Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
Chapter 28 – Intraepithelial Neoplasia of the Lower Genital Tract (Cervix, Vulva) :
Etiology, Screening, Diagnostic Techniques, Management
Kenneth L. Noller
KEY TERMS AND DEFINITIONS
Atypical Squamous
Cells (ASC)
Bethesda System term used to indicate that abnormal squamous cells
are present that do not fulfill all the criteria for a diagnosis of a
squamous intraepithelial lesion. It is commonly abbreviated as ASC.
Two subtypes are recognized: ASC of undetermined significance (ASCUS) and ASC, cannot exclude a higher grade lesion (ACS-H).
Atypical Glandular
Cells (AGC)
A Bethesda System term used to indicate that there are abnormal
glandular cells present that do not fulfill all the criteria for a diagnosis
of an adenocarcinoma in situ or adenocarcinoma. The term can often
be further qualified if the cells of origin can be identified.
The Bethesda System
(TBS)
A system of terminology for the reporting of cervical cytology test
results that is used by virtually all cytology laboratories in the United
States as well as in many other countries. It was last revised in 2002.
Carcinoma In Situ
An older term, now mostly abandoned, to represent full epithelial
thickness neoplastic changes. It has been replaced by the term cervical
intraepithelial neoplasia 3.
Cervical
Intraepithelial
Neoplasia (CIN)
A premalignant change in the cervical epithelium. The cells have
altered nuclei that have at least some features of a neoplastic process.
CIN is graded in three steps. CIN 1 is of little or no clinical
consequence as it is usually a result of a transient human
papillomavirus infection only. In the past, CIN 1 was referred to as
mild dysplasia. If the cellular changes are more extensive and include
one half to two thirds of the thickness of the epithelium, it is referred to
as CIN 2. Full-thickness cellular changes are referred to as CIN 3. CIN
3 includes those changes previously referred to as severe dysplasia and
carcinoma in situ.
Colposcope
(Colposcopy)
A low-power, binocular microscope that is mounted on a stand. It is
focused approximately 30 cm from the objective lens. It is used to view
the uterine cervix after a speculum has been introduced into the vagina.
It is the diagnostic method of choice for the evaluation of most Pap test
abnormalities.
Conization
Removal of the central cervix for the purpose of diagnosis or treatment
of cervical neoplasia. It may be performed either with a scalpel (cold
knife cone) or by a loop electroexcision procedure.
Cryocautery
An office method for the destruction of areas of CIN. Although its
success rate is similar to that of a loop electroexcision procedure, it is
used less frequently than in the past. One limitation is that no tissue
sample is obtained.
Dysplasia
An outdated term for the changes now called CIN.
Endocervical
Sampling
This refers to obtaining a sample from the endocervix to determine
whether CIN is present. The sample can be collected with an
endocervical brush (cytology) or an endocervical curette (histology).
High-Grade
This is a term used in TBS to report cellular changes that are consistent
Squamous
with a histologic report of CIN 2 or CIN 3. It is slowly replacing the
Intraepithelial Lesion
CIN terminology for histology specimens.
(HSIL)
This is a group of more than 100 types of DNA-containing viruses
known to infect humans. More than 15 types may be found in the
genital area. Cervical cancer virtually always contains HPV DNA. The
Human
vast majority of all sexually active individuals are infected with the
Papillomavirus (HPV)
virus at some time. In most cases, the infection is self-limited. Recently,
vaccines have been developed that prevent HPV infection with the more
common HPV types.
Loop Electroexcision
Procedure (LEEP)
This is the most commonly used procedure for the removal of areas of
CIN. It is an office procedure in which a thin electric wire loop is used
to excise squamous intraepithelial lesions.
Low-Grade
This is a term used in TBS to report cellular changes that are consistent
Squamous
with a histologic report of CIN 1. In most cases, it indicates that an
Intraepithelial Lesion
active HPV infection is present.
(LSIL)
Metaplasia
The process by which an area of glandular epithelium is replaced by
squamous epithelium. It is a normal process and its presence on a
biopsy specimen is considered normal.
Mosaic
A colposcopic term used to describe a tissue pattern that is often
associated with neoplasia.
The concept that cancer could be diagnosed by the examination of cells
was conceived by Dr. Papanicolaou, and the test retains his name.
Originally, a sample of cells was scraped from the uterine cervix,
spread on a glass slide, and fixed in alcohol. Samples are now most
Pap Test (Pap Smear) often placed in a vial of transport medium, and the actual slide is
prepared in the laboratory. The Pap test is the most effective cancer
screening procedure ever developed. In countries where most adult
women are screened regularly, the incidence of invasive cervical
cancer is reduced by approximately 70%.
Punctation
A colposcopic term used to describe a tissue pattern that is often
associated with neoplasia.
Satisfactory
Colposcopy
A colposcopic examination in which the entire transformation zone can
be seen. All other examinations are termed unsatisfactory.
This is the area between the border of squamous epithelium and
Transformation Zone glandular epithelium in the central cervix. Almost all significant
squamous neoplasia originates in this area.
Carcinoma of the cervix is one of the most common malignancies in women. According to a
2002 ACOG Practice Bulletin, it is estimated to be the second or third most common cause of
cancer death in women worldwide, despite the fact that a screening test, the Pap smear, is
available that has been demonstrated to reduce the incidence of the disease by at least 70%.
Unfortunately, many developing countries lack the ability to carry out widespread Pap screening.
The epidemiology of cervical cancer has been studied for more than a century. This work paved
the way for the discovery that an infection with the HPV is a necessary, but insufficient cause of
the disease (Bosch and coworkers). The recent introduction of a vaccine that protects against the
most prevalent cancer-associated types of HPV infection has the potential to reduce the
occurrence of this cancer dramatically (Mao and associates).
Cervical neoplasia is also increased in women who are immunosuppressed whether through
infection (e.g., HIV), medications (e.g., chemotherapy), or genetics, according to a 2003 study by
Schuman and coworkers. Smoking also increases a woman's risk of developing significant CIN,
probably by altering the local immune response of the cervix.
KEY POINTS
•
The Pap test is the most effective cancer screening procedure ever developed.
•
When it is used widely, it decreases the incidence of cervical cancer by approximately
70%.
•
TBS terminology is used for the reporting of cervical cytology specimens.
•
Cervical cancer is caused by HPV.
•
Virtually all HPV infections regress spontaneously.
•
Smoking increases the likelihood that an HPV infection will persist or progress.
•
A vaccine is available that prevents HPV infection if given before exposure to the
HPV types in the vaccine.
•
In some cases, an HPV infection can lead to a precancer of the cervix called CIN. CIN
is graded as 1, 2, or 3 depending on the percentage of the epithelial thickness that is
involved in the process.
•
CIN 1 should be observed rather than treated as it usually regresses spontaneously.
•
Treatment of CIN 2 and 3 can be performed in the office with any one of several
techniques.
•
CIN 2 and 3 occur more commonly in women who are immunocompromised.
•
An HPV DNA test can be used to triage women with ASC-US cytology reports. It can
also be combined with cervical cytology for screening for CIN in women older than
age 30.
•
The colposcope is used to evaluate women with abnormal Pat tests.
•
The LEEP procedure is the most common method used to treat CIN 2 and 3.
•
Cervical stenosis, infertility, and premature birth are increased slightly in women who
have been treated for CIN, regardless of the treatment method used.
HISTORY, EPIDEMIOLOGY, AND INFECTION
It is likely that carcinoma of the cervix has been a major cause of cancer death for centuries,
although histologic confirmation has only been available more recently. In Paris in the 19th
century, cervical cancer was reported to be the most common malignancy in women.
In the early part of the 20th century, epidemiologic studies demonstrated that the cancer was
closely linked to sexual activity. Early age at first intercourse and multiple sexual partners were
the most consistent risk factors. This suggested that there might be an infectious agent passed
through sexual activity that is the “cause” of cervical carcinoma. Although some studies found
associations with herpes simplex virus infections, Chlamydia infections, and gonorrhea, all these
were ultimately discarded. It was only when it became possible to identify HPV infection that the
true “cause” of cervical cancer was discovered.
The papillomaviruses are found in virtually all mammalian species and are generally speciesspecific. They are double-stranded DNA viruses that replicate within epithelial cells, as
described in a 2005 ACOG Practice Bulletin. The group that infects humans (HPV) includes
more than 100 types. Within these types there is further grouping such that the types that
commonly are found on one anatomic part of the body are not the same as found on other parts.
For example, plantar warts on the feet are not caused by the same HPV types as warts on the
hands. In several locations, infection with HPV is associated with a clinically evident lesion, the
wart. Unfortunately, this has led to HPV being labeled as the “wart virus” despite the fact that
many infections, indeed most in the genital tract, do not form warts.
Approximately 40 types of HPV are known to infect the genital tract of both men and women. Of
these, at least 12 are associated with cancer. The other types are either associated with genital
warts or unimportant infections with no clinical symptoms. Because it is not possible to grow the
virus in the laboratory, it has taken many years and much indirect evidence to determine that an
infection with one of the cancer-associated types is a necessary precursor to squamous cell
carcinoma and most of the cases of adenocarcinoma of the uterine cervix. However, the virus is
an “incomplete” cause as the vast majority of genital HPV infections do not result in cancer.
Epidemiologic evidence is conclusive that the virus can be passed from one individual to another
through sexual activity. However, HPV DNA can be found on clothing and other surfaces and
thus fomite transmission might be possible, although, according to Winer and colleagues, it is
unlikely. It will not be possible to determine whether such material is infective until a method of
culturing HPV is developed.
Studies of college students and other groups performed by Wheeler and colleagues in 1996 and
Moscicki and associates in 1998 have confirmed that most men and women acquire a genital
HPV infection within a few years of the onset of sexual activity. The most common type
identified in the general U.S. population is type 16, which is also the type most highly associated
with cancer. Studies by Ho and associates in 1995 and 1998 [16] [15] tested participants for
evidence of the virus at regular intervals several months apart, and most of the detected
infections cleared within a few months, although some persisted for as long as 36 months.
Recently, it has been found that many infections last only a few weeks, suggesting that the
previous studies underestimated the cumulative incidence of the disease. Many investigators now
believe that in sexually active individuals, infection with HPV at some time is almost universal.
Despite nearly uniform infection with HPV, the vast majority of women do not develop cervical
cancer (Koutsky and colleagues). That is, of the millions and millions of women who are
infected with HPV, only a few will ever develop cervical cancer, even if they are never screened
and/or treated for preinvasive lesions. Longitudinal studies have now confirmed this fact ( Fig.
28-1 ). The search for a predictive measure that will distinguish between those women who are
infected and will clear the disease and those in whom the infection will persist and lead
eventually to carcinoma has been frustrating. Although it is clear that those women who have a
compromised immune system from any cause (genetic, iatrogenic, or infectious) have a greater
risk of developing a persistent HPV infection, there is as yet no way to predict which healthy
women will be unable to clear the disease spontaneously (Aldieh and associates). The only other
independent risk factor that has been identified is smoking.
Figure 28-1 Colpophotograph of a cervix with an active human papillomavirus infection. The patient had a cytology sample
reported as low-grade squamous intraepithelial lesion. She was followed without treatment, and the lesions regressed over the next
year.
A cancer-associated HPV type causes neoplastic cellular changes when its DNA becomes
integrated into the host cell genome. When this happens, certain repressor areas of the viral
genome are lost. Consistently, the loss of these control mechanisms allows for the expression of
the viral E6 and E7 genes. As described by Munger and colleagues, the production of
oncoproteins results in the inactivation of the p53 and retinblastoma tumor repressors). These
changes theoretically lead to cell immortalization and rapid cell proliferation. However, in most
cases, the transformed cells are managed by the individual's immune system, and the
infection/intraepithelial neoplasia is defeated. In some women, for reasons that are still not clear,
the transformed cells begin to replicate, and if the lesion is not treated, after a period of several
years, a cancer can develop.
Testing for the presence of HPV DNA is useful in a few specific clinical settings, and these are
described in the sections on cytology screening and management of abnormal cytology reports.
Recently, vaccines that protect against the acquisition of HPV types 16 and 18, the two most
common cancer-associated HPV types, have become available commercially. Studies, in
particular one by Mao and colleagues, have confirmed that they protect against the development
of significant preinvasive neoplasia and that the protection remains effective for at least 3.5
years. These vaccines have the potential to prevent approximately 70% of all cases of squamous
cancer of the cervix. However, to be most effective, they must be given before exposure, that is,
at the onset of sexual activity ( Noller and associates, 1987 ). Ideally, all girls (and boys,
although the studies showing efficacy in males have not yet been completed) would receive the
series of three injections around age 11 and 12. It is not yet known whether vaccination
protection is lifelong or whether a booster dose will be needed later. The vaccine is derived from
“virus-like particles” that do not contain any of the viral DNA.
Because the vaccines currently available do not provide protection against all cancer-associated
HPV types, screening with the Pap test will need to be continued indefinitely. Indeed, it is
possible that suppression of types 16 and 18 will provide an opportunity for other carcinogenic
types to become more prevalent. Newer vaccines that have the potential to protect against a
greater number of the common cancer-associated types are in development.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com
Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
CERVICAL CYTOLOGY TESTING (THE PAP TEST)
Cervical cytology testing became available in many developed countries in the 1950s after the
studies of Dr. Papanicolaou had shown that by examining a cellular sample scraped from the
uterine cervix and properly prepared and stained, the presence of cancer and its precursors could
be identified. The 1941 monograph by Drs. Papanicolaou and Traut remains one of the sentinel
breakthroughs in the history of preventive medicine. Their work led to the demonstration that
when cancer precursors were identified, local therapy prevented the development of cancer.
Despite the fact that Pap testing has a low sensitivity (many false-negatives), in virtually all
countries that use it, the incidence of cervical cancer has been reduced by approximately 70%,
according to Fahey and Nanda and their coworkers. The success of the technique relies on the
facts that it takes many years for invasive cancer to develop following an HPV infection and that
most women are tested repeatedly. Indeed, most women who develop invasive cervical cancer in
the United States have either never been tested or have not been tested for many years.
The technique requires that the cervix be visualized after placement of a speculum into the
vagina. The portio of the cervix is then scraped using either a “broom” or the combination of a
plastic spatula and an endocervical brush (Figs. 28-2 and 28-3 [2] [3]) ( Martin-Hirsch and
coworkers, Lancet, 1999 ). Noller and colleagues' 2003 survey of the Fellows of the American
College of Obstetricians and Gynecologists showed great uniformity the use of Pap testing. This
survey was conducted before the new cytology guidelines, discussed later, had become widely
accepted.
Figure 28-2 A plastic spatula is often used to obtain a specimen from the exocervix. It must be used with an instrument that samples
the endocervix. A, Cervix as seen through a speculum, with the spatula being used to obtain a cell sample. B, Longitudinal view at
the same point in the procedure.
Figure 28-3 Both of these instruments can be used to obtain a cytologic sample from the endocervix. Cervical broom (Unimar)
(top). Cytobrush (Medscand) (bottom).
Originally, the clinician would place the collected sample on a glass slide and fix it with alcohol.
In recent years, that method has been replaced almost entirely by a “liquid-based” approach. The
sample is now placed in a liquid medium for transport to the laboratory where the slide is
prepared. This technique is slightly more sensitive for the detection of CIN, but its greatest value
is that the medium can be used for HPV DNA testing and for the detection of some sexually
transmitted diseases (Hutchinson and colleagues).
ACOG has recommended Pap testing for all women within 3 years of the onset of sexual activity
or at age 21 (ACOG Practice Bulletin Number 45, 2003; ACOG Committee Opinion Number
330, 2006). Invasive cervical cancer is virtually never found in women younger than the age of
21 as the disease takes many years to develop after an initial HPV infection. Nonsexually active
women should be tested at age 21 as there is some evidence that HPV infections might occur
from fomite transmission. In addition, childhood sexual abuse might also transmit HPV.
The frequency of Pap testing has always been controversial. Although annual testing was the
norm for many years, there has never been a study conducted to determine the optimum
frequency. Currently, most organizations that make recommendations suggest annual testing
until age 30. After age 30, if there has been no evidence of HSIL and the most recent previous
tests have been negative, the interval can be extended to every 2 or 3 years. Perhaps the most
effective testing after age 30 is the use of the combination of the Pap test and HPV DNA, per
studies by Bellinson and Schiffman and their associates. If both of these tests are negative, the
risk of HSIL during the next 3 years is extremely small. (This is the only U.S. Food and Drug
Administration–sanctioned use of HPV DNA testing as a screening procedure.) Annual testing
with cytology alone is acceptable, although not necessary for most women.
Of course, the combination of two tests for screening will occasionally result in disparate results,
i.e., when one test is positive and the other is negative. A group of experts in this area met under
the leadership of the National Cancer Institute to develop interim guidelines for patient
management in these situations. Results were published by Wright and colleagues in 2004 . In
general, if one test is positive and one negative, the clinician can either perform colposcopy or
repeat both tests in 6 to 12 months. Eventually, data will emerge to support or modify these
opinions.
In the past, according to the ACOG Practice Bulletin 45, most women were advised to continue
to have Pap testing after hysterectomy, despite the fact that vaginal carcinoma is exceedingly
rare. Indeed, Pearce and colleagues showed that most abnormal Pap tests after hysterectomy
result in false-positives. Therefore, the current recommendation is that women cease to have Pap
testing after a total hysterectomy, i.e., the cervix has been removed completely. The only
exceptions are women who have a history of an HSIL, are immunocompromised, or were
exposed in utero to diethylstilbestrol.
Testing may also be discontinued in women who have no history of HSIL, have no new sexual
partner, and have reached an advanced age, according to a study by Sawaya and associates.
Unfortunately, the various organizations do not agree on the age at which testing can be stopped,
but the age range of 65 to 70 is most commonly cited.
Several investigators have examined the cost benefit of various cytology methods, intervals, and
techniques. In most cases, according to studies by Brown and Garber and Kim and coworkers,
following the current guidelines is the most efficient method both to care for a patient and to
maximize the expense of screening.
Cervical Cytology Reporting:The Bethesda System
In 1988, the National Cancer Institute convened a conference to develop a uniform terminology
for the reporting of Pap test reports. It has been modified twice, the most recent modification
occurring in 2001 (Broder). The box shows the currently used classification. Virtually all
laboratories in the United States (and many countries throughout the world) use this terminology.
The management of patients with various abnormal reports is outlined here. ACOG Practice
Bulletin Number 66 and a summary article by Noller in 2005 are sources for more information
on this topic. Unfortunately, this cytology nomenclature is often confused with the terms used to
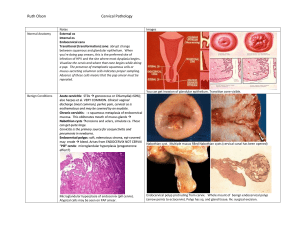
describe histologic diagnoses. Figure 28-4 shows how TBS, CIN, and dysplasia categories
correspond to tissue changes.
Figure 28-4 Diagram of cervical epithelium showing various terminologies used to characterize progressive degrees of cervical
neoplasia. CIN, cervical intraepithelial neoplasia; HSIL, high-grade squamous intraepithelial lesion; HPV, human papillomavirus;
LSIL, low-grade squamous intraepithelial lesion.
The first part of any TBS report states whether the sample was satisfactory or unsatisfactory.
Reasons for an unsatisfactory report include such things as lack of a label, loss of transport
medium, scant cellularity, and contamination by foreign material. Few samples are reported as
unsatisfactory if a liquid-based technique is used.
The report next indicates whether the cellular material was normal. If other than normal, the
abnormalities are further divided into squamous and glandular. The cytologist may also comment
on the presence of evidence of infections such as yeast and changes consistent with a diagnosis
of bacterial vaginosis.
Squamous abnormalities are found in approximately 5% to 6% of all cytology samples. The most
common is ASC-US. This indicates that there are cells on the slide that show some of the
features associated with squamous lesions, but either there are very few of these cells present or
the changes are not consistent with a more precise report. In most laboratories, ASC-US changes
are reported in 3% to 5% of all samples.
ASC-US reports require a management plan. Kinney and associates have demonstrated that
although an ASC-US report is usually not indicative of HSIL, because ASC-US reports are
common, the absolute number of women with HSIL and ASC-US is high. The National Cancer
Institute sponsored a prospective, randomized study, the ASCUS LSIL Transmission Study
(ALTS), to determine the most efficacious method of further evaluation of women with this
report. One third of the women had immediate colposcopy, one third had repeat cytology in 4 to
6 months, and one third had HPV DNA testing, followed by colposcopy if the test was positive
for high-risk HPV types. Although the HPV DNA arm performed slightly better than the others,
all three approaches were found to be acceptable (Solomon and coworkers).
The Bethesda System for Reporting Cervical Cytology
Adequacy of sample
Satisfactory
Unsatisfactory
Squamous cell abnormalities
Atypical squamous cells (ASC)
ASC of undetermined significance
ASC, cannot exclude high-grade lesion
Low-grade squamous intraepithelial lesion
High-grade squamous intraepithelial lesion
Squamous cell carcinoma
Glandular cell abnormalities
Atypical glandular cells, specify site of origin, if possible
Atypical glandular cells, favor neoplastic
Adenocarcinoma in situ
Adenocarcinoma
Other cancers (e.g., lymphoma, metastatic, sarcoma)
The second abnormality is ASC-H. This report indicates that there are cells present that are
worrisome for a significant lesion, but are few in number. All women with this report should be
evaluated with a colposcopic examination as there is a high likelihood that a significant lesion is
present, as reported by Sherman and associates in 1999 .
LSIL is the next category. In the ALTS trial, it was shown that most of the women with this
report were HPV DNA positive (ALTS Report, 2000). This report is most often found to be
consistent with histology reports of CIN 1, HPV, and/or mild dysplasia. Indeed, it is not possible
with the light microscope to determine which of these lesions represents a transient viral
infection and which has the potential to progress to a higher grade lesion. Women with LSIL
cytology reports should have a colposcopic examination.
HSIL is the next category. Women with this report often have a CIN 2 or 3 lesion, and, very
occasionally, cancer. All should be evaluated with colposcopy. This is the most straightforward
of all the categories in TBS ( Sherman and associates, 2001 ). In fact, there is such good
correlation between an HSIL cytology report and the finding of CIN 2 or 3 by colposcopy, if the
two techniques do not agree, an excisional procedure is recommended to determine the actual
nature of the lesion.
If solid evidence of carcinoma is present in the cytology specimen, it will be reported as such. In
countries where cytology screening has been in place for many years, this is a rare finding. Other
malignancies can also rarely be identified on cytology, e.g., lymphoma, sarcoma, metastatic
cancer.
As discussed in Zweitig and colleagues' study, about 3 times in 1000, a cytology sample will
contain abnormal glandular cells. Sometimes these can be classified by the site of origin (e.g.,
endometrium, ovary), but often cannot. The classification of these glandular lesions is long and
complicated (see Box), but the all are managed similarly. All these women should have
colposcopy, and if no lesion is identified, additional tests are needed. Conization of the cervix,
scalpel excision is preferred to LEEP in this instance, should be performed unless there are other
explanations for the abnormal glandular cells. For example, in pregnancy and with certain
cervical infections such as Chlamydia, abnormal glandular cells are occasionally seen. If
colposcopy is negative, these women can be followed until after the condition is resolved.
However, if the abnormal glandular cells persist, conization is necessary. If the woman is older
than age 35, an endometrial biopsy should be performed. When atypical glandular cells are
present, there is approximately a 7% to 10% risk of an invasive cancer being present, making this
a very worrisome report.
The first step in the management of women with the various abnormal cytology reports is shown
in the following box. Because colposcopy is the predominant method of evaluation of women
with abnormal reports, the technique is discussed in detail below.
Natural History of Cervical Intraepithelial Neoplasia
CIN is “graded” as 1, 2, or 3 depending on the percentage of the thickness of the epithelium that
demonstrates cells with nuclear atypia. There is now general agreement that the histo-logic
changes known as CIN 1, mild dysplasia, or HPV all result from infection with HPV ( Fig. 28-5
). In the vast majority of cases, these lesions disappear spontaneously, often within weeks to
months, although, according to Moscicki and associates, it may take up to 36 months in some
cases. For reasons that have not as yet been discovered, in a few women, these infections persist
and the virus becomes integrated into the host genome, allowing for the development of
malignant transformation. Fortunately, this process is slow and requires several years from first
infection to the development of cancer.
Figure 28-5 A, Cervical intraepithelial neoplasia 1 (mild dysplasia). Atypical cells are present in the lower one third of the
epithelium. (H&E stain, ×250.) B, Low-grade squamous intraepithelial lesion cytology. These cells show an altered nuclear-tocytoplasmic ratio with enlargement and have granular chromatin. (Pap stain, ×800.)
First Step in the Evaluation of a Woman with an Abnormal Cervical Cytology Report
Squamous lesions
ASC-US
HPV DNA testing for HR types
Repeat Pap in 6 months
Colposcopy (all three options acceptable)
ASC-H
Colposcopy
LSIL
Colposcopy
HSIL
Colposcopy
Glandular lesions
All reports require colposcopy and further evaluation if negative
ASC-H, atypical squamous cells, cannot exclude a higher grade lesion; ASC-US, atypical
squamous cells of undetermined significance; HR, high risk; HSIL, high-grade intraepithelial
lesion; HPV DNA, human papillomavirus DNA; LSIL, low-grade squamous intraepithelial
lesion.
When the process of cell transformation involves one half to two thirds of the thickness of the
epithelium, it is designated CIN 2 ( Fig. 28-6 ). The process still remains reversible at this stage
with approximately half disappearing spontaneously without treatment.
Figure 28-6 Cervical intraepithelial neoplasia 2 (moderate dysplasia). The atypical cells extend approximately halfway to through
the epithelium. (H&E, ×300.)
When the neoplastic process involves the full or nearly full thickness of the epithelium, it is
designated CIN 3 ( Fig. 28-7 ). This term encompasses what was once called severe dysplasia
and carcinoma in situ. Studies demonstrated that histopathologists could not differentiate
between these categories in a consistent manner. Because CIN 3 is believed to be the precursor
to invasive cancer, treatment is recommended (see later). However, even CIN 3 changes
spontaneously disappear approximately one third of the time.
Figure 28-7 A, Cervical intraepithelial neoplasia 3 (severe dysplasia/carcinoma in situ). There is a lack of squamous maturation
throughout the thickness of the epithelium. Virtually all the cells have enlarged nuclei with granular chromatin. Note that the
basement membrane is intact showing that this process is confined to the epithelial layer only. B, High-grade squamous
intraepithelial lesion. These cells exhibit large nuclei with granular chromatin. Very little cytoplasm can be seen. (Pap stain, ×800.)
Fortunately, it takes several to many years for CIN to progress to invasive cancer (Kiviat).
Treatment at any time during the intraepithelial stage will halt further progression. There is even
an early stage of invasive cancer that is sometimes called microinvasive carcinoma. These
lesions are not visible to the naked eye, but may be identified by colposcopic examination ( Fig.
28-8 ). Management of theses lesions is covered in Chapter 29 .
Figure 28-8 Colpophotograph of a microinvasive carcinoma of the anterior lip of the cervix at 6× magnification. Abnormal vessels
can be seen, and one of these is bleeding due to the application of acetic acid.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com
Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
EVALUATION OF ABNORMAL CYTOLOGY: COLPOSCOPY
As discussed previously, the technique of colposcopy is almost always the first step in the
evaluation of women with abnormal cytology results. The only exception is the category of
ASC-US in which there are three equally appropriate first steps in the evaluation: repeat cytology
in 6 months, HPV DNA testing, and colposcopy. If the repeat cytology specimen is positive or if
the HPV DNA test is positive, the patient needs a colposcopic examination. Thus, for most
abnormal reports, colposcopy is the first step in management (ACOG Bulletin #65, September
2005).
The colposcope is a low-power binocular microscope that is mounted on a stand with a powerful
light source that is focused 30 cm beyond the front objective. Its useful magnification is from
approximately 3× to 15×. The instrument is placed just outside the vagina after a speculum has
been inserted and the cervix brought into view. After any obscuring mucus is removed with a
swab, the cervix is carefully examined for the presence of lesions. In most cases, none will be
visible. Diluted acetic acid, 3% to 5%, is then applied to the cervix, and after approximately 30
seconds, the cervix is again examined. Although the exact mechanism of action has never been
determined, the acetic acid causes areas of increased nuclear density to be seen. With experience,
a colposcopist can distinguish those tissue patterns that are associated with CIN from normal
epithelium.
A good colposcopist becomes facile in the recognition of tissue patterns, much as a pathologist
relies on that ability to make histologic diagnoses. Although published several decades ago, there
are no better descriptions and illustrations of the technique and findings of colposcopy than in
the textbooks of Coppleson and colleagues and Kolstad and Stafl.
The colposcopist must also determine whether the transformation zone (TZ) can be seen in its
entirety ( Fig. 28-9 ). The TZ is the area that lies between normal columnar epithelium and
mature squamous epithelium. The TZ is important because the vast majority of cases of
squamous neoplasia of the cervix begin in this anatomic area, probably because it is an area of
rapid cell turnover. Virtually all women are born with an area of columnar epithelium on the
portio (face) of the cervix. When the vagina becomes very acidic at the time of menarche, this
single columnar cell layer is gradually replaced by squamous epithelium through the process of
squamous metaplasia. Squamous epithelium is much more resistant to the low pH of the mature
vagina.
Figure 28-9 Normal cervix as seen through a colposcope at approximately 6× magnification. The central grapelike structures are
covered with columnar epithelium. The tissue outside this area represents squamous metaplasia. There are multiple "gland" openings
in this area, indicating that columnar epithelium is being replaced by squamous epithelium. This area between the columnar and
squamous epithelia is known as the transformation zone. (From Coppleson M, Pixley E, Reid B: Colposcopy—A Scientific and
Practical Approach to the Cervix in Health and Disease. Springfield, IL, Charles C Thomas, 1971.)
It is important to be able to assess the entire TZ. If some portions extend into the endocervical
canal beyond visibility, the examiner will not be able to determine whether there is more
significant disease above. In these cases, the lesion should not be treated with ablative methods
(see later), but rather by one of the techniques that provides a tissue sample for histologic
examination. If the entire TZ is visible, and the patient has not previously been treated for CIN,
any of the common methods of treatment of CIN can be employed. However, if there is any
finding that suggests that the lesion might extend into the canal or if it is not possible to see the
TZ, it is wise to evaluate the endocervix with either a cytologic specimen from the canal or an
endocervical curettage.
If a lesion is seen, one or more biopsy specimens should be taken to confirm the diagnosis ( Fig.
28-10 ). Because the cervix has few if any pain fibers that respond to a cutting action, the
samples can be taken with minimal or no pain. However, it is important to maintain a sharp
cutting edge on the biopsy instruments as the cervix has pain fibers that respond to stretch. If
bleeding occurs, the base of the biopsy site can be touched with Monsel's solution or a silver
nitrate stick. Cervical biopsy specimens are very small, usually only approximately 4 × 5 mm.
Therefore, no restrictions are needed. The sites heal within a few days ( Fig. 28-11 ). The
exception is if a biopsy is performed during pregnancy. In that case, the patient should be
advised to place nothing in the vagina for 3 weeks.
Figure 28-10 Cervical biopsy instruments. Punch biopsy (top). Endocervical curette (bottom).
Figure 28-11 Colpophotograph (approximately ×12) of a cervical biopsy site 72 hours after the procedure. The eschar is already
beginning to separate from the cervix.
Colposcopy during pregnancy is difficult. The cervix becomes larger, the vaginal side walls tend
to obstruct the view of the cervix, the blood supply to the cervix is increased, and decidual
changes in the epithelium can be confused with CIN. Nonetheless, colposcopy plays a key role in
a pregnant woman with an abnormal Pap test (Wright and coworkers). Invasive cancer must be
ruled out, and that determination can be made by a careful colposcopic examination of the
cervix. If there is no evidence of invasion, further evaluation can be postponed until after
delivery. Biopsies during pregnancy can be performed safely in the physician's office. However,
the examiner must be ready to respond with prolonged local pressure and, on rare occasions,
with suture ligation should brisk bleeding occur.
The only indication for an excisional procedure in pregnancy is the possible presence of invasive
disease. In those cases, a conization procedure under anesthesia is recommended.
If CIN was identified during pregnancy, a follow-up colposcopic examination should be
scheduled postpartum. However, it should not be attempted until at least 6 weeks have passed.
Many times the lesion will have disappeared, even if it was CIN 3.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com
Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
TREATMENT
There has been a great change in the approach to treatment of CIN lesions over the past 30 years.
Now that it is known that the vast majority of the lesions disappear spontaneously, treatment is
indicated for only those lesions that have demonstrated a potential for further progression.
Cervical Intraepithelial Neoplasia 1
Treatment of CIN 1 is no longer the preferred method of management of these lesions at any age.
Exceptions should be made on a patient-by-patient basis and only if the lesion has persisted for at
least 12 months. Treatment of CIN 1 in women younger than age 21 is not recommended, even if
the lesion persists. Virtually all CIN 1 is a manifestation of a transient HPV infection, and these
resolve with the development of anti-HPV antibodies. Although many lesions regress within
months, resolution may take up to 36 months. Because the lesion is so far removed from cancer,
it should not be regarded as a serious finding. Although patients with CIN 1 require follow-up to
ensure that the lesion regresses, clinicians should not present the finding in a way that alarms the
patient.
Some small fraction of CIN 1 lesions progress to CIN 2 or 3, but, at present, it is not possible to
determine which have that potential. However, because the treatment of CIN 2 and 3 is easy and
office-based, there is no penalty for waiting to determine whether spontaneous resolution of a
CIN 1 lesion will occur. In addition, all the treatments are associated with a risk of long-term
complications such as cervical stenosis and premature delivery, according to Kyrgiou and
associates ( Fig. 28-12 ).
Figure 28-12 Mild cervical stenosis following cryocautery for cervical intraepithelial neoplasia 2. The colposcopic examination is
unsatisfactory because the transformation zone cannot be seen (colpophotograph approximately ×6).
Cervical Intraepithelial Neoplasia 2
The majority of CIN 2 lesions also regress spontaneously. For many years, virtually all CIN 2
lesions were treated. It slowly became more common not to treat women younger than age 21.
As the transient nature of these lesions has become more evident, many clinicians now follow
patients beyond age 21, particularly if they are not through with childbearing. If a lesion
progresses to CIN 3, it should be treated.
Cervical Intraepithelial Neoplasia 3
Although some of these lesions regress, most either persist or, in some cases, progress to
invasive cancer ( Fig. 28-13 ). Therefore, according to ACOG Practice Bulletin 66, they should
be treated. If the involved area is removed in its entirety, the disease is cured. Several methods
have similar treatment success, and these are discussed.
Figure 28-13 Extensive cervical intraepithelial neoplasia 3 (CIN 3) lesion covering most of the epithelium visible in this
colpophotograph. The predominant feature is a mosaic pattern. There is “umbilication” of many of the tiles with a punctuate vessel, a
common feature of CIN 3. Although this large lesion needs to be examined carefully for evidence of atypical vessels, a hallmark of
invasive cancer, none are seen in this view. (Colpophotograph ×8.) (From Kolstad P, Stafl A: Atlas of Colposcopy. Baltimore,
University Park Press, 1972.)
Women who have had one CIN 3 lesion are slightly more likely to develop another lesion in the
future. Therefore, long-term follow-up is necessary.
Treatment Methods
The goal of treatment of CIN is to remove the lesion, and any technique that accomplishes that
goal can be used. Currently, most treatment is office-based. Indeed, it is hard to justify the
expense and increased risk of treatment under general anesthesia, except in rare cases with
specific indications.
Treatment can be accomplished either by ablation (cryotherapy, thermoablation, CO2 laser
ablation) or excision (LEEP [also known as LLETZ], cold knife conization, CO2 laser
conization). All these methods have first-treatment success rates of approximately 95%, and the
choice of method depends on the availability of equipment and the experience and expertise of
the clinician ( Martin-Hirsch and colleagues, Cochrane Database, 1999 ) Hysterectomy is not
recommended for treatment of CIN, even if cervical biopsy specimens have been reported as
showing “carcinoma in situ.” As early as 1976, Kolstad and Klem demonstrated that
hysterectomy for carcinoma in situ was no better than an excisional cone. In addition,
hysterectomy carries risks that are much more common and serious than office-based therapy of
CIN 3.
When a first treatment fails, it is because of incomplete excision of the entire lesion. Involved
tissue can be left behind either in the endocervix or on the exocervix. The latter does not
represent a difficult treatment problem as colposcopy can easily identify the area and office
excision is both easy and curative.
When the endocervical margin of an excised specimen is positive for CIN, the patient should be
followed with endocervical evaluation and colposcopy in 3 to 4 months. Many of these women
will not have persistent disease, according to Lopes and colleagues, probably because very little
of the lesion remained and the normal healing process destroyed the remainder. However, when
there is evidence that CIN remains in the endo-cervical canal 4 to 6 months after the procedure,
repeated excision of the canal is indicated. An endocervical margin that is positive is not an
indication for hysterectomy or immediate repeat excision.
Ablative Methods
Cryotherapy
This outpatient method was the most commonly used treat-ment for CIN lesions in the 1970s and
1980s, but has largely been supplanted by LEEP. If patients are carefully selected, the success
rate is approximately 95%. Larger CIN lesions have higher failure rates, most likely because the
whole lesion is not covered by the cryoprobe. It is not appropriate to use cryo-therapy if the
lesion extends into the endocervix.
The procedure is simple. After colposcopy and sampling has shown that the lesion is confined to
the exocervix, a probe is selected that will cover the entire lesion ( Fig. 28-14 ). In most systems,
N2O is used as the refrigerant. The probe is applied to the cervix and the system is activated. The
cervix will freeze quickly, but the probe must remain in place until the ice ball that forms extends
to at least 5 mm beyond the edge of the instrument. In most cases, this takes 3 to 4 minutes. The
refrigerant is then turned off, and the probe allowed to thaw and separate from the cervix.
Several studies have suggested that repeating the freeze–thaw cycle a second time results in a
higher success rate, whereas others have shown equal success with a single freeze.
Figure 28-14 Three varieties of cryotherapy probes.
Most patients experience almost no discomfort during the procedure, although some complain of
menstrual-type cramping. Because the tissue that was destroyed remains on the cervix, within a
few hours to a day, the patient will begin to experience vaginal discharge. As the tissue sloughs,
the amount of dis-charge increases, and malodor is common. It may take as long as 3 weeks for
the discharge to stop. The patient should be cautioned to place nothing in the vagina for at least 3
weeks after the procedure to avoid causing dislodgment of the escar.
The first follow-up should occur in approximately 4 to 6 months and include cytology and
colposcopy. The cytology sample should include the endocervix.
Short-term complications from the procedure include the nuisance of the discharge and
occasionally bleeding. Long-term complications include cervical stenosis and a small increase in
preterm labor. Unfortunately, the instrument was sometimes used by inexperienced individuals,
and cases of invasive cancer following treatment were reported. In almost every case, an
appropriate evaluation had not been performed before treatment.
Thermoablation
This technique is almost never used in the United States at present. Various loops, needles, and
paddles were used to destroy CIN lesions. Although the success rate was as high as other
techniques, it often required general anesthesia and perhaps resulted in more cervical stenosis
than other methods.
CO2 Laser Ablation
This technique became available to clinicians in the 1980s. When a focused CO2 laser beam is
directed at the cervical epithelium, the laser energy is absorbed by the water in the cells. The
water turns to steam and the cell wall disrupts, killing the cell. The cell protein is largely
“exploded” in a plume of smoke that is drawn out of the vagina by suction. Because very little
dead tissue is left after the procedure, there is no prolonged vaginal discharge as there is with
cryotherapy. The success rate is similar to other techniques.
The technique became popular both because the area of tissue destruction could be minimized
and there was no prolonged discharge as with cryotherapy. In addition, because the instrument is
attached to a colposcope, usually those who used the technique were very familiar with CIN.
Additional training is required as treatment success depends on the correct choice of laser energy
delivered (calculated as a “power density”) and proper depth and extent of treatment.
For several years, CO2 laser ablation was the method of choice for treatment of CIN. It can be
performed in the office with no anesthesia. (I have personally treated several hundred patients in
the office with this technique.) However, the equipment is very expensive. When LEEP became
available, laser treatment began to wane. Currently, it is used almost exclusively in those cases in
which there the lesion extends far out onto the exocervix. In these cases, CO2 laser can be
effective with less tissue destruction than other methods.
Excisional Methods
Loop Electrosurgical Excision (LEEP)
This procedure is currently the most common method for the treatment of CIN 2 and 3. It
involves the removal of the TZ of the cervix under local anesthesia and can be performed safely
and without discomfort in the office.
Typically, 3 or 4 mL lidocaine with epinephrine is injected into the cervix in a circumferential
manner, making five to eight injections at the distal edge of the resection margin. The lidocaine
is injected just under the epithelium rather than deep into the cervix. One to 2 minutes should be
allowed for the epinephrine to cause vasoconstriction. A wire loop attached to a cautery machine
that can provide a cutting current is then used to remove the tissue. Various sizes of loops are
available ( Fig. 28-15 ). If there is any bleeding, the edge of the defect can be cauterized with a
ball electrode attached to the current generator. In most cases, there is less than 5 mL of blood
loss. There is no reason to perform curettage of the endocervical canal above the resected margin
as the management of the patient is the same whether the sample is positive or negative, and
curettage can cause additional scarring.
Figure 28-15 Examples of electrodes (Utah Medical Corp., Midvale, UT) used for a loop electroexcision procedure. The width of
the excised tissue specimens can range from 1.0 to 2.0 cm, and the specimen depth can be adjusted by sliding the guard attached to
the electrode shaft. Following excision, the base of the cervix is often gently cauterized with a ball electrode. (Courtesy Steven E.
Waggoner, MD, The University of Chicago.)
The LEEP specimen is sent to the laboratory for histologic evaluation. In most cases, the whole
lesion will have been excised and the margins of the specimen will be free of CIN. If either
margin is positive for CIN, a colposcopic examination should be performed with the first followup cytology in 4 to 6 months. If the exocervical margin was positive, that area should be
evaluated carefully. If a small bit of the original lesion was left behind, treatment is usually very
easy.
If the endocervical margin showed signs of CIN, there is no urgency to perform a repeat
procedure. Many of these women will have no residual disease at the time of follow-up. In all
cases, the endocervix should be evaluated either by cytology or endocervical curettage. Only if
persistent CIN is demonstrated in the canal should a repeat LEEP be performed. A positive
endocervical margin or evidence of persistent disease in the canal is not an indication for
hysterectomy. Indeed, hysterectomy is almost never indicated for the treatment of CIN. Only if
CIN 3 persists despite multiple treatment attempts should it be considered, and evaluation by an
expert colposcopist is strongly recommended.
Cold Knife Conization
This term is used to describe removal of the CIN lesion with a scalpel (the cold knife). Before
colposcopy was widely used in the evaluation of women with abnormal Pap tests, cold knife
conization was the standard diagnostic procedure. Under general anesthesia, the cervix would be
stained with an iodine-containing solution, and all the epithelium that did not stain would be
removed. The knife would be angled toward the endocervical canal, thus removing a coneshaped piece of tissue that could be evaluated by a pathologist. Often, extensive suturing of the
defect bed would be performed.
With the advent of colposcopy and office-based therapy, cold knife conization is used less and
less often. For the evaluation of squamous lesions, it offers no advantage over LEEP, which does
not require the use of general anesthesia. Its sole unique indication at present is in the diagnostic
evaluation of patients with glandular lesions in which the absence of the thermal artifact
introduced at the endocervical margin by LEEP is problematic. In addition, some clinicians still
use the technique when a LEEP has failed, although there are few data to support this approach.
The technique has evolved over time. Because colposcopy should always be performed before
cold knife conization, the exocervical extent of the lesion will be known. There is no reason to
excise more tissue than necessary, so the excision should be tailored to the lesion. In many cases,
a small cylinder of tissue can be removed instead of the larger “cone.” In most cases, bleeding
can be controlled with application of Monsel's solution (ferrous subsulfate) to the defect,
especially if a vasoconstrictive solution is injected into the cervix before the excision. Sutures are
only rarely necessary. If a bleeding site is encountered, a simple or figure-of-eight ligature of the
bleeder suffices. There is no indication for the Sturmdorf sutures often used in the past. This
technique rolled the exocervical epithelium into the canal, making subsequent evaluation
virtually impossible. In addition, it is not necessary to control bleeding.
Follow-up
All the treatment methods described have a first-time success rate of approximately 95% (
Martin-Hirsch and colleagues, Cochrane Database, 1999 ). According to ACOG Practice Bulletin
Number 66, because women who have been treated for CIN 2 and 3 have a somewhat higher risk
of developing a new lesion, they should be followed closely. A first Pap test should be taken 4 to
6 months after the treatment and repeated at that interval until three negative cytology results
have been reported. At that time, the woman can be returned to annual screening examinations.
If a Pap test is reported as showing a squamous abnormal-ity, colposcopy should be performed.
The examination should include an evaluation of the endocervix, either with cytology or
endocervical curettage. If a lesion is seen on the distal exocervix, it most likely represents an
edge that was not included in the initial treatment. However, if a lesion is either seen to be
involving the endocervical canal or if the endocervical specimen is positive, an excisional
procedure that includes the endocervix should be performed.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com
Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
VAGINAL INTRAEPITHELIAL NEOPLASIA
The least common malignancy of the lower female genital tract is vaginal cancer. The lesions are
virtually all squamous carci-nomas, and it it believed that most are preceded by an intraepithelial
lesion (Audet-Lapointe and coworkers, Cardosi and colleagues). However, cancer is so rare that
it is no longer advised to screen for the malignancy in women who have had a total hysterectomy
unless they have a history of CIN 2 or 3. In fact, because the majority of abnormal vaginal
cytology specimens are falsely positive, women who have undergone hysterectomy should be
actively discouraged from having cytology samples taken. The exceptions, according to
Kalogirou and colleagues, are women who have been treated for HSIL, women exposed in utero
to diethylstilbestrol, and women who are immunocompromised.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com
Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
VULVAR INTRAEPITHELIAL NEOPLASIA
Vulvar cancer occurs primarily in postmenopausal women who have had an untreated
preinvasive lesion for many years. Unfortunately, cytologic screening of the vulva is not useful
as it is unreliable. Most cases are identified either through a patient complaint of a “sore” or an
area that “itches.” Some asymptomatic cases are identified when a clinician performs a vulvar
examination and identifies an abnormal-appearing area.
Natural History
The natural history of vulvar intraepithelial neoplasia (VIN) lesions is not as well worked out as
for CIN lesions. Although it is believed that most cases of invasive squamous cancer of the vulva
go through an intraepithelial stage similar to cervical lesions, is not known for certain (van Seters
and colleagues). It is known that many invasive squamous cancers of the vulva contain HPV
DNA, but the percentage of positive cases is lower than those of the cervix where it is almost
100%. When vulvar cancer occurs in a reproductive-age woman (a rather rare event), HPV DNA
can almost always be identified. In postmenopausal women, the percentage of cancers with HPV
DNA is small.
Vulvar histology is much less helpful than cervical histology. For example, it is known that a
fraction of CIN 3 lesions will progress to cancer if not treated. However, a much larger frac-tion
of VIN 3 lesions disappear spontaneously, particularly when they occur in women younger than
age 35. Currently, VIN 1 lesions are not treated, as are fewer and fewer VIN 2 lesions.
Invasive vulvar cancer is probably preceded by VIN 3 in the majority of cases. However, many
VIN 3 lesions never progress, especially when they occur in women younger than age 35. In that
age group, VIN 3 most often represents HPV infection. Because there is no way to distinguish
between those that will and will not regress, treatment of VIN 3 is still recommended at all ages.
Treatment of VIN
Before a decision to treat is made, following Wright and Chapman, it is important to have
histologic confirmation of the lesion, both to be certain that it is truly VIN 3 and also to rule out
invasion ( Fig. 28-16 ). For some reason, many clinicians are reluctant to perform vulvar biopsies
in the office. These can be done with a minimal of discomfort by using a very small (30 gauge)
needle and lidocaine.
Figure 28-16 Vulvar intraepithelial neoplasia (VIN) 3 lesion as seen through a colposcope after the application of acetic acid. A
second lesion is out of focus, but can be seen in the background. VIN is often multifocal.
If a decision is made to treat a VIN lesion, there are several different techniques that can be used.
The goal is to destroy the lesion, and any method that removes the epithelium can accomplish
that goal. Unlike the cervix, there are no crypts (commonly called glands) in the vulvar
epithelium, so excisions can be very superficial.
In the past, excision with a scalpel was used almost universally to treat VIN. Fortunately, many
of these lesions are small and require only a small excision, especially in younger women.
Because of the multiple folds of skin on the vulva, it is almost always possible to close the
incision primarily. If lesions recur, a relatively common event, there may not be sufficient skin
remaining for primary closure without relaxing incisions. It is not necessary to remove more than
the lesion. In the past, “skinning vulvectomy” in which all the skin of the vulva was removed and
a skin graft placed on the defect, was commonly used to treat vulvar carcinoma in situ (VIN 3).
That procedure is no longer indicated, as simple excision of the individual lesion(s) has a similar
cure rate.
The CO2 laser can be used to ablate areas of VIN. It is especially useful in the area surrounding
the clitoris where it is appropriate to remove the minimum amount of tissue consistent with
removal of the entire lesion. However, the skill of the operator is important with this technique as
the ablation should not be carried through the dermis. The raw edges, actually burns, left after
laser surgery are much more painful than excision and primary closure.
Cryosurgery has been used, but there is poor control of the depth of the tissue destruction and
healing is slow and painful. LEEP is used by some. There is better control of depth with LEEP
than with cryosurgery, but it is still rarely used.
A novel approach in young women with VIN 3 lesions, particularly in the clitoral area, is the
application of imiquimod. Although no large studies have been reported, small case series have
shown a good rate of clearance for those who can tolerate the irritation that always accompanies
its use. Long-term data are also not available.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com
Katz: Comprehensive Gynecology, 5th ed.
Copyright © 2007 Mosby, An Imprint of Elsevier
BIBLIOGRAPHY
ACOG Practice Bulletin Number 45. Cervical cytology screening. Obstet
Gynecol 2003; 102:417-427.
ACOG Practice Bulletin Number 61. Human papillomavirus. Obstet Gynecol 2005; 105:905918.
ACOG Committee Opinion Number 330. Evaluation and management of abnormal cervical
cytology and histology in the adolescent. Obstet Gynecol 2006; 107:963-968.
ACOG Practice Bulletin Number 66. Management of abnormal cervical cytology and histology.
Obstet Gynecol 2005; 106:645-664.
ACOG Practice Bulletin Number 35. Diagnosis and treatment of cervical carcinomas. Obstet
Gynecol 2002; 99:855-867.
Aldieh L, Klein RS, Burk R, et al: Prevalence, incidence and type-specific persistence of human
papillomavirus in human immunodeficiency virus (HIV)-positive and HIV-negative women. J
Infect Dis 2001; 184:682-690.
Audet-Lapointe P, Body G, Vauclair R, et al: Vaginal intraepithelial neoplasia. Gynecol
Oncol 1990; 35:232-239.
Bellinson J, Qiao YL, Pretorius RG, et al: Shanxi province cervical cancer screening study: A
cross-sectional comparative trial of multiple techniques to detect cervical neoplasia. Gynecol
Oncol 2001; 83:439-444.
Bosch FX, Manos MM, Munoz N, et al: International Biological Study on Cervical Cancer
(IBSCC) Study Group. Prevalence of human papillomavirus in cervical cancer: A Worldwide
perspective. J Natl Cancer Inst 1995; 87:796-802.
Broder S: Rapid Communication—the Bethesda System for reporting cervical/vaginal cytologic
diagnoses—report of the 1991 Bethesda Workshop. JAMA 1992; 267:1892.
Brown AD, Garber AM: Cost effectiveness of 3 methods to enhance the sensitivity of
Papanicolaou testing. JAMA 1999; 281:347-353.
Cardosi RJ, Bomalaski JJ, Hoffman MS: Diagnosis and management of vulvar and vaginal
intraepithelial neoplasia. Obstet Gynecol Clin North Am 2001; 28:685-702.
Coppleson M, Pixley E, Reid B: Colposcopy—A Scientific and Practical Approach to the Cervix
in Health and Disease, Springfield, IL, Charles C Thomas, 1971.
Fahey MT, Irwig L, Macaskill P: Meta-analysis of Pap test accuracy. Am J
Epidemiol 1995; 141:680-689.
Ho GYF, Bierman R, Beardsley L, et al: Natural history of cervicovaginal papillomavirus
infection in young women. N Engl J Med 1998; 338:423-428.
Ho GYF, Burk RD, Klein S, et al: Persistent genital human papillomavirus infection as a risk
factor for persistent cervical dysplasia. J Natl Cancer Inst 1995; 87:1365-1371.
Human papillomavirus testing for triage of women with cytologic evidence of low-grade
squamous intraepithelial lesions: Baseline date from a randomized trial. The atypical squamous
cells of undetermined significance/low-grade squamous intraepithelial lesions triage study
(ALTS) group. J Natl Cancer Inst 2000; 92:397-402.
Hutchinson ML, Zahniser DJ, Sherman ME, et al: Utility of liquid-based cytology for cervical
carcinoma screening: Results of a population-based study conducted in a region of Costa Rica
with a high incidence of cervical carcinoma. Cancer 1999; 87:48-55.
Kalogirou A, Antoniou G, Karakitsos P, et al: Vaginal intraepithelial neoplasia (VAIN)
following hysterectomy in patients treated for carcinoma in situ of the cervix. Eur J Gynaecol
Oncol 1997; 18:188-191.
Kim JJ, Wright TC, Goldie SJ: Cost-effectiveness of alternative triage strategies for atypical
squamous cells of undetermined significance. JAMA 2002; 287:2382-2390.
Kinney WK, Manos MM, Hurley LB, Ransley JE: Where's the high-grade cervical neoplasia?
The importance of minimally abnormal Papanicolaou diagnoses. Obstet Gynecol 1998; 91:973976.
Kiviat N: Natural history of cervical neoplasia: Overview and update. Am J Obstet
Gynecol 1996; 175:1099-1104.
Kolstad P, Klem V: Long-term follow-up of 1121 cases of carcinoma in situ. Obstet
Gynecol 1976; 48:125.
Kolstad P, Stafl A: Atlas of Colposcopy, Baltimore, University Press, 1972.
Koutsky LA, Galloway DA, Holmes KK: Epidemiology of genital human papillomavirus
infection. Epidemiol Rev 1988; 10:122-163.
Kyrgiou M, Koliopoulos G, Martin-Hirsch P, et al: Obstetric outcomes after conservative
treatment for intraepithelial or early invasive cervical lesions: Systematic review and metaanalysis. Lancet 2006; 367:489-498.
Lopes A, Morgan P, Murdoch J, et al: The case of conservative management of “incomplete
excision” of CIN after laser conization. Gynecol Oncol 1993; 49:247-249.
Manos MM, Kinney WK, Hurley LB, et al: Identifying women with cervical neoplasia: Using
human papillomavirus DNA testing for equivocal Papanicolaou results. JAMA 1999; 281:16051610.
Mao C, Koutsky LA, Ault KA, et al: Efficacy of human papillomavirus-16 vaccine to prevent
cervical intraepithelial neoplasia: A randomized controlled trial. Obstet Gynecol 2006; 107:1827.
Martin-Hirsch P, Lilford R, Jarvis G, Kitchner HC: Efficacy of cervical-smear collection
devices: A systematic review and meta-analysis. Lancet 1999; 354:1763-1770.
Martin-Hirsch PL, Paraskevaidis E, Kitchener H: Surgery for cervical intraepithelial neoplasia.
Cochrane Database Syst Rev 1999; 3:(CD001318)
Moscicki AB, Shiboski S, Broering J, et al: The natural history of human papillomavirus
infection as measured by repeated DNA testing in adolescent and young women. J
Pediatr 1998; 132:277-284.
Moscicki AB, Shiboski S, Hills NK, et al: Regression of low-grade squamous intra-epithelial
lesions in young women. Lancet 2004; 364:1642-1644.1678–1683
Munger K, Baldwin A, Kirsten M, et al: Mechanisms of human papillomavirus-induced
oncogenes. J Virol 2004; 78:11451-11460.
Nanda K, McCrory DC, Myers ER, et al: Accuracy of the Papanicolaou test in screening for and
follow-up of cervical cytologic abnormalities: A systemic review. Ann Intern
Med 2000; 132:810-819.
Noller KL: Cervical cytology screening and evaluation. Obstet Gynecol 2005; 106:391-397.
Noller KL, Bettes B, Zinberg S, Schulkin J: Cervical cytology screening practices among
obstetrician-gynecologists. Obstet Gynecol 2003; 102:259-265.
Noller KL, O'Brien PC, Melton 3rd LJ, et al: Coital risk factors for cervical cancer. Sexual
activity among white middle class women. Am J Clin Oncol 1987; 10:222-226.
Papanicolaou GN, Traut HF: The diagnostic value of vaginal smears in carcinoma of the uterus.
Am J Obstet Gynecol 1941; 42:193-206.
Pearce KF, Haefner HK, Sarwar SF, Nolan TE: Cytopathological findings on vaginal
Papanicolaou smears after hysterectomy for benign gynecologic disease. N Engl J
Med 1996; 335:1559-1562.
Sawaya GF, Grady D, Kerlikowske K, et al: The positive predictive value of cervical smears in
previously screened postmenopausal women: The Heart and Estrogen/Progestin Replacement
Study (HERS). Ann Intern Med 2000; 133:942-950.
Schiffman M, Herrero R, Hildesheim A, et al: HPV DNA testing in cervical cancer screening:
Results from women in a high-risk province of Costa Rica. JAMA 2000; 283:87-93.
Schuman P, Ohmit SE, Klein RS, et al: Longitudinal study of cervical squamous intraepithelial
lesions in human immunodeficiency virus (HIV)-seropositive and at-risk HIV-seronegative
women. J Infect Dis 2003; 188:28-36.
Sherman ME, Solomon D, Schiffman MASCUS LSIL Triage Study Group: Qualification of
ASCUS: A comparison of equivocal LSIL and equivocal HSIL cervical cytology in the ASCUS
LSIL Triage Study. Am J Clin Pathol 2001; 116:386-394.
Sherman ME, Tabbara SO, Scott DR, et al: “ASCUS rule out HSIL”: Cytologic features,
histologic correlates and human papillomavirus detection. Mod Pathol 1999; 12:335-343.
Solomon D, Schiffman M, Tarone RALTS Study Group: Comparison of three management
strategies for patients with atypical squamous cells of undetermined significance: Baseline
results from a randomized trial. J Natl Cancer Inst 2001; 93:293-299.
USPHA/IDSA guidelines for the prevention of opportunistic infections in persons infected with
human immunodeficiency virus. MMWR Recomm Rep 1999; 48:1-59.
van Seters M, van Beurden M, de Crain AJ: Is the assumed history of vulvar intraepithelial
neoplasia III based on enough evidence? A systematic review of 3322 published patients.
Gynecol Oncol 2005; 97:645-651.
Wheeler CM, Greer CI, Becker TM, et al: Short-term fluctuations in the detection of cervical
human papillomavirus DNA. Obstet Gynecol 1996; 88:261-268.
Winer RL, Lee SK, Hughes DE, et al: Genital human papillomavirus infection: Incidence and
risk factors in a cohort of female university students. Am J Epidemiol 2003; 157:218-226.
Wright VC, Chapman WB: Colposcopy of intraepithelial neoplasia of the vulva and adjacent
sites. Obstet Gynecol Clin North Am 1993; 20:231-255.
Wright Jr TC, Cox JT, Massad LS, et al: American Society for Colposcopy and Cervical
Pathology. 2001 consensus guidelines for the management of women with cervical intraepithelial
neoplasia. Am J Obstet Gynecol 2003; 189:295-304.
Wright TC, Cox JT, Massad LS, et al: 2001 consensus guidelines for the management of women
with cervical cytological abnormalities. JAMA 2002; 287:2120-2129.
Wright Jr TC, Cox JT, Massad LS, et al: ASCCP-Sponsored Consensus Conference. 2001
Consensus Guidelines for the management of women with cervical cytological abnormalities.
JAMA 2002; 287:2120-2129.
Wright Jr TC, Schiffman M, Soloman D, et al: Interim guidance for the use of human
papillomavirus DNA testing as an adjunct to cervical cytology for screening. Obstet
Gynecol 2004; 103:304-309.
Zweitig S, Noller K, Reale F, et al: Neoplasia associated with atypical glandular cells of
undetermined significance on cervical cytology. Gynecol Oncol 1997; 65:314-318.
Email to Colleague Print Version
Copyright © 2007 Elsevier Inc. All rights reserved. - www.mdconsult.com