Emergency Action Planning
advertisement

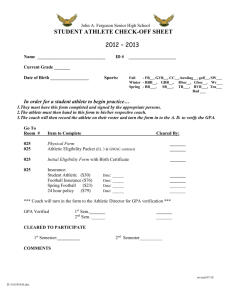
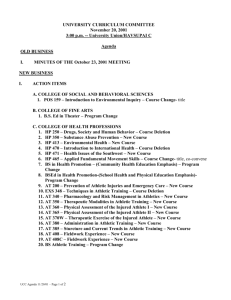
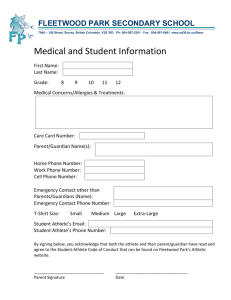
Emergency Action Planning Why? Chaos – Emergencies are never planned – There are always “wild cards” in certain situations The more prepared you are for an emergency situation, the better the reaction Why? Professional Need – NCAA has recommended that all member institutions develop an emergency plan for their athletic programs 2001 survey of NCAA institutions revealed that at least 10% do not maintain an emergency plan The same survey revealed that 1/3 of institutions do not maintain plans for off-season strength and conditioning activities – The National Federation of State High School Associations has recommended the same for secondary schools. Why? Legal Need – Organizational medical personnel, including certified athletic trainers have a duty to ensure high-quality care of athletic participants – Gathers v Loyola Marymount University Settlement included a statement that care was delayed for the injured athlete, and the defendants acted negligently and carelessly in not providing an appropriate medical response – Kleinknecht v Gettysburg College Court ruled that the college owed a duty to the athletes who are recruited to play at the school That duty included “prompt and adequate emergency services while engaged in the school-sponsored intercollegiate athletic activity for which the athlete has been recruited” Components Athletic injuries may occur at any time and during any activity – Does not always involve impact sports – The athletic trainer may not always be the first responder Management involves: – – – – – Athletic trainers Student AT’s Emergency Medical Personnel Physicians Coaches Implementation Implementation of the EAP Step 1 : Written Down * Continuity * Modified for different athletic venues * Location and type of equipment modified based on location Implementation Implementation of the EAP Step 2 : Education * Must include all members * Written copy to all possible members * Must be posted by all telephones Implementation Implementation of the EAP * Step 3 : Rehearsal * Provides team members chance to maintain competent skills * Allows communication between ATC’s and emergency personnel * Annual in-service / spring game * Take into account turnover of personnel Personnel It is imperative that the EAP outline who is responsible for summoning help and clearing the uninjured from the area CPR / First Aid / AED Certification Equipment Good operating condition – Regular inspections (splints, etc.) – Batteries for AED – Available at each venue Communication Must have access to a working telephone or a two way radio-DO NOT ALWAYS RELY ON A CELL PHONE!!!!! Established equipment and helmet removal policies and procedures before an emergency happens Who accompanies the athlete to the ER? Communication What do I need to know before I call EMS? 1) 2) 3) 4) 5) 6) type of emergency suspected injury present condition current assistance location of phone being used location of emergency **Most importantly make sure you stay on the line until the EMS dispatcher says otherwise!** Communication Paperwork, paperwork, paperwork,Importance of having current paperwork(provided at start of school year) on all athletes. With no informed consent, consent implied on part of athlete to save athlete’s life Transportation Emphasis must be placed on having an ambulance on site at high risk events Response Time – parents transporting Venue Location Emergency Action Plan should be venue specific Plan should encompass accessibility to emergency personnel, communication systems, equipment and transportation Home Teams : Communicate Visiting Teams : Familiarize Timber Creek High School 2 Gyms (Large and small) Wrestling Room Tennis Courts – 4 courts with easy street access 1 baseball fields and 1 softball fields Game field (sub varsity football / soccer games / track) 3 ½ Practice Fields (football , soccer) KISD Stadium – Varsity football games played on Keller High School campus Five Emergency Action Plans Timber Creek High School Five Different Emergency Action Plans Plans are printed in Policies and Procedures Manual issued to each coach Plans are also printed and posted at each venue near fixed phone line Timber Creek High School Implementation – Student AT’s get CPR/AED certified before they begin working FB practice at the beginning of each school year. – Review session at beginning of each season with coaches during CPR/First Aid Training. Timber Creek High School Equipment – Splints – Crutches – AED ‘s Centrally located in each athletic venue – Spineboard Policy – Biohazard Materials Timber Creek High School Communication – Fixed telephone lines in : AT Rooms Coaches Offices – Cell phones – Two way radios at each venue with administrators / game administrators Timber Creek High School Transportation – Golf Cart at outside venues – Gates for ambulance entry – Directions to side door for easy gymnasium entry if needed Timber Creek High School Venue Location – Specific to each location, circumstances, entry points and communication available Emergency Action Planning Venue Map School Map Example of Emergency Action Plan “Curve Balls” Gates and keys Parents calling EMS Parents, in general Absence of parents Crowd Control Response Time Weather – – – – Need to have EAP’s for events when weather threatens Evacuation to safe areas for all (1) players (2) spectators and (3) officials Notification of these threats Need to clarify who makes this call Notification Notification depends on district policies – Principal – AD – Assistant AD – Head Athletic Trainer – Athletic Coordinator – Superintendent Documentation Document, document, document Best if we document when it is fresh on our minds to avoid mistakes – Little Note Pad – Computer Program – Paper Copies Principles of Assessment Appropriate acute care cannot be provided without an assessment done on the field On-field assessment – Determine nature of injury – Decide on a plan - direction of treatment – Divided into primary and secondary survey Primary survey Performed initially to establish presence of life-threatening condition -Life threatening injuries take precedents Airway, breathing, circulation, shock and severe bleeding Used to correct life-threatening conditions The Unconscious Athlete Must be considered to have lifethreatening condition – Note body position and level of consciousness – Check and establish vitals; (look, listen, and feel for pulse) then start compression, airway, breathing, (CAB) – may need to log roll – Assume neck and spine injury – Remove helmet only after neck and spine injury is ruled out (facemask removal will be required in the event of CPR) Secondary survey Life-threatening condition ruled out Determine injury severity and transportation from field Perform a more detailed evaluation of conditions that do not pose lifethreatening injuries -sometimes done on the field and other times it can wait till the athlete is off the playing field Off-Field Assessment Performed by athletic trainer or physician once athlete has been removed from site of injury Divided into 4 segments – History – Observation – Physical examination – Special tests Off-Field Assessment History – Obtain information about injury – Listen to athlete and how key questions are answered Visual Observation – Inspection of injured and non-injured areas – Look for gross deformity, swelling, skin discoloration Off-Field Assessment Palpation – Assess bony and soft tissue – Systematic evaluation beginning with light pressure and progressing to deeper palpation – beginning away from injured area Special Test – Designed for every body region for detecting specific pathologies – Used to substantiate findings from other testing Immediate Treatment Following Acute Injury Primary goal is to limit swelling and extent of hemorrhaging If controlled initially, rehabilitation time will be greatly reduced Control via PRICE – PROTECTION – REST – ICE -COMPRESSION -ELEVATION Immediate Treatment Following Acute Injury PROTECTION -Prevents further injury -Immobilization and appropriate forms of transportation will help in protecting an injury from further damage REST -Stresses and strains must be removed following injury as healing begins immediately -Days of rest differ according to extent of injury Immediate Treatment Following Acute Injury ICE (Cold Application) -Initial treatment of acute injuries -Used for strains, sprains, contusions, and inflammatory conditions -Used to decrease pain, promote vasoconstriction -Lowers metabolism, tissue demand for oxygen and hypoxia Immediate Treatment Following Acute Injury -Ice should be applied initially for 20 minutes and then repeated every 1 - 1 1/2 hours and should continue for at least the first 72 hours of new injury -Treatment must last at least 20 minutes to provide adequate tissue cooling and can be continued for several weeks Compression -Decreases space allowed for swelling to accumulate Immediate Treatment Following Acute Injury -Important adjunct to elevation and cryotherapy and may be most important component -A number of means of compression can be utilized (Ace wraps, foam cut to fit specific areas for focal compression) -Compression should be maintained daily and throughout the night for at least 72 hours (may be uncomfortable initially due to pressure build-up) Immediate Treatment Following Acute Injury Elevation -Reduces internal bleeding due to forces of gravity -Prevents pooling of blood and aids in drainage -Greater elevation = more effective reduction in swelling Moving and Transporting Injured Athletes -Must be executed with techniques that will not result in additional injury -No excuse for poor handling -Planning is necessary and practice is essential -Additional equipment may be required Suspected Spinal Injury -Coach should access EMS immediately and wait for rescue squad before attempting to move athlete -Transportation and movement should be left to trained experts -Maintain head and neck in alignment with long axis of body Suspected Spinal Injury Placing Athlete on Spine Board – EMS should be contacted if this will be required – Must maintain head and neck in alignment of long axis of the body – One person must be responsible for head and neck at all times – Primary emergency care must be provided to maintain breathing, treating for shock and maintaining position of athlete Suspected Spinal Injury Suspected Spinal Injury Ambulatory Aid – Support or assistance provided to injured individual to walk – Prior to walking, serious injury should be ruled out along with further injury with walking – Complete and even support should be provided on both sides by individuals of equal height when providing ambulatory aid – Arms of athlete are draped over shoulders of assistants, with their arms encircling his/her back Basket Carry – Used to move mildly injured athlete a greater distance than could be walked with ease – Carrying the athlete can be used – following a complete examination – Convenient carry is performed by two people Basket Carry Stretcher Carry – Best and safest mode of transport – With all segments supported/splinted athlete is lifted and placed gently on stretcher – Careful examination is required if stretcher is needed – Various injuries will require different positioning on stretcher Proper Fit and Use of Crutches -When lower extremity ambulation is contraindicate a crutch or cane may be required -Faulty mechanics or improper fitting can result in additional injury or potentially falls -Fitting athlete – Athlete should stand with good posture, in flat soled shoes – Crutches should be placed 6” from outer margin of shoe and 2” in front Proper Fit and Use of Crutches – Crutch base should fall 1” below anterior fold of axilla – Hand brace should be positioned to place elbow at 30 degrees of flexion – Cane measurement should be taken from height of greater trochanter Walking with Crutch – Corresponds to walking – Tripod method Swing through without injured limb making contact with ground – Four- point crutch gait Foot and crutch on same side move forward simultaneously with weight bearing Walking with Crutch Stair climbing should be introduced when athlete is able to move effectively on level surface (‘up with the good – down with the bad’) Questions??