Mannitol Salt Agar (MSA) plate and inoculates it with a swab from your own skin surface by streaking for confluence (tight zig-zag from top to bottom) with a cotton swab. Moisten the sterile swab with plain water, and swab an area of your skin. Good areas to find Staph aureus include the outside of your nose, the inside of your nose, the axilla (armpit), the inside of your elbow. However, you can swab wherever you like. Write down the location you chose in your lab manual at the end of Ch 45. Then add a Novobiocin antibiotic disc in the center. When we examine the plates next lab, growth indicates Staphylococcus (it’s the only genus that grows on high salt levels; that’s what makes MSA selective media), and if the organism can ferment mannitol (a sugar), the waste product (an acid) will turn the pH indicator yellow (that’s what makes the agar differential). The yellow color in the media will differentiate the species of Staphylococcus. Staph aureus and Staph saprophyticus (yellow colonies) are mannitol fermenters, while Staph epididymis and Micrococcus (white colonies) do not ferment mannitol. You could then do a coagulase test (S. aureus would be the only one positive). Today, place a Novobiocin antibiotic disc on your plate. If a clear zone develops around the nonfermenting colonies, the organism is Staph epidermidis. A Gram stain would show Micrococcus as being Gram positive cocci that are very tiny. Then do a catalase test to differentiate streptococci (negative) for staphylococci (positive). Take a toothpick, scoop up a colony, and place it on a glass slide. Use a pipette to add a drop of hydrogen peroxide to the colony. Bubbles are a positive test, which means that organism has the catalase enzyme, so it can break down hydrogen peroxide in the lysosomes of our WBCs; that is a virulence factor. H2O2 H2O + O2 (water and bubbles). 1 Chapter 46: Respiratory Bacteria The lower respiratory tract (larynx, trachea, bronchial tubes, and alveoli) is normally sterile, but the upper respiratory tract (nose and throat) is not because it is in contact with the contaminated air we breathe. The throat is a warm, moist environment, allowing many bacteria to thrive. It is normal to find Staphylococcus, Streptococcus, Neisseria, and Haemophilus as normal microbiota in the throat. However, we do not often become ill because of their antagonism toward each other. They suppress each other’s growth by competing for nutrients and producing inhibitory substances. Streptococcal species are the predominant organisms in throat cultures, and some species are the major cause of sore throats. Pathogenic bacteria may produce hemolysins, which breaks down red blood cells. HEMOLYSIS TEST (Controls: Beta = Strep pyogenese; gamma = E. coli, alpha = Streptococcus pneumoniae) Have your lab partner swab the back of your throat and then use it to inoculate a blood agar plate using the streak for confluence method. You will use this plate to observe hemolysis patterns. Beta hemolysis (Streptococcus pyogenes, Staphylococcus aureus) means the organism can completely lyse red blood cells and they digest the hemoglobin (they are pathogenic bacteria), so there will be clear zone with a clean edge around the colonies on your plate. Alpha hemolysis (Streptococcus pneumoniae) means the bacteria partially destroys the red blood cells, and they oxidize the iron in the hemoglobin, which turns the colony green, with a cloudy zone around the colony and NO clear areas. Gamma hemolysis means the organism is non-hemolytic, so there will be NO clear areas, and the colony will not be green. Streptococci that are alpha or gamma hemolytic are usually normal microbiota, whereas beta-hemolytic streptococci are usually pathogens. More than 90% of streptococcal infections are caused by Beta-hemolytic Group A Streptococcus (Strep pyogenes), which is sensitive to the antibiotic bacitracin, whereas other streptococci are resistant to it. Each INDIVIDUAL takes one Blood Agar plate and inoculates it with a swab from your own throat by streaking for isolation with a cotton swab. Do not swab your own throat; have your lab partner do it. See the photo in Ch 46 of your lab manual for the place in the throat to swab. Make sure you do not touch the cotton to the tongue. Do not wet it with water first; use it dry. Next week, look for alpha (green zone), beta (clear zone), and gamma (no change) hemolysis. One person will inoculate one blood agar plate with Streptococcus pyogenes on one half and Streptococcus pneumoniae on the other half. This will be a control plate for the whole class to observe. When you have inoculated all the plates from Chapters 25, 45 and 46, tape together all of the plates from your lab group, label the tape with the date, Magrann, Ex 25, 45-6, and your lab group number and place them INVERTED (agar on the top) into the incubator. SOIL PROJECT Use your working stock (isolation plate) to perform the following tests for morphological characteristics 1) Gram stain to determine Gram +/- and shape (rods or cocci) 2) Negative stain to determine shape and arrangements (staph, strep, diplo, singles) 3) Motility stab 4) Hanging drop to observe if it runs or tumbles 5) Endospore stain Use your working stock to perform the following tests for cultural characteristics 1) Inoculate a broth and plate to observe colony morphology. Use the terminology from your lab manual to describe it. A. NUTRIENT BROTH CHARACTERISTICS: 2 1. Is there turbidity (cloudiness)? 2. Is there growth only at the top (pellicle), only at the bottom (sediment), flakes in the middle (flocculant), or growth throughout (uniform turbidity)? 3. What color is it? B. PLATE CHARACTERISTICS: 1. MARGINS (look at the surface of the plate) a. Filiform (thread-like edge) b. Arborescent (tree-like branches) c. Beaded (starts smooth, breaks into individual colonies at top) d. Effuse (edges are not clearly defined) e. Rhizoid (root-like branches) f. Echinulate (serrated edge) 2) TEXTURE (look at surface of plate) a. Flay, dry (Bacillus megatarium) b. Spreading (proteus, pseudomonas) c. Crusty, waxy (mycobacterium) d. Transparent 3) PIGMENTATION (color of plate) a. Yellow b. White c. Green d. Etc 4) ELEVATION a. Convex b. Flat c. Raised d. Umbonate 2) Determine the optimal temperature by inoculating 3 TSB tubes, labeled with three different temperatures you want to incubate at. Use the spectrophotometer to calculate their optical density at the next lab period. The tube with the most growth (highest OD) is the temperature they prefer. 3) Determine the oxygen requirements by inoculating a thioglycolate tube. Next lab period, record if it is a strict aerobe, strict anaerobe, or facultative anaerobe. 4) Determine if your organism displays hemolysis by inoculating a blood agar plate THIS SATURDAY’S LAB Chapter 25 Last lab, each lab group took 3 Petri plates of Mueller-Hinton agar (looks like nutrient agar). You inoculated one plate with Staph aureus, one with E. coli, and one with Pseudomonas aeruginosa. You then placed 5 different antibiotic discs on each plate. Now measure the zones of inhibition for each disk (the whole diameter of the clear zone, including the disc), compare them to the chart on p.193, and complete the lab manual questions for chapter 25. Note that your lab manual does not list three of your antibiotics on page 193. Here are their values: http://www.microrao.com/micronotes/pg/kirby_bauer.pdf Neomycin 12 = Resistant 13-16 = Intermediate 45 17Chapter = Sensitive Kanomycin 13 = Resistant 14-17 = Intermediate 18 = Resistant Novobiocin 17 = Resistant 18-21 = Intermediate 22 = Sensitive 3 Last week, each INDIVIDUAL took one Mannitol Salt Agar (MSA) plate and inoculated it with a swab from your own skin surface. Examine that plate. Growth indicates Staphylococcus (it’s the only genus that grows on high salt levels; that’s what makes MSA selective media), and if the organism can ferment mannitol (a sugar), the waste product (an acid) will turn the pH indicator yellow (that’s what makes the agar differential). Describe your colonies according to p.28 in your lab manual, and record the results on p. 355 of your lab manual. Do a Gram stain (review p. 55) on one of the colonies. The yellow color in the media will differentiate the species of Staphylococcus. Staph aureus and Staph saprophyticus (yellow colonies) are mannitol fermenters, while Staph epididymis and Micrococcus (white colonies) do not ferment mannitol. If we did a coagulase test (we will not), S. aureus would be the only positive organism. Then do a catalase test to differentiate streptococci (negative) for staphylococci (positive). Take a toothpick, scoop up a colony, and place it on a glass slide. Use a pipette to add a drop of hydrogen peroxide to the colony. Bubbles are a positive test, which means that organism has the catalase enzyme, so it can break down hydrogen peroxide in the lysosomes of our WBCs; that is a virulence factor. H2O2 H2O + O2 (water and bubbles) Chapter 46 Last lab, each INDIVIDUAL took one Blood Agar plate and inoculated it with a swab from your own throat. Examine that plate by HOLDING IT UP TO THE LIGHT and look for hemolysis patterns: alpha (green zone, as seen in Strep pneumonia), beta (clear zone, as seen in Strep pyogenes which causes strep throat), and gamma (no change) hemolysis. Do a Gram stain on one colony (review on p. 55). Also do a Gram stain on your experimental plates. 4