Medical Record: Deep Vein Thrombosis (DVT) Case
advertisement

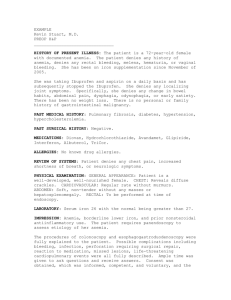
SUBJECTIVE DATA (S): IDENTIFYING DATA: Initials: P.B. Age: 76 years Race: Caucasian Gender: Male CHIEF COMPLAINT (CC): Patient c/o “leg pain and swelling x2 days”. HISTORY OF PRESENT ILLNESS (HPI): Patient states he slipped off the step of his camper and fell 2 days ago and hurt his right lower extremity. His leg started to swell and became more painful 1 day after the occurrence. Patient states that today his right lower extremity is swelling even more and feels very tight. Patient states he believes he hit his leg on one of the steps when he fell. location: right lower extremity quality: patient describes a feeling of tightness severity: patient rates pain a “5” on a scale from 1-10. He states the pain is now constant and is continuing to worsen timing: symptoms started 2 days ago setting: patient states his symptoms started after he slipped off the step of his camper 2 days ago alleviating and aggravating factors: pain in leg is worse when the patient tries to flex his lower leg and when he walks. He says it feels a little better when he is resting with his leg elevated. associated signs and symptoms: swelling, warmth, and redness in right lower extremity PAST MEDICAL HISTORY (PMH): Allergies: NKDA Current medications: altace 10 mg capsule, claritin 10 mg tablet Age/health status: 76 years Appropriate immunization status: Up to date on all vaccines; He states he had his tetanus-diptheria booster 6 years ago and has had the herpes zoster vaccine. Flu and pneumonia vaccines given October 2013. He states he will be getting the flu vaccine at his primary physician’s office this fall. Previous screening tests result: Patient states he has a yearly physical each year and has his cholesterol, PSA level, and other labs checked. All lab work was reported normal in May 2014. Colonoscopy was done at age 65 and was reported normal. Dates of illnesses during childhood: N/A Major adult illnesses: Patient states he has a history of HTN and allergic rhinitis Injuries: N/A Hospitalizations: Patient states he was in the hospital with pneumonia about 10 years ago. He explains that he receives a pneumonia vaccine every 5 years now. Surgeries: Patient denies having any surgery FAMILY HISTORY (FH): Father died at the age of 82 from an AMI. Mother died at the age of 88 from complications from Type II diabetes. Patient states he is unsure of their complete medical history. Patient has 1 sister who has HTN as well. He has 2 children who are alive and healthy at the age of 54 and 49. SOCIAL HISTORY (SH): He is married and is a retired police officer. He is independent with his ADLs and lives with his wife. He states he and his wife currently exercise about 3 times per week which includes going to the mall in the morning for brisk walking for about 1 mile. He is a former smoker- ½ pack/day but he states he quit about 30 years ago. He does drink alcohol occasionally if he is at a social event. He drinks caffeine (coffee, tea, or soda) 1-3 times daily. No illicit drug use. REVIEW OF SYSTEMS (ROS): 1. Constitutional symptoms- Patient denies fever, fatigue, chills, malaise, night sweats, unexplained weight loss or weight gain, loss of appetite. 2. Eyes- Patient denies blurred vision, difficulty focusing, ocular pain, diplopia, scotoma, peripheral visual changes, and dry eyes. Patient states he does wear corrective lenses and has for the last 20 years. Date of last eye exam was in 2013. 3. Ears, nose, mouth, and throat- Patient denies vertigo, sinus problems, headaches, epistaxis, dental problems, oral lesions, hearing loss or changes, nasal congestion, sore throat, hoarseness. Date of last dental visit was about 8 months ago. 4. Cardiovascular- Patient has a history of HTN. He states he was diagnosed several years ago but it is managed well with altace. Patient states he exercises about 3 times a week for about 30 minutes to an hour. Patient denies any history of heart murmur, chest pain, palpitations, dyspnea, activity intolerance, varicose veins, edema. Date of last EKG and cholesterol level was in May 2014 at his yearly physical and was reported normal. 5. Respiratory- Patient denies cough, SOB, difficulty breathing, wheezing, pain with inspiration, chest tightness, history of respiratory infections, exposure to TB, hemoptysis. Patient states he had a chest x-ray about 10 years ago when he was hospitalized with pneumonia. He is unsure of when his last TB skin test was done. Patient states he is a former smoker but quit about 30 years ago. 6. Gastrointestinal- Patient denies dysphagia, reflux, pyrosis, loss of appetite, bloating, nausea, vomiting, diarrhea, constipation, hematemesis, abdominal or epigastric pain, hematochezia, change in bowel habits, food intolerance, flatulence, hemorrhoids. Patient states he tries to eat healthy, well-balanced meals. 7. Genitourinary- Patient denies urgency, frequency, dysuria, suprapubic pain, nocturia, incontinence, hematuria, history of stones. 8. Musculoskeletal- Patient reports pain and swelling in the RLE. Patient denies back pain, joint pain, muscle cramps, neck pain or stiffness, changes in ROM. He states he exercises about 3 times a week. He does wear his seatbelt. 9. Integumentary- Patient reports redness and warmth of RLE. Patient denies itching, uritcaria, hives, nail deformities, hair loss, moles, open areas, bruising. Patient denies breast tenderness, masses, skin changes. 10. Neurologic- Patient denies weakness, numbness, headache, tingling, memory difficulties, involuntary movements or tremors, syncope, stroke, seizures, paresthesias. 11. Psychiatric- Patient denies nightmares, mood changes, anxiety, depression, nervousness, insomnia, suicidal thoughts, exposure to violence, or excessive anger. 12. Endocrine- Patient denies cold or heat intolerance, polydipsia, polyphagia, polyuria, changes in skin, hair or nail texture, unexplained change in weight, changes in facial or body hair, changes in hat or glove size, use of hormonal therapy. 13. Hematologic/lymphatic- Patient denies unusual bleeding or bruising, lymph node enlargement or tenderness, fatigue, history of anemia, blood transfusions. Patient is unsure of last HCT result but states all lab work was done at his last physical in May 2014 and everything was reported to him as “normal”. 14. Allergic/immunologic- Patient reports a history of seasonal allergies. He states he has always had allergies but it is now managed well with Claritin. Patient denies exposure to blood or body fluids, use of steroids, or immunosuppression in self or family. He is unsure of his last Hep B vaccine but knows he is up-to-date on all vaccines. OBJECTIVE DATA (O): 1. Constitutional- VS: Temp- 99.1, BP- 133/81, HR- 84, RR- 18, O2 sat- 99%, Height6’4”, Weight- 220 lbs, BMI- 26.78; General Appearance: healthy-appearing, wellnourished, and well-developed. Level of Distress: NAD. Ambulation: ambulating normally. 2. Eyes- sclerae white. Conjunctivae pink. Pupils are PERRL, 3 mm bilaterally. Extraocular movements intact. 3. Ear, Nose, ThroatEars: external appearance normal-no lesions, redness, or swelling; on otoscopic exam tympanic membranes clear. Hearing is intact. Nose: appearance of nose normal with no mucous, inflammation, or lesions present. Nares patent. Septum is midline. Mouth: pink, moist mucous membranes. No missing or decayed teeth. Throat: no inflammation or lesions present. Tonsils WNL- no erythema, ulcers, masses, exudate, inflammation. 4. Cardiovascular- S1, S2. Regular rate and rhythm, no murmurs, gallops, or rubs Carotid Arteries: normal pulses bilaterally, no bruits present Pedal Pulses: 2+ bilaterally Extremities: +2 edema in RLE; no cyanosis, clubbing, less than 2 second refill 5. Respiratory- Even and unlabored. Clear to auscultation bilaterally with no wheezes, rales, or rhonchi 6. Gastrointestinal- abdomen soft and nontender to palpation, nondistended. No rigidity or guarding, no masses present, BS present in all 4 quadrants 7. Genitourinary- No bladder distention, suprapubic pain, or CVA tenderness. Prostate exam was not performed. 8. Musculoskeletal- RLE +2 pitting edema, + Homan’s sign, redness, warmth, and tenderness noted. Joint stability normal in all extremities, no tenderness to palpation in all other extremities 9. Integument/lymphaticInspection: No scaling or breaks on skin, face, neck, or arms. General palpation: no skin or subcutaneous tissue masses present, no tenderness, skin turgor normal Face: no rash, lesion, or discoloration present Lower Extremities: RLE redness and warmth; no rash, lesion, or LLE discoloration present Upper Extremities: no rash, lesion, or discoloration present 10. Neurologic- Grossly oriented x3, communication ability within normal limits, attention and concentration normal. Sensation intact to light touch, gait within normal limits 11. Psychiatric- Judgment and insight intact, rate of thoughts normal and logical. Pleasant, calm, and cooperative. Patient appears to be happy/content. 12. Hematologic/immunologic- Lymph nodes not palpable, no tenderness or masses present, no bruising DIAGNOSTIC TESTS: US DOPPLER VENOUS LOWER EXT - 09/17/14 CPT Code: 93971 Results: There is deep venous thrombosis involving the right superficial femoral popliteal and posterior tibial veins ASSESSMENT (A): Level of visit: new office outpatient visit- 99203 1. Deep Vein Thrombosis 453.40: Deep vein thrombosis, unspecified Swelling, pain, warmth, and redness of right lower extremity. Positive Homan’s sign. Doppler venous ultrasound confirmed deep venous thrombosis. 2. 311: Hypertension Currently controlled. Patient is taking altace 10 mg capsule daily 3. 530.81: Allergic rhinitis Currently controlled. Patient is taking claritin 10 mg tablet daily Differential Diagnoses: 1. Muscle strain 848.9 Swelling, pain, warmth, and redness of right lower extremity Refuting data: Doppler venous ultrasound confirmed deep venous thrombosis. 2. Cellulitis 682.6 Swelling, pain, warmth, and redness of right lower extremity Refuting data: Doppler venous ultrasound confirmed deep venous thrombosis. 3. Peripheral vascular disease 443.9 Swelling, pain, warmth, and redness of right lower extremity Refuting data: Doppler venous ultrasound confirmed deep venous thrombosis. 4. Popliteal (Baker’s) cyst Swelling, pain, warmth, and redness of right lower extremity Refuting data: Doppler venous ultrasound confirmed deep venous thrombosis. PLAN (P): 1. Patient sent to emergency department via private vehicle. Report called and given to Dr. Beasley in ED. 2. Continue taking altace 10 mg PO daily to manage HTN. Continue follow-up with primary physician every 3 to 6 months. Keep a log of daily blood pressures to take to all doctor appointments. 3. Continue taking claritin 10 mg PO daily to manage allergic rhinitis. Continue follow-up with primary physician. Medication profile: Altace - - - - Indication: Angiotensin-converting enzyme (ACE) inhibitor, used to treat hypertension, congestive heart failure (post AMI), AMI/Stroke prevention in patients age 55 years and older MOA: ACE inhibitors inhibit the actions of angiotensin converting enzyme (ACE), thereby lowering the production of angiotensin II and also decreasing the breakdown of bradykinin. The decrease in angiotensin II results in relaxation of arteriole smooth muscle leading to a decrease in total peripheral resistance, reducing blood pressure as the blood is pumped through widened vessels. Dose: HTN- 2.5 to 20mg/day PO divided q day-bid Start: 2.5mg PO daily; 1.25mg PO daily if hypovolemia or renal artery stenosis CHF, post MI- 5mg PO bid Start: 2.5mg PO bid; 1.25mg PO daily if hypovolemia or renal artery stenosis; increase dose every 3 weeks to target Cardiovascular event prevention- 10mg PO daily Start: 2.5mg PO daily x7 days, then 5mg PO daily x3 weeks, then 10mg PO daily; start 1.25mg PO daily if hypovolemia or renal artery stenosis; may divide bid if MI or HTN; for patients >55 yo with CAD, stroke, PVD, or DM history plus 1 other risk factor Brand name/generic: Altace (ramipril) Prices for 30 capsules of ramipril 10mg (generic) -Publix: $67 cash or $6.16 with coupon -Wal Mart: $9.04 with discount -Target: $35 cash or$6.16 with coupon -Walgreens: $63 cash or $12.37 with coupon Follow up: By the vascular specialist to whom the patient is referred. Consultation/referral: Patient sent to emergency department for treatment. Report called to Dr. Beasley. Patient should be referred to a specialist with expertise in vascular medicine and coagulation disorders. Patient Education: -Explain what a DVT is: a blood clot in the deep veins of the leg. The clot can clog the vessel and keep blood from getting where it needs to go. Blood backs up and causes swelling and pain. -Explain potential complications: if not treated, clot can travel to other parts of the body and clog vessels there. When a clot breaks off and moves through the bloodstream, this is called an embolism. An embolism can get stuck in the brain, lungs, heart, or other area, leading to severe damage or even death. -Emergency signs and symptoms: panting or SOB, sharp chest pain when you breathe in or strain, coughing or coughing up blood, rapid HR -Explain why he is being sent to the emergency room: You will need to be evaluated by a vascular surgeon to decide treatment options since it is a large, obstructive clot. Possible treatments include anticoagulants- heparin is usually the first drug you will receive. Coumadin is usually started as well. You will most likely take warfarin for at least 3 months. Some people must take it longer, or even for the rest of their lives, depending on their risk for another clot. You will be given a pressure stocking to wear on your leg or legs. A pressure stocking improves blood flow in your legs and reduces your risk for complications from blood clots. It is important to wear it every day. In rare cases, you may need surgery if medicines do not work. Surgery may involve: Placing a filter in the body's largest vein to prevent blood clots from traveling to the lungs or removing a large blood clot from the vein or injecting clot-busting medicines -Prevention: To prevent deep vein thrombosis: Wear the pressure stockings your doctor prescribed. Moving your legs often during long plane trips, car trips, and other situations in which you are sitting or lying down for long periods. Take blood thinning medicines your doctor prescribes. Do not smoke.