23. digestive pt
advertisement

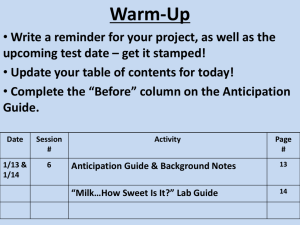
PRASETYASTUTI BIOCHEMISTRY DEPARTMENT 1) PROSES PENCERNAAN DI CAVITAS ORAL 2) 3) PROSES PENCERNAAN STOMACH PROSES PENCERNAAN DI INTESTINE Saliva Disekresi oleh glandula salivary Terdiri dari ± 99.5% air Mengandung mucin (glycoprotein) acts as lubricant for a) Mastication and b) swallowing a vehicle for the excretion of certain drugs (ethanol and morphine) ion inorganic (K,Ca, HCO3, SCN, dan Iodine, Ig (IgA) pH ± 6.8 a -amylase Saliva Menghidrolisis pati dan glikogen menjadi maltosa dan oligosakarida dengan memutus ikatan a (1->4) glycosidic In active pada pH ≤ 4 lipase Lingual Disekresi oleh glandula Ebner’s pada permukaan dorsal tongue 30% TG diet di cerna di stomach oleh lipase lambung dan lipase lingual menghasilkan asam lemak dan 1,2-diacylglycerols. Pada bayi prematur (lipase pankreas tidak disekresi dalam jumlah cukup Pada anak defisiensi lipase pankreas congenital, ½ TG dapat dicerna dan diabsorbsi. Gastric juice: sekresi gastric jernih, cairan kuning pucat 0.2-0.5% HCL pH ± 1.0 97-99% air Mucin dan garam inorganic HCL a) Mendenaturasi protein dan membunuh bacteria b) sel parietal merupakan sumber HCL c) Proses sama dengan “the chloride shift” (sel darah merah, mekanisme renal tubular sekresi H+) Mekanisme sekresi asam lambung Kadar ion H dalam sekresi sel parietal 3 juta X lebih tinggi dibanding dalam darah HC1 160 mM (ekivalen pH 0.8). Klorida disekresi melawan gradien konsentrasi dan gradien elektrik -- kemampuan sel parietal mensekresi asam tergantung pada transport aktif Pepsin Is produced in the chief cell as zymogen, pepsinogen Activated to pepsin by H+ and by pepsin itself (autocatalysis) Endopeptidase( hydrolyzes peptide bonds within the main polipeptude structur) Rennin (chimosin, Rennet) Penting dalam proses pencernaan pada bayi ( mencegah mengalirnya susu dari lambung) Tidak terdapat pada lambung orang dewasa Casein Rennin, Ca paracasein Lipase Lambung mensekresi lipase Lipase Lingual dan gastric mengawali pencernaan lipid dengan menghidrolisa TG yang mengandung asam lemak tidak jenuh rantai pendek dan rantai sedang, umumnya rantai panjang membentuk FFA dan 1,2diacylglycerols pH optimum 3.0 – 6.0 Rusak pada pH rendah Chyme (isi stomach) - duodenum Sekresi pankreas dan biliari yang alkalin menetralkan chyme yang asam sehingga pH ke arah alkalin ---- ensim pankreas dan juice intestinal aktif -- menghambat kerja pepsin Sekresi pankreas = saliva kandungan air, beberapa protein dan senyawa organik dan inorganiknya. pH sekresi pankreas ≥ 7.5 – 8.0. Disekresi sebagai zymogen Aktivasi trypsinogen oleh enterokinase (enteropeptidase) di sekresi oleh mukosa intestinal . Menghidrolisis ikatan peptida lisin dalam zimogen, melepas polipeptida kecil --- tripsin aktif sekali trypsin terbentuk , mengkatifkan trypsinogen ---- > trypsin kimotripsinogen -- kimotrypsin proelastase -- elastase dan procarboxypeptidase, --- carboxypeptidase karboksipeptidase exopeptidase Menghidrolisis ikatan peptida terminal karboksil , membebaskan asam amino Amylase Menghidrolisis amilum dan glikogen menjadi maltosa, maltotriosa (3 residu α-glucosa diikat dengan ikatan α 1-4) dan a mixture of branched (1---6) oligosaccharides (α- limit dextrins), non branched oligosaccharides, and some glucose Lipase Menghidrolisis ikatan ester primer TG Bekerja pada antar muka minyak dan air yang mengemulsikan tetes lemak yang terbentuk melalui agitasi mekanik dalam usus dengan adanya produk aktivitas lipase gastrik dan lipase lingual, garam empedu, kolipase, fosfolipid dan phospholipase A2. Kimotripsin spesifik untuk ikatan peptida yang mengandung residu asam amino yang tidak bermuatan Elastase Menghidrolisis ikatan yang berdekatan dengan residu asam amino kecil (glisin, alanin dan serin) Cholesteryl ester hydrolase Mengkatalisis hydrolysis cholesteryl esters - diabsorbsi dari intestine dalam bentuk bebas tidak teresterifikasi Ribonuclease (Rnase) and deoxyribonuclease (Dnase) Phospholipase A2 Menghidrolisis ikatan ester pada posisi 2 glycerophospholipids yang berasal dari biliary dan diet dietary origins to formembentuk lysophospholipid Bile Diproduksi oleh liver diantara waktu makan Berperan penting dalam pencernaan gallbladder menyimpan bile Sifat-sifat bile 1. emulsification -- menurunkan tegangan permukaan 2. Neutralization menetralkan kimus yang asam yang berasal dari lambung 3. excretion -- wahana asam empedu dan ekskresi cholesterol, obat2, toksin, pigmen empedu, macam2 substansi inorganik ( Cu, Zn, Hg) Juice intestinal di sekresi oleh glandula Brunner dan Lieberkuhn - Aminopeptidase : exopeptidase menghidrolisis ikatan peptida didekat amino terminal asam amino dari polypeptide dan oligopeptida dan dipeptidase - disaccharidases and oligosaccharidases - Maltase ( maltose -- 2 mol glucose) - Sucrase [ sukrosa --glukosa + fruktosa] - Lactase ( lactose - galactose + glucose - Trehalase : hydrolysing trehalosa - Phosphatase: menghilangkan phosphate dari fosfat organik Polynucleotidases Mengubah asam nukleat -- nucleotida Nucleosidases Mengkatalisis fosforilasi nukleosida - basa nitrogen + pentose phosphate Phospholipase Phospholipids - glycerol, fatty acids, phosphoric acid, bases ( choline) Secretion Enzyme Substrate Action Saliva Ptyalin Starch Hydrolysis to form dextrins Gastric juice Pepsin Protein Gastric lipase Fats Hydrolysis of peptide bonds Hydrolysis into free fatty acids Final Product Secretion Enzyme Substrate Action Pancreatic exocrine secretion Lipase Fat Final Product Hydrolysis to Fatty monoacids glycerides Cholesterol Cholesterol esterase Hydrolysis to Cholesesters of terol cholesterol and fatty acids alphaAmylase Hydrolysis Starch, dextrins Dextrin, maltose Secretion Enzyme Substrate Action Pancreatic exocrine secretion Protein Hydrolysis Polypeptides Chymotrypsin Protein Hydrolysis Polypeptides Carboxypeptidase Hydrolysis Amino acids Trypsin Polypeptides Final Product Ribonuclease Ribonu-cleic Hydrolysis Monoacids nucleotides Elastase Fibrous protein Hydrolysis Amino acids Secretion Enzyme Substrate Action Brush border CarboxyPolypepenzymes peptidase; tides aminopeptidase; dipeptidase Hydrolysis Final Product Amino acids Enterokinase Trypsino-gen Activates to trypsin Polypeptidases and peptides Sucrase Sucrose Glucose, fructose Hydrolysis Secretion Enzyme Substrate Action Brush border enzymes Isomaltase Dextrin Final Product Hydrolysis Glucose Maltase Maltose Hydrolysis Glucose Lactase Lactose Hydrolysis Glucose, galactose Nucleotidases Nucleic acid Hydrolysis Nucleotides Nucleosidases Nucleosidases Hydrolysis Purine and and pyrimidine phosphorylase bases A Lactose intolerance Lactase activity is rate-limiting for lactose absorption The syndrome should not be confused with intolerance to milk Sign and symptoms Cramps, diarrhea, flatulence (accumulation of undigested lactose, osmotically active hold water- fermentative action on the sugar of the intestinal bacteria - produce gases ) Lactase deficiency: the small intestine produces low levels of lactase and cannot digest much lactose. Lactose malabsorption. Lactase deficiency may cause lactose malabsorption. In lactose malabsorption, undigested lactose passes to the colon. The colon, part of the large intestine, absorbs water from stool and changes it from a liquid to a solid form. In the colon, bacteria break down undigested lactose and create fluid and gas. Not all people with lactase deficiency and lactose malabsorption have digestive symptoms. Lactase deficiency and lactose malabsorption may lead to lactose intolerance 1. Inherited lactase deficiency Relatively rare Symptoms develop very soon after birth - The feeding of lactose-free diet –> disappearance of the symptoms - consumtion of live culture yogurt ( provides active β–galactosidase , Ca and energy to replase milk 2. Secondary low-lactase activity Digestion of lactose is limited even in normal humans, intolerance to milk is not uncommon as a consequence of intestinal diseases. Tropical and non tropical sprue Kwashiorkor Colitis Gastroenteritis After surgery for peptic ulcer 3. primary low-lactase activity Gradual decline in activity of lactase Not due to lack of lactase mRNA B. Sucrase Deficiency An inherited deficiency sucrase and isomaltase ( sucrase and isomaltase occur together as a complex enzyme) C. Disacchariduria An increase excretion of disaccharides ≥ 300 mg disaccharide excreted in the urine D. Monosaccharide Malabsorption Congenital condition due to a single mutation in which glucose and galactose are absorbed only slowly defect in the Na glucose cotransporter carrier mechanism (SGLT1) Fructose is not absorbed via this transporter - absorbtion of fructose is normal CHYLURIA : chylomicrons are present in urine The presence of an abnormal connection between the urinary tract and the lymphatic drainage system of the intestine Feeding TG in place of dietary fat --- disappearance of chyluria. Colipase deficiency : defect pancreatic lipase activity Lactase deficiency: the small intestine produces low levels of lactase and cannot digest much lactose. Lactose malabsorption. Lactase deficiency may cause lactose malabsorption. In lactose malabsorption, undigested lactose passes to the colon. The colon, part of the large intestine, absorbs water from stool and changes it from a liquid to a solid form. In the colon, bacteria break down undigested lactose and create fluid and gas. Not all people with lactase deficiency and lactose malabsorption have digestive symptoms. Lactase deficiency and lactose malabsorption may lead to lactose intolerance Primary lactase deficiency, (lactase non persistence) is the most common type of lactase deficiency. In people with this condition, lactase production declines over time. This decline often begins at about age 2; however, the decline may begin later. Children who have lactase deficiency may not experience symptoms of lactose intolerance until late adolescence or adulthood. Researchers have discovered that some people inherit genes from their parents that may cause a primary lactase deficiency. Secondary lactase deficiency results from injury to the small intestine. Infection, diseases, or other problems may injure the small intestine. Treating the underlying cause usually improves the lactose tolerance Developmental lactase deficiency may occur in infants born prematurely. This condition usually lasts for only a short time after they are born. Congenital lactase deficiency is an extremely rare disorder in which the small intestine produces little or no lactase enzyme from birth. Genes inherited from parents cause this disorder. JA, Assa’ad A, Burks AW, et al. Guidelines for the diagnosis and management of food allergy in the United States: report of the NIAID-sponsored expert panel. Journal of Allergy and Clinical Immunology. 2010;126(6 suppl.):S1–S58. 2Suchy FJ, Brannon PM, Carpenter TO, et al. National Institutes of Health Consensus Development Conference: lactose intolerance and health. Annals of Internal Medicine. 2010;152(12):792–796. 1Boyce 1. Stomach and Intestine Peptic ulcers Peptic ulcer is a general term that refers to ulcers occurring in the lower esophagus, the stomach, or the duodenum (upper part of the small intestine). What is the difference between a duodenal ulcer and a gastric ulcer? A duodenal ulcer is a break in the lining of the upper part of the small intestine (the duodenum); a gastric ulcer is a break in the lining of the stomach. 2. Bile and the Biliary System a. Gallstones (Cholelithiasis) There are two major types of gallstones, which form due to distinctly different pathogenetic mechanisms 1. Cholesterol Stones About 90% of gallstones are of this type. These stones can be almost pure cholesterol or mixtures of cholesterol and substances such as mucin. The key event leading to formation and progression of cholesterol stones is precipitation of cholesterol in bile. There are clearly important genetic determinants for cholesterol stone formation. There is also an important gender bias in development of stones - the prevalence in adult females is two to three times that seen in males and use of contraceptive steroids is a risk factor for development of gallstones. 2. Pigment Stones Roughly 10% of human gallstones are pigment stones composed of large quantities of bile pigments, along with lesser amounts of cholesterol and calcium salts. The most important risk factor for development of these stones is chronic hemolysis from almost any cause - bilirubin is a major constituent of these stones. Additionally, some forms of pigment stones are associated with bacterial infections. Apparently, some bacteria release deconjugate bilirubin, leading to precipitation as calcium salts b. Jaundice Jaundice, is yellowing of the skin, sclera (the white of the eyes) and mucous membranes caused by increased levels of bilirubin in the human body. Usually the concentration of bilirubin in the blood must exceed 2-3mg/dL for the coloration to be easily visible. Jaundice comes from the French word jaune, meaning yellow