Integrating Didactic and Clinical Education

Athletic Training Clinical
Proficiencies
By
Sue Shapiro, Ed.D.,L/ATC
Clinical Coordinator/Assistant Professor
Barry University
Miami Shores, Florida
Objectives
Implementation of clinical proficiencies
Linking the didactic and clinical components
Clinical proficiency delineation
Integrative evaluation strategies/tools
Competency-Based Objectives
Nothing becomes real for the student until it is EXPERIENCED
CROSSING THE
BRIDGE
HOURLY
BASED
COMPENTENCY
BASED
Competency-Based Instruction
Identifies the professional roles students will assume upon completion
Determines what constitutes effective performances within these roles
Learning Cognitive
Information in Isolation
Merging of Didactic and
Clinical Components
Flexible Clinical Scheduling is a Prerequisite to
Competency-Based
Progression
Flexible Clinical
Scheduling Should:
Provide open laboratory practice
Encourage advanced students to practice and teach fellow students in a controlled environment other than the clinical setting
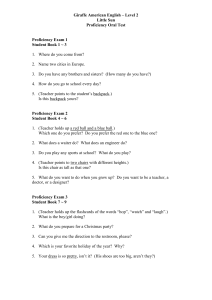
Clinical Proficiency
Preparation
First Phase
Formulate a student portfolio
Student Portfolio Matrix
Clinical Proficiency
Preparation
Second Phase
Formulate a matrix of the didactic courses in the athletic training program
Didactic Course Matrix
Didactic Course Matrix
Clinical Proficiency
Preparation
Third Phase
Formulation of Clinical Hours
Matrix
Clinical Hours Matrix
Clinical Proficiency
Preparation
Fourth Phase
Clinical Proficiency Matrix
Clinical Proficiency Matrix
Clinical Proficiency Matrix
Clinical Proficiency Matrix
Clinical Proficiencies
Individual skills
Subset skills taught together
Lower Extremity Clinical
Proficiency
Individual Subset Skills:
Pelvic obliquity
Tibial torsion
Hip anteversion and retroversion
Genu valgum,varum, and recurvatum
Rearfoot valgus and varus
Forefoot valgus and varus
Pes cavus and planus
Foot and toe posture
Grouped Subset Skills:
Lower Extremity
Postural Deviations and Predisposing
Conditions
Good Posture Part Faulty Posture I NI l. Legs are straight up and down.
Knees and legs 1. Knees touch when feet are apart
( genu valgum)
2. Patellae face straight ahead when feet are in good position
3. Looking from the side the knees are straight (i.e. neither bent forward nor “ locked ” backward) l. In standing, the longitudinal arch has the shape of a half dome
2. Barefoot or in shoes without heels, the feet toe-out slightly
3. In shoes with heels, the feet are parallel
Feet
2. Knees are apart when feet touch ( genu varum)
3. Knee curves slightly backward ( hyperextension knee or genu recurvatum)
4. Knee bends slightly forward or not as straight as it should be
( flexed knee)
5. Patellae facing slightly toward each other ( medial rotated femurs and/or snake eyes)
6. Patellae facing slightly outward ( lateral rotated femurs and/or frog eyes) l . Low medial longitudinal arch or flatfoot ( pes planus)
2. High medial longitudinal arch
( pes cavus)
3. Weight borne on the inner side of the foot making ankle roll in ( pronation)
4. In walking the feet are parallel and the weight is transferred from the heel along the outer border to the ball of the foot
5. In running, the feet are parallel or toe-in slightly. The weight is on the balls of the feet and toes because the heels do not come in contact with the ground
1. Toes should be straight, neither curled downward nor bent upward
2. Toes should extend forward in line with the foot and not be squeezed together or overlap
Toes
4. Weight borne on the outer border of the foot or the ankle rolls out ( supination)
5. Toeing-out while walking or standing ( forefoot valgus, outflared or slue-footed)
6. Toeing-in while walking or standing ( forefoot varus or pigeon-toed)
7. Posterior calcaneus rolls inward ( rearfoot valgus)
8. Posterior calcaneus rolls outward ( rearfoot varus) l. Toes bend up at the first joint and down at middle and end joints so that the weight rest on the tips of the toes ( hammer toes)
2. Big toe slants inward toward the midline of the foot ( hallus valgus)
3. Second toe longer than 1 st
( morton foot) toe
•
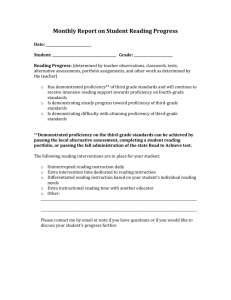
Pelvic Obliquity
Purpose: To identify abnormal pelvic alignment that can lead to leg length discrepancies.
Proper Identification Procedures for Pelvic Obliquity:
The ACI will observe the student athletic trainer performing a pelvic obliquity check.
Patient should be bare foot with the knees fully extended and the feet together.
The ASIS and iliac crest should be exposed for viewing
Ask the athlete to stand facing away from the examiner
Examiner places a finger or two of each hand on each of the athlete ’ s iliac crests and imagines a line drawn between the two crest
Pelvic obliquity is present when this imaginary line is not parallel to the floor
Leg length discrepancies should be investigated at this point
Completed Pelvic Obliquity Observation Pass Fail
• Hip Anteversion and Retroversion
Purpose: To identify abnormal rotational malalignments of the femur in relation to the femoral neck.
Proper Testing for Femoral Rotation The ACI will observe the student athletic trainer performing observational and orthopedic testing of the hip for anteversion and retroversion.
P NP
The athlete should be viewed from the front with the knees facing forward. The examiner should observe abnormal toeing in or toeing out of the feet. An athlete with increased femoral anteversion tends to stand with the limb in an internally rotated position, producing in- toeing. While the athlete with decreased femoral anteversion or femoral retroversion tend to stand with the limb in an externally rotated position, producing out-toeing.
Next, perform a Craig ’ s Test to estimate the amount of femoral anteversion present.
The athlete is placed prone with the ipsilateral knee flexed to 90 degrees.
The examiner palpates the lateral prominence of the greater trochanter with one hand while controlling the rotation of the limb with the other.
An imaginary vertical line serves ad the reference for this test. The limb is then rotated until the lateral prominence of the greater trochanter is felt to be maximal.
The angle made between the axis of the tibia an the vertical is considered an approximation of the femoral anteversion. Normal anteversion is between 8 degrees and 15 degrees.
Completed Testing for Anteversion and Retroverson Pass Fail
Important Aspects of
Proficiency Delineation l. The process is descriptive and not prescriptive
2. Assignment of importance of each subset in the delineation
Important Aspects of
Proficiency Delineation
3. Assignment of Successful Mastery of
Clinical Skill
% of Mastery needed to pass
Particular subsets that must be completed
# of times a student can attempt test
Should students be allowed to progress to next level if he/she doesn ’ t successfully complete proficiencies at one level
Integrating Components
INTEGRATED COMPONENTS
INTEGRATING COMPETENCY
BASED CLINICAL EDUCATION
Competency based clinical education is a group effort
Don ’ t want student to become check off artist
Team Teaching
The coordinated and cooperative planning, teaching, supervision, and evaluation of a group of learners by 2 or more instructors, each having special competencies and knowledge in a specialized area.
Success of Team
Teaching Depends on
Instructors working in cooperation and communicate as allies
Everyone involved is responsible for developing the objectives, instructional methodologies and evaluation
Multiple instructors can evaluate clinical competencies with high degree of consistency
INTEGRATING COMPETENCY
BASED CLINICAL EDUCATION
Competency based clinical education is a group effort
Don ’ t want student to become check off artist
Student ’ s need to be able to
THINK-IN-ACTION
Students need to learn to
THINK -IN-ACTION
&
REASON-IN TRANSITION
LINKAGE OF EVALUATING
SKILLS
Experiential learning does not occur without active participation
It requires:
Engagement in the situation
Problem Solving
Integrative Evaluation Tools
NARRATIVES
ALGORITHM
Algorithm Evaluation
Blueprint or diagrams that lead a student through a step by step process of how to perform a certain set of tasks in an organized fashion taking into account that the procedure will change or take a different path based on the finding at any giving point
INTEGRATING COMPETENCY
BASED CLINICAL EDUCATION
Don ’ t want student to become check off artist
Student ’ s need to be able to THINK-IN-
ACTION
Emphasizing linking process and content
LINKING PROCESS
AND CONTENT
CONTENT PROCESS
INTEGRATING COMPETENCY
BASED CLINICAL EDUCATION
Don ’ t want student to become check off artist
Student ’ s need to be able to THINK-IN-
ACTION
Emphasizing linking process and content
Individualization is very important in competency based programs
INDIVIDUALIZATION
CLINICAL
COMPONENT
=
Individual
Abilities
+
Learning Styles
Individualization
Allows each student to go through the integrative process:
At his/her own content level
Pace the learning at their own rate of speed.
The Sculpturing of a
Professional