Yen - WordPress.com
advertisement

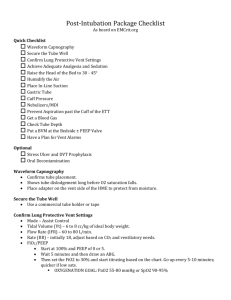
Roles INTUBATION CHECKLIST Adapted from Greater Sydney Area-HEMS checklist v2016-01-30 Monitor Lifeguard or Assistant reads Intubator checks and responds Situation briefed Resuscitation maximized Roles assigned Check Check Check P.P.E. Position optimized Oxygen sufficient, maximized and preoxygenated Mask O2 at 15 liters, Nasal O2 at 15 liters Suction tested Two I.V.’s working Monitors visible: Sat Cardiac BP B.P. cuff cycling, opposite arm Drugs ready: Induction + Paralytic? Fluids + or - Pressors? Post analgesia / sedation? Monitor lifeguard Drug pusher Documenter Airway assistant C-spine stabilizer Intubator SET-UP Check Check Check Check Check IV/MONITORS/DRUGS Check Check Check Check Check Check B.V.M., PEEP, End-tidal CO2 O.P.A., N.P.A. Laryngoscope tested Endotracheal tube and Syringe Cuff tested and lubed Extra tube, Tube tie Stylet and Bougie Supraglottic airway and Cric kit EQUIPMENT Check Check Check Check Check Check Check Check C-spine assistant briefed Risks discussed Fail plan briefed E.L.M. & bougie plan briefed Desat trigger and plan briefed TEAM BRIEF Check Check Check Check Check Any other questions and concerns? CHECKS COMPLETE – ANESTHETIZING AT _ _ : _ _ Yen Chow @TBayEDguy 2016-02-07 Succinylcholine contraindications Malignant Organophosphates NEVERhyperthermia USE (K+ release+++) PROLONGED DURATION Hyperkalemia (known or concern), Crush injury Pseudocholinesterase def Malignant hyperthermia Organophosphate tox Myopathies/Muscular dystrophies Myasthenia gravis(?) Hyperkalemia, Crush injury Eaton-Lambert Syndrome* Amyotrophic Lateral Sclerosis, Myopathy, Muscular dystrophyMultiple Sclerosis Pseudocholinesterase def, Guillain-Barre, Botulism, Tetanus Amyotrophic Lateral Sclerosis, Multiple Sclerosis Hypothyroidism Burns ≥ 2nd degree over 10% BSA >5 days until healed Guillain-Barre, Botulism, Tetanus Stroke Spinal 6 months GIVE MOREpost injury Burnswith ≥ 2ndhemiparesis, º >10% BSA >5 dayscord untilinjury healed>5 days until Severe intra-abdominal sepsis >5 days until resolution Myasthenia Gravis** (lasts long tho) Stroke + hemiparesis, Spinal cord injury >5 days until 6 months post injury NO PROBLEM Severe intra-abdominal sepsis >5 days until Parkinson’s Disease resolution Epilepsy Acute CVA or spinal cord injury *Sensitive to BOTH depolarizing and non-depolarizing neuromuscular blockers **Resistant to succinylcholine; BUT avoid non-depolarizing, response unpredictable, use ½ dose BRIEFING Situation What’s going on Task What we need to do Intent The reason is Concerns Watch out for Calibrate Other thoughts/ideas? Intubation drugs kg lbs 40 88 50 110 60 132 70 154 80 176 90 198 100 220 110 242 120 264 130 286 140 308 150 kg 330 lbs 80 160 20 20 40 100 200 25 25 50 120 240 30 30 60 140 280 35 35 70 160 320 40 40 80 180 360 45 45 90 200 400 50 50 100 220 440 55 55 110 240 480 60 60 120 260 520 65 65 130 280 560 70 70 140 300 600 75 75 150 12 6 15 7.5 18 9 21 10.5 24 12 27 13.5 30 15 33 16.5 36 18 39 19.5 42 21 60 6 24 240 75 7.5 30 300 90 9 36 360 105 10.5 42 420 120 12 48 480 135 13.5 54 540 150 15 60 600 165 16.5 66 660 180 18 72 720 195 19.5 78 780 210 21 84 840 225 22.5 90 900 60 160 80 75 200 100 90 240 120 105 280 140 120 320 160 135 360 180 150 400 200 165 440 220 180 480 240 195 520 260 210 560 280 225 mg 600 mg 300 mg 48 64 40 80 40 2 8 1 8 60 80 50 100 50 2.5 10 1.25 10 72 96 60 120 60 3 12 1.5 12 84 112 70 140 70 3.5 14 1.75 14 96 128 80 160 80 4 16 2 16 108 144 90 180 90 4.5 18 2.25 18 120 160 100 200 100 5 20 2.5 20 132 176 110 220 110 5.5 22 2.75 22 144 192 120 240 120 6 24 3 24 156 208 130 260 130 6.5 26 3.25 26 168 224 140 280 140 7 28 3.5 28 180 240 150 300 150 7.5 30 3.75 30 Ketamine (IBW) IV 2 mg/kg IM 4 mg/kg shocky 0.5 mg/kg IV gtts 0.5 mg/kg/h to 1.0 mg/kg/h mg mg mg mg/h mg/h Etomidate (TBW) IV 0.3 mg/kg shocky 0.15 mg/kg IV 45 mg 22.5 mg Propofol (LBW vs TBW) LBW IV 1.5 mg/kg shocky 0.15 mg/kg IV TBW gtts 0.6 mg/kg/h to 6 mg/kg/h mg mg mg/h mg/h Succinylcholine (TBW) IV 1.5 mg/kg IM 4 mg/kg shocky 2 mg/kg IV Rocuronium (IBW) IV 1.2 mg/kg shocky 1.6 mg/kg IV Fentanyl IV 1 mcg/kg 2 mcg/kg gtts 1 mcg/kg/h Midazolam 0 .05 mg/kg IV/IM 0.2 mg/kg gtts 0.025 mg/kg/h to 0.2 mg/kg/h Yen Chow @TBayEDguy 2016-02-07 mg mg mcg mcg mcg/h mg mg mg/h mg/h POST-INTUBATION Reassess ABCD vitals ETT secured Tube depth, ETCO2 waveform, Cuff pressure In-line suction ready Analgesia/Sedation Supplies (oxygen, drugs, power) Ventilator settings Head of Bed raised 30 degrees Gastric tube & Foley prn Secure all lines and tubes Rescue airway equipment nearby Post debriefing What was planned? List objectives and expected actions What actually happened? Review any actions not standard operating procedure Review any safety concerns Why did it happen? Reasons for ineffective or unsafe performance What can we do next time? Identify effective and ineffecrive performance Determine how to apply the lessons leared to the next time Yen Chow @TBayEDguy 2016-02-07 Check Check Check Check Check Check Check Check Check Check Check 12 (3x4) Step Response to desaturation BVM PEEP 15 Mask 15 LPM Nasal 15 LPM Upright lungs, Clear FB OAW Jaw thrust position head fluids and neck Coordinated slow small Pulse ox lag? Two person Mask seal squeeze Shock? underhand Sex (6) Steps to BVM (adapted from Jason N. Cook @cptjcook “#SexyBagging”) 2 thumbs 2 person ventilate carefully OPA/NPA down jaw position BVM with coordination thrust Airways (OPA NPA) BVM and PEEP CO2 end-tidal and confirm (stethoscope) Suction(s) Laryngoscope and alternates Oxygen (pre re and apOx) Positioned Endotracheal tube cuff lubed tested syringed Stylet Bougie SGA Surgical airway Monitors, Meds, IV, BP cuff cycling opp arm Assistants and roles assigned, tasks briefed ELM Bougie Plan, approach, fails, risks Assistants help add or maintain • • • • • • • • Collar opening, in line stabilization Cricoid pressure External Laryngeal Manipulation Bougie prepass Head elevation Extra laryngoscope lift Jaw thrust Mouth opening Yen Chow @TBayEDguy 2016-02-07 Jaw thrust Airways (oral / nasal) Work together Slow small squeeze from Rich Levitan @airwaycam PEEP Optimize each airway attempt by Manipulations (head neck larynx device) Adjuncts Suction Change size/type Oxygenation, O2 flow, PEEP address Tone adapted from #Vortex @VortexApproach Nicholas Chrimes @nicholaschrimes and Peter Fritz @pzfritz 30 second drilled responses to encountered or anticipated difficulty 1) Release/relax cricoid 2) ELM bimanual laryngoscopy 3) Extra head elevation 4) Extra laryngoscope lift 5) Use Mac as Miller 6) Bougie Consider 1) More jaw thrust/mouth opening 2) Check position patient/intubator 3) More/better suction 4) Change blade/device size/type Technique (e.g. right paraglossal straight blade) 5) Change intubator (best experienced) 6) Address patient tone, cooperation, muscle relaxation 7) Use right corner of mouth/right cheek pull 8) Straight to cuff styletting 9) Left turn at Laryngeal inLet on railroading ETT over bougie 10) Right turn tube tip hitting tracheal Rings Each next attempt MUST Address difficulty encountered and Change something