type I
advertisement

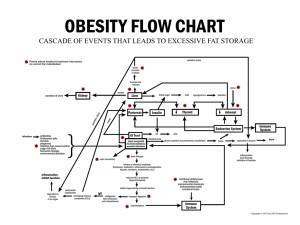
Immunopathology Ahmad Shihada Silmi Hematologist & Immunologist IUG Section A Hypersensitivity Gell and Coombs Classification of Hypersensitivities Types of Hypersensitivity Adapted from: Kuby Immunology, Sixth Edition Type I Hypersensitivity Classic allergy • Mediated by IgE attached to Mast cells. • The symptoms resulting from allergic responses are known as anaphylaxis. – Includes: Hay fever, asthma, eczema, bee stings, food allergies. Allergens • Allergens are nonparasite antigens that can stimulate a type I hypersensitivity response • Allergens bind to IgE and trigger degranulation of chemical mediators. Allergens Proteins Foreign serum Vaccines Plant pollens Drugs Penicillin Sulfonamides Local anesthetics Foods Nuts Eggs Insect products Bee venom Dust mites Mold Spores Animal hair and dander Characteristics of allergens • Small 15-40,000 MW proteins. • Specific protein components • Often enzymes. • Low dose of allergen • Mucosal exposure. • Most allergens promote a Th2 immune response. Allergens Example: Der P1 • Der P1 is an enzyme allergen • from the fecal pellets of the dust mite. Der P1 Allergen Allergen is easily aerosolized and inhaled. Der P1 breaks down components of tight junctions which helps it to cross mucosa. Atopy • Atopy is the term for the genetic trait to have a predisposition for localized anaphylaxis. • Atopic individuals have higher levels of IgE and eosinophils. Genetic Predisposition Type I hypersensitivity • Candidate polymorphic genes include: – – – – – IL-4 Receptor. IL-4 cytokine (promoter region). FcεRI. High affinity IgE receptor. Class II MHC (present peptides promoting Th2 response). Inflammation genes. Mechanisms of allergic response Sensitization • Repeated exposure to allergens initiates immune response that generates IgE isotype. • Th2 cells required to provide the IL-4 required to get isotype switching to IgE. Mechanisms of allergic response Sensitization Th2/B cell interaction Drive B cell Activation and IgE secretion Mechanisms of allergic response Sensitization • The IgE can attach to Mast cells by Fc receptor, which increases the life span of the IgE. • Half-life of IgE in serum is days whereas attached to FcεR it is increased to months. Mechanisms of allergic response Fc ε receptors (FcεR) FcεR1 • High affinity IgE receptor found on • mast cells/basophils/activated eosinophils. • Allergen binding to IgE attached to FcεR1 triggers release of granules from cell. Mechanisms of allergic response Effector Stage of Hypersensitivity Secondary exposure to allergen • Mast cells are primed with IgE on surface. • Allergen binds IgE and cross-links to activate signal with tyrosine phosphorylation, Ca++ influx, degranulation and release of mediators. Type I hypersensitivity. IgE produced in response to initial allergen exposure binds to Fc receptors on mast cells and basophils. Rechallenge with the same allergen leads to release of histamine and other mediators, which produce various symptoms of localized atopic reaction or generalized anaphylaxis. Type I: Effects of Degranulation Mediators of Type I Hypersensitivity Immediate effects • Histamine • Constriction of smooth muscles. • Bronchiole constriction = wheezing. • Constriction of intestine = cramps-diarrhea. • Vasodilation with increased fluid into tissues causing increased swelling or fluid in mucosa. • Activates enzymes for tissue breakdown. • Leukotrienes • Prostaglandins Immediate vs. late effects Mediators of Type I Hypersensitivity Primary Mediators Pre-formed mediators in granules • Histamine • Cytokines TNF-α, IL-1, IL-6. • Chemoattractants for Neutrophils and Eosinophils. • Enzymes • tryptase, chymase, cathepsin. • Changes in connective tissue matrix, tissue breakdown. Type I Hypersensitivity Secondary mediators formed after activation • Leukotrienes • Prostaglandins • Th2 cytokines- IL-4, IL-5, IL-13, GM-CSF Continuation of sensitization cycle • Mast cells control the immediate response. • Eosinophils and neutrophils drive late or chronic response. • More IgE production further driven by activated Mast cells, basophils, eosinophils. Continuation of sensitization cycle Eosinophils • Eosinophils play key role in late phase reaction. • Eosinophils make: • enzymes, • cytokines (IL-3, IL-5, GM-CSF), • Lipid mediators (LTC4, LTD4, PAF) • Eosinophils can provide CD40L and IL-4 for B cell activation. Localized anaphylaxis • Target organ responds to direct contact with allergen. • Digestive tract contact results in vomiting, cramping, diarrhea. • Skin sensitivity usually reddened inflamed area resulting in itching. • Airway sensitivity results in sneezing and rhinitis OR wheezing and asthma. Systemic anaphylaxis • • Systemic vasodilation and smooth muscle contraction leading to severe bronchiole constriction, edema, and shock. Similar to systemic inflammation. Treatment for Type I Pharmacotherapy • Drugs – – – – Non-steroidal anti-inflammatories Antihistamines block histamine receptors. Steroids Theophylline OR epinephrine -prolongs or increases cAMP levels in mast cells which inhibits degranulation. Treatment for Type I Immunotherapy • • Desensitization (hyposensitization) also known as allergy shots. Repeated injections of allergen to reduce the IgE on Mast cells and produce IgG. Treatment for Type I Effect of allergy shots Allergen Specific Antibodies Hypersensitivity Type II: Antibody-Mediated Cytotoxic Hypersensitivity • Players – Cell-surface antigens – Antibodies IgM, IgG • Inappropriate response – Normally: eliminate foreign cells – But: autoimmunity, or when foreign cells should be tolerated Type II: Mechanism Antigen on cell surface Antibody bind to antigens 1. Activate complements membrane attach complex 2. Antibody-dependent cell-mediated cytotoxicity (ADCC) cytotoxic cells with Fc receptors bind to Fc region of antibodies on cell 3. Opsonization phagocytosis Type II: Example - Autoimmunity • Goodpasture’s Syndrome • Antigen = α3 chain of basement membrane collagen – Found in kidneys and lungs • Auto-antibodies binds to α3 on own cells crosslink Fc receptors on cytotoxic cells activates monocytes, neutrophils, tissue basophils chemokines rescuit more neutrophils self tissue destruction Type II: Example - Autoimmunity From: Dokkyo Medical University http://www.dokkyomed.ac.jp/dep-k/cli-path/a-super/vasculitis/vashtml/vas-63.html Type II: Example – Foreign Antigen • Transfusion reaction ABO blood-group incompatibility From: http://www.collectmedicalantiques.com/images/bloodletting/4_transfusion.jpg TYPE II Hypersensitivity Antibody mediated cytotoxicity Blood Transfusion reactions Innocuous antigens on red blood cells EXAMPLE: ABO blood group antigens ABO Blood Groups • Antibody against RBC antigen binds and mediates killing of RBCs via C’or ADCC causes systemic inflammation. TYPE II Antibody mediated cytotoxicity Drug reactions • Drug binds to RBC surface and antibody against drug binds and causes lysis of RBCs. • Immune system sees antibody bound to "foreign antigen" on cell. ADCC Drug-induced Thrombocytopenic Purpura TYPE II Hemolytic disease of newborn Rh factor incompatibility • IgG Abs to Rh an innocuous RBC antigen – Rh+ baby born to Rh- mother first time fine. 2nd time can have abs to Rh from 1st pregnancy. – Ab crosses placenta and baby kills its own RBCs. – Treat mother with Ab to Rh antigen right after birth and mother never makes its own immune response. TYPE II Rh factor incompatibility Hypersensitivity Type III: Immune Complex-Mediated Hypersensitivity Adapted from: Kuby Immunology, Sixth Edition Type III: Immune Complex-Mediated Hypersensitivity • Players – Soluble antigens – Antibodies IgG – Complements Inappropriate response – Normally: antibody-antigen immune complex helps antigen phagocytosis + clearance – But: when large amount of complexes present tissue damage Type III: Localized Reaction Also called “Arthus reaction” Previously sensitized host Antigen exposure to specific site (ex. Inhalation, injection, etc.) Immunoglobuin-antigen complex (IgG) 1. Complement activation (C3a/C5a anaphlytoxins, chemotactic agents, membrane attack complex) 2. Bind Fc receptor on leukocytes (lytic enzyme secretion, phagocytosis) Type III: Localized Reaction • Similar to type I hypersensitivity except for – IgG, complement activation, inflammation, phagocytosis TYPE III Antigen antibody immune complexes IgG mediated Immune Complex Disease • Large amount of antigen and antibodies form complexes in blood. • If not eliminated can deposit in capillaries or joints and trigger inflammation. Type III (Immune Complex) Reactions • IgG antibodies and antigens form complexes that lodge in basement membranes. Type III Hypersensitivity Autoimmunity TYPE III Immune Complexes • PMNs and macrophages bind to immune complexes via FcR and phagocytize the complexes. BUT • If unable to phagocytize the immune complexes can cause inflammation via C’ activation C3a C4a, C5a and "frustrated phagocytes". TYPE III Immune Complex Disease "Frustrated Phagocytes” • If neutrophils and macrophages are unable to phagocytize the immune complexes these cells will degranulate in the area of immune complex deposition and trigger inflammation. • Unable to eat -------try to digest outside cell. Type III: Localized - Example From: Rocking J Farm http://www.rockinjfarm.com/images/hay.jpg • Extrinsic allergic alveolitis: “Farmer’s Lung” • Spores of thermophilic actinomycetes in dry and dusty moldy hay inhale large amount initial exposure leads to circulating IgG repeated exposures produce IgG-antigen complex in lungs pneumonitis + alveolitis Type III: Generalized Reaction Systemic exposure to antigen (ex. Blood stream) Large amount of antigen load compared to amount of IgG Small IgG-antigen complexes Difficult to clear Circulate and become deposited all over body Tissue damage (same effector mechanism as localized reaction) Type III: Generalized – Foreign Antigen • Serum sickness • Intravenous injection of antitoxins/antivenins (ex. developed from immunizing a horse) 7-10 days B cell priming + class-switch to IgG against foreign serum proteins IgG-antigen complexes circulating in blood – Joints arthritis – Skin rash – Kidneys glomerulonephritis From: Encyclopaedia Britannica http://student.britannica.com/comptons/art56794/A-scientist-collects-venom-from-a-snake Serum Sickness TYPE III Immune Complex Disease Localized disease • Deposited in joints causing local inflammation = arthritis. • Deposited in kidneys = glomerulonephritis. Type III: Generalized – Self Antigen • Autoimmunity: systemic lupus erythematosis • Environmental trigger (ex. UV) cell death impaired apoptic cell clearance nuclear proteins + DNA exposed in circulation auto-antibodies against nuclear components B cell priming + class-switch to IgG circulating self IgG-self antigen immune complexes Hypersensitivity Delayed type hypersensitivity Th1 cells and macrophages • DTH response is from: – Th1 cells release cytokines to activate macrophages causing inflammation and tissue damage. – Continued macrophage activation can cause chronic inflammation resulting in tissue lesions, scarring, and granuloma formation. • Delayed is relative because DTH response arise 24-72 hours after exposure rather than within minutes. Type IV: Delayed-Type Hypersenstivity • Major players – T helper 1 – Macrophages • Inappropriate response – Normally: necessary immune protection against intracellular pathogens – But: prolonged response leads to extensive tissue destruction Stages of Type IV DTH Sensitization stage • Memory Th1 cells against DTH antigens are generated by dendritic cells during the sensitization stage. • These Th1 cells can activate macrophages and trigger inflammatory response. Type IV: Sensitization Phase First exposure to antigen Antigen-presenting cell (dendritic cells, macrophages) MHC II presentation Naïve CD4+ T cells Activated, antigen-specific T helper 1 cells • Time frame = 1-2 weeks • Primary response established Stages of Type IV DTH Effector stage • Secondary contact yields what we call DTH • Th1 memory cells are activated and produce cytokines. – IFN-γ, TNF-α, and TNF-β which cause tissue destruction, inflammation – IL-2 that activates T cells and CTLs – Chemokines- for macrophage recruitment. – IL-3, GM-CSF for increased monocyte/macrophage Stages of Type IV DTH Effector stage Secondary exposure to antigen • Inflamed area becomes red and fluid filled can form lesion. – From tissue damage there is activation of clotting cascades and tissue repair. • Continued exposure to antigen can cause chronic inflammation and result in granuloma formation. Type IV: Effector Phase Second exposure Memory T helper 1 activated Effector T helper 1 Inflammatory cytokines (ex. IFN) Chemokines for phagocyte recruitment More activated macrophages to exposure site • At exposure site – Mostly non-specific inflammatory cells(ex. Macrophages) – Few antigen-specific cells (ex. T cells) Type IV: Effector Phase Problematic consequence (ex. Mycobacterium tuberculosis) bacteria cannot be cleared Granuloma formation Continuous macrophage + T helper 1 activation High lytic enzyme secretion Tissue damage Granuloma Formation from DTH Mediated by Chronic Inflammation Type IV DTH Contact dermatitis • The response to poison oak is a classic Type IV. – Small molecules act as haptens and complex with skin proteins to be taken up by APCs and presented to Th1 cells to get sensitization. – During secondary exposure Th1 memory cells become activated to cause DTH. Contact dermatitis Type IV: Examples • Contact dermatitis – Small molecules (ex. Nickel) bind to skin protein able to be presented and recognized by T cells From: Mayo Clinic http://www.mayoclinic.com/health/nickel-allergy/DS00826/DSECTION=causes Type IV (Cell-Mediated) Reactions • Delayed-type hypersensitivities due to TD cells • Cytokines attract macrophages and initiate tissue damage Type IV: Examples • Mantoux Test (Mycobacterium tuberculosis) – Tuberculin (purified protein derivative) intradermal injection 48-72 hours swelling – Swelling = previous exposure/sensitization – No swelling = no previous exposure/sensitization From: Centers for Disease Control and Prevention – Public Health Image Library Type IV DTH Drug reactions can be any Type of Hypersensitivity Section B Autoimmunity What is Autoimmunity? • Autoimmunity is an immune response to self antigens that results in disease. • The immune response to self is a result of a breakdown in immune tolerance. Immune Tolerance • Tolerance of self is a hallmark of adaptive immune response. • B cell tolerance vs. T cell tolerance. B cell Tolerance No T cell help • Autoreactive B cells that enter lymph node should fail to get costimulation from T cells and therefore never enter primary follicles. Maintenance of T cell tolerance • Clonal deletion – negative selection in the thymus, deletion in the periphery. • Sequestration of antigens – Inside nucleus – Inaccessible to immune system (brain, eye, testes) • Immunological ignorance – self antigens at low density on APCs – or T cells do not cross barrier. Maintenance of T cell tolerance • Anergy – Lack of co-stimulation or second signal to T cells results in anergy. • Suppression – T-cell cytokine mediated suppression. – Regulatory T cells. CD4+CD25+ CTLA4+ T cells that produce suppressive cytokines. Inducing Autoimmunity OR Breaking of self-tolerance Injury (inflammation) or Infection "Viral Trigger" is term for virus infection leading to autoimmune response. Inducing Autoimmunity Breaking of self-tolerance • Release of sequestered antigens: Tissue damage by infection may allow access of T cells and B cells to sequestered antigens. • Antigenic (molecular) mimicry is when similarity between foreign antigen and self protein results in cross-reactivity. Antigenic Mimicry Breaking of self-tolerance • Inappropriate expression of Class II MHC. – Abnormal expression of class II molecules can lead to presentation of self antigens that were not presented in thymus or periphery. – "non-APC" becomes APC with inflammation. Classification of autoimmune diseases Autoantibody or T cell mediated autoimmune diseases Antibodies to RBC antigens Autoantibodies to surface receptors Graves' disease =hyperthyroid Stimulating autoantibodies bind thyrotropin receptor for thyroid stimulating hormone. Myasthenia Gravis Blocking Autoantibodies Antibodies to acetyl choline receptors block muscle activation and trigger Inflammation that causes the destruction of the nerve/muscle junctions resulting in paralysis. Autoantibodies to surface receptors Blocking autoantibodies • Hashimoto's thyroiditis =hypothyroid – Blocking autoantibodies inhibit thyroid function. Goodpasture's Syndrome • Autoantibodies to type IV collagen and noncollagenous basement membrane • Antibodies bind in lung and kidney causing inflammation and destruction. Rheumatoid Arthritis Immune Complex Disease • Autoantibodies to ubiquitous antigens – IgM against IgG is called "rheumatoid factor" – IgG against glucose-6-phosphate isomerase. • Primary disease manifestation – immune complexes get deposited in joints and trigger inflammatory response. – Complement and FcγRs play large role. Systemic lupus erythematosus (SLE) Immune complex disease • Chronic IgG production to intracellular proteins. • Disease symptoms are widespread and varied. – kidney damage, lung disease, skin, eye, etc. Systemic lupus erythematosus (SLE) • Autoantibodies against nucleoprotein particles: – Nucleosome – Spliceosome – Ribonucleoprotein complexes • Th response to one epitope can drive auto Abs. Systemic lupus erythematosus (SLE) Lupus • One T helper epitope can provide help to multiple antibody epitopes in the same particle Potential disease cycle for SLE • Immune complexes form – get deposited in joints, small blood vessels C' activation, activation of phagocytes – Inflammation/damage causes more release of intracellular antigens and then – MORE immune complexes can form T cell Mediated Autoimmune Diseases Multiple sclerosis (MS) • T cell responses to myelin basic protein (MBP). • The destruction of the myelin sheath results in neurological symptoms Multiple sclerosis (MS) • The cause remains unknown, but autoimmunity possibly triggered during an inflammatory response to a viral infection is implicated. • MBP has high sequence homology with measles protein and Hepatitis B virus protein. Antigenic mimicry? Insulin-dependent (type I) diabetes mellitus (IDDM) Type I diabetes • Selective destruction of insulin-producing β cells in the islets of Langerhans of the pancreas. • Autoantibodies and self-reactive T cells have been found in human patients with IDDM. Type I diabetes Specific killing of insulin producing β islet cells Diabetes • CD8+ CTLs are thought to be responsible for the actual killing of the islet cells. • Autoantibodies are present in IDDM. – However, animal models of IDDM have shown that these autoantibodies alone cannot cause IDDM. Susceptibility Factors MHC • Relative Risk--- ratio of having a specific MHC allele increases risk for that disease. – e.g. Ankylosing spondylitis, an inflammatory disease of the vertebral joints, the RR with HLA-B27 is 87. MHC Risk for Diabetes (IDDM) • The relative risk associated with having the DR3/DR4 combination is 25:1 Susceptibility Factors Gender • Increased risk associated with gender. – e.g. Female to male ratio for • • • • SLE 10:1 MS 5:1 Hashimoto's thyroiditis 4:1 But IDDM is 1:1 and AS is 0.3:1. Susceptibility Factors Immune regulation genes • Increased risk associated with changes in expression of immune regulation genes. • Decreased expression of Fas, FasL, assoc with SLE. • Decreased amount of Complement proteins (C1, C2, C4) has been assoc with SLE. Susceptibility Environmental factors • Smoking has been associated with Goodpasture's syndrome. – Potentially the damage to lung basement membrane helps trigger autoimmune response. • Pollution, occupational exposure, etc. Treatment of Autoimmune Diseases • Pharmacotherapy – Anti-inflammatories--steroids or NSAIDS. – Other specific drugs for symptoms e.g. insulin • Possible Immunotherapies – Block co-stimulation – Peptide vaccines. Inject peptides to block MHC and prevent self peptides from binding. – Oral Tolerance. MBP ingested to induce tolerance. Section C Immunodeficiencies Host Defense Mechanisms • Skin and mucosal barriers • Humoral immunity (B cells, plasma cells, Ab) • Cell-mediated immunity (T cells) • Phagocytosis • Complement Suspecting Immunodeficiency • Look for infections that are: – – – – – – Frequent Recurrent/chronic Unusual organisms Organisms that respond poorly to therapy Growth retardation Family history Suspecting Immunodeficiency • Humoral (antibody) deficiency associated with: – Recurrent infections with encapsulated bacteria – Chronic sinupulmonary infections • Cell-mediated deficiency characterized by: – Recurrent infections with • • • Viruses Fungi Opportunistic organisms (PCP) – Diarrhea, wasting, growth retardation • Combined immunodeficiency Humoral Immunodeficiency (B cells) Humoral Immunodeficiency (B cells) • Transient hypogammaglobulinemia of infancy – – – – • Slow to develop normal levels of antibody Asymptomatic, minor infections Low levels of IgG, IgA (IgM usually normal) Resolves by 3-6 yo IgA deficiency – – – – – – Most common humoral antibody deficiency 50-80% asymptomatic Recurrent sinopulmonary infections most frequent manifestation May have severe malabsorption (chronic diarrhea) Isolated low IgA level Increased risk of autoimmune disorders Bruton’s X-linked Agammaglobulinemia • No B cells • Child clinically well for first 6 months of life • Recurrent upper/lower respiratory tract infections with encapsulated bacteria (S. pneumo, H.flu) – Bronchiectasis chronic cough/increased sputum • • • • Sepsis, meningitis, skin infections Paucity of lymphoid tissue (tonsils, adenoids) Markedly decreased IgG, IgA, IgM Treatment: IVIG, antibiotic therapy Common Variable Immunodeficiency • B lymphs don’t differentiate into plasma cells • Recurrent sinopulmonary infections • Low IgG, IgA, IgM • Treatment: IVIG • Associated with autoimmune disease, lymphoma Cellular Immunodeficiency (T cell) DiGeorge Syndrome • No T cells secondary to thymic hypoplasia • “CATCH 22” • Overwhelming infections with viruses, fungi, bacteria • Treatment: correct hypocalcemia, cardiac defects, fetal thymus transplant Combined Immunodeficiency SCID • Defects in stem cell maturation • Adenosine deaminase deficiency (toxic insult to T and B cells) • Manifestations seen in first 3 months of life – Recurrent, severe bacterial, viral, fungal, and protozoan infections (usually respiratory infections) – Failure to thrive, diarrhea, dermatitis, candidiasis • Most have lymphopenia, decreased IgG, IgA, and IgM – Diagnosis made by analysis of T, B, and NK cell subsets • Treatment: isolation, treat underlying infections, bone marrow transplant Wiskott-Aldrich Syndrome • X-linked recessive • Symptoms in infancy – Recurrent, severe infections – Eczema – Thrombocytopenia (petechiae) • Low levels of IgM • Increased risk for hematologic malignancy • Treatment: manage bleeding/infections, BMT Ataxia Telangiectasia • Autosomal recessive deficiency in DNA repair affecting T and B cells • Progressive ataxia, telangiectasia, variable immunodeficiency (recurrent sinopulmonary infections common) • Increased risk of malignancy (leukemia, lymphoma) Hyper IgE (Job) syndrome • Autosomal recessive • Symptoms/signs – Coarse facial features/skeletal abnormalities – Recurrent staph infections • • Impetigo (resistant) Pneumonia with pneumatocele formation – 3 E’s: Elevated IgE, Eosinophilia, Eczema Hyper IgM Syndrome • T cell abnormality preventing IgM IgG • X-linked recessive (males 6 mo-1 year) • Frequent sinopulmonary infections, diarrhea, opportunistic infections (PCP) • Low levels of IgG/IgA, high levels of IgM • Treatment: Ig replacement HIV • Retrovirus infecting CD4 + cells – Vertical transmission, breastmilk, sex • Wide range of clinical manifestations – Failure to thrive, fevers, night sweats, malaise, recurrent thrush, recurrent bacterial infections • Decreased CD4 count, may have elevated Ig Acquired Immunodeficiency Syndrome (AIDS) Structure of HIV-1 gp120 gp41 Envelope env Protease Reverse Trascriptase Integrase pol Matrix (p17) gag Genome Capsid (p24) Serological Profile Kuby, 2007 Immunological Abnormalities • Infection and destruction of dendritic cells, macrophages and Th cells • Late decrease in Th cell numbers (200/mm3 blood) Phagocytic Disorders Chronic Granulamatous Disease (CGD) • Defective NADPH oxidase • 75% X-linked recessive, 25% autosomal recessive • Severe, recurrent staph aureus infections of lymph nodes, and skin (granulomas, heal slowly), pneumonitis, osteo, hepatosplenomegaly • Dx: Nitroblue tetrazolium (NBT) test • Treatment: antimicrobial prophylaxis, IFNgamma, BMT Leukocyte adhesion deficiency (LAD) • Deficient chemotaxis • Recurrent soft tissue, skin, respiratory infections, impaired wound healing (typically no pus, minimal inflammation) • Delayed umbilical separation • Increased WBC count • Treatment: BMT Complement System Disorders • Defects of early components (C1-C4) associated with infections with encapsulated bacteria – Present similarly to humoral immune deficiencies • Defects of late components (C5-C9) associated with Neisseria infections • Also associated with autoimmune-like conditions • CH50 functional assay assesses entire complement cascade – Also may use individual components • Treatment: treat infectious and autoimmune sequelae Summary • Primary immunodeficiencies are inherited • They can affect hematopoietic stem cells, lymphoid or myeloid cells. • Secondary immunodeficiencies are due to infections, aging, cancer or chemical exposure • HIV affects immune system by eliminating CD4+ T cells