Chapter 11 notes - Castle High School
advertisement

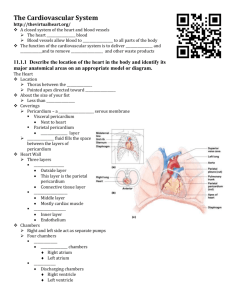
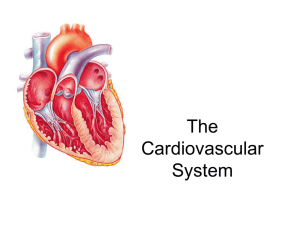
The Cardiovascular System Chapter 11 Cardiovascular Overview • Major function: transportation • Blood transports oxygen, nutrients, cell wastes, hormones, and many other substances vital for homeostasis to and from the cells The Heart: Anatomy • Enclosed within the mediastinum • Apex points toward the left at approximately the 5th intercostal space • Enclosed by double-walled pericardium (sac) Pericardium • Outer Layer: fibrous pericardium • Protection & anchors heart to surrounding structures • Inner Layer: serous pericardium • slippery two-layer structure • parietal layer – lines fibrous pericardium • visceral layer – hugs heart and is part of heart wall (also called epicardium) • produces serous fluid to allow the heart to beat in a relatively frictionless environment Heart Wall: three layers • Epicardium: visceral pericardium • Protects by producing serous fluid • Myocardium: thick bundles of cardiac muscle twisted and whorled into ringlike arrangements • Contractile layer of heart • Endocardium: thin, glistening sheet of endothelium that lines the heart chambers • Continuous with the linings of the blood vessels leaving and entering the heart Heart Wall • Chambers of the Heart • Four chambers: two left & two right separated by septum • Each lined with endocardium • Upper: right & left atria - receiving chambers for blood from the body • Lower: right & left ventricles: thick-walled, discharging chambers, pumps blood from the heart circulation throughout the body Circulation & Blood Flow • Heart acts as a double pump • Pulmonary circulation: • Superior & inferior venae cavae brings blood to the right atrium • Flows into right ventricle and is pumped through pulmonary trunk, which splits into pulmonary arteries (right & left) to take blood to the lungs • Oxygen & carbon dioxide are exchanged in the lungs, and the blood is returned to the left atrium through the four pulmonary veins • Systemic circulation: • Blood flows into the left ventricle from the left atrium, and is pumped out of the heart into the aorta • Systemic arteries branch to supply body tissues and oxygen-poor blood circulates via the systemic veins back to the superior & inferior venae cavae to the right side of the heart Heart Valves • Four valves allow blood to flow in only one direction through heart chambers • Atrioventricular (AV) valves: located between atrial and ventricular chambers on each side (open during heart relaxation) • Bicuspid (mitral) valve – left AV valve (has two flaps of endocardium) • Tricuspid valve – right AV valve (has three flaps of endocardium) • Chordae tendinae – anchor flaps of valves to walls of the ventricles so that valves can prevent backflow of blood when ventricles contract • Semilunar valves: guard bases of two large arteries leaving the ventricular chambers (open during heart contraction) • Pulmonary semilunar valve: between right ventricle and pulmonary artery • Aortic semilunar valve: between left ventricle and aorta Cardiac Circulation • Blood contained in the heart does not nourish the myocardium • Coronary arteries (right and left): branch from the base of aorta and encircle the heart as the functional blood supply • Oxygenates and nourishes the heart muscle • If blocked, causes ischemia (chest pain) and eventually myocardial infarction • Coronary veins: myocardium drains into coronary veins, which empty into an enlarged vessel (coronary sinus) • Coronary sinus empties into right atrium Physiology of the Heart • In one day, pumps 6 liters of blood through the blood vessels over 1000 times • Made of cardiac muscle – contract spontaneously and independently, even if all nervous connections are severed • Fibers shorter than skeletal muscle & branching with striations • One central nucleus • Intercalated disc where cells join • Involuntary muscle • Muscle cells in different areas of the heart have different rhythms, so need to be coordinated with a control system • Atrial cells = 60 bpm • Ventricular cells = 20-40 bpm • Two systems regulate heart activity: • Autonomic nervous system: increase & decrease heart rate • Intrinsic conduction system (nodal system): built into the heart tissue & sets basic rhythm Intrinsic Conduction System • Tissue is a cross between muscle and nervous tissue • Causes heart muscle depolarization in only one direction – from the atria to the ventricles • Contraction rate: 75 bpm as coordinated unit • Sinoatrial node: located in right atrium; increases rate of depolarization; starts heartbeat and sets pace (pacemaker) • Atrioventricular (AV) node: junction of atria & ventricles; in septum between two atria; only way impulse gets to ventricles (heart block if not conducting impulse) • Atrioventricular (AV) bundle (bundle of His) and right and left bundle branches located in the interventricular septum (wringing contraction of ventricle) • Purkinje fibers – spread within the muscle of the ventricle walls (causes contraction from apex to atria to eject blood superiorly) Cardiac Cycle • Based on pressure and conduction of impulses to cause contractions • One complete heartbeat • Recorded on electrocardiogram (ECG) • P wave: atrial depolarization • QRS wave: rapic ventricle depolarization • T wave: ventricle repolarization • Cardiac Cycle: Fig 11.8 page 366 • ECG: “A Closer Look” pg. 367 Cardiac Cycle & Heart Sounds • Atria contract simultaneously, then as they relax the ventricles contract • Systole: heart contraction (ventricular) • Diastole: heart relaxation (ventricular) • Cardiac cycle: events of one complete heartbeat, during which both atria and ventricles contract & relax • Mid-to-late diastole: semilunar valves closed and AV valves open • Ventricular systole: AV valves close, semilunar valves open • Early diastole: semilunar valves shut and AV valves forced open • Heart sounds – “lub-dup” • “lub” = closing of AV valves; “dup” = semilunar valves close at end of systole Cardiac Output • Cardiac output (CO): amount of blood pumped out by each side of the heart in 1 minute • Stroke volume (SV): volume of blood pumped out by a ventricle with each heartbeat • CO = HR x SV • Average CO = 75 bpm x 70 ml/beat = 5250 ml/min • Entire blood supply passes through the body once each minute (adult blood volume is approximately 6000 ml) • Blood Vessels Vascular system: closed transport system of blood vessels • Blood flows from arteries (0.1 mm-1 cm) arterioles (10-100 µm) capillary beds venules (10-100 µm) veins (0.11 mm) Microscopic Anatomy of Blood Vessels • Blood vessels have three coats, or tunics (except capillaries) • Tunica intima: lines the interior of the vessels; thin layer of endothelium • Tunica media: bulky middle coat; smooth muscle and elastic fibers (constricts or dilates blood vessels) • Tunica externa (adventitia): outermost tunic; supports and protects vessels Structural Differences in Blood Vessels Arteries • • • Take blood away from heart in circulation Thickest walls (thick tunica media) to withstand continuous changes in pressure Have additional elastic membranes in the tunica media Veins • • • • Take blood towards the heart in circulation Thinner tunica media, so larger lumen Veins have valves to prevent backflow of blood and ensure that venous return equals cardiac output (amount of blood pumped out of heart) Muscles surrounding veins aid in venous return as well Capillaries • • • Exchange of materials between blood and tissues happens through the walls of capillaries Wall is one cell layer thick (only tunica intima) Form capillary beds in tissues (flow from arteriole to venule through capillary bed is called microcirculation) Capillary Exchange • Number of capillaries in a tissue is related to metabolic activity • Types of capillary exchange: • Diffusion (O2, CO2, glucose, amino acids, hormones) & osmosis (water) • high to low (slow process) • Proteins & blood cells are too large to leave the vessel • Transcytosis – active transport, material enclosed in pinocytic vessels (large lipid insoluble molecules, i.e. insulin) • Bulk flow – pressure driven flow of particles that regulates relative volume of blood and interstitial fluid (faster process) • Blood pressure pushes fluids out of the vessels; osmotic pressure draws fluid back in (filtration and reabsorption) • Lymphatic system returns fluid left in the interstitial fluid back to the blood Vital Signs: Physiology of Circulation • arterial pulse, blood pressure (along with respiratory rate & body temperature) are vital signs taken in clinical setting • Arterial pulse: arteries expand and recoil with each beat of the left ventricle and creates a pulse (pressure wave) • normally equals heart rate: 70-76 bpm in normal resting person • influenced by activity, postural changes, emotions • Blood pressure: pressure blood exerts against the inner walls of blood vessels that keeps blood circulating continuously even between heartbeats • Highest in arteries • Systolic – peak of ventricular contraction; diastolic – ventricles relaxing • Normal is 120/80 mm Hg • Figure 11.22 on page 386 Factors Affecting Blood Flow • Blood flow: volume of blood that flows through any tissue/time (mL/min); moves down pressure gradient • Affected by: • Blood pressure: decreases as move away from aorta • Resistance: friction increases as size of lumen decreases; differences in blood viscosity; friction increases as blood vessel length increases • Venous return: valves keep blood from backing up • Velocity: flows faster in larger vessels