Cardovascular System The Heart Chap. 12
advertisement

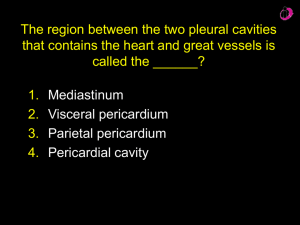
Cardiovascular System The Heart Chap. 12 The Cardiovascular system is comprised of the heart, blood vessels, & blood The heart acts as a “pump”, creating pressure which causes blood to move through the blood vessels of the body, allowing O2 & nutrients to be distributed to, & wastes removed from, body tissues Heart Anatomy Overview Play Heart Anatomy video Anatomical Features of the Heart The heart lies within the mediastinum of the thoracic cavity Hollow muscular organ with four internal chambers (2) atria (lt. atrium & rt. atrium)receive blood from veins (2) ventricles (lt. ventricle & rt. ventricle)- pump blood into arteries Superior aspect of heart is the “base”, where the blood vessels attach; Inferior is the “apex”, which rests on the relaxed diaphragm Pericardium The heart lies enclosed within pericardial membranes pericardium (pericardial sac) – outer layer of dense CT that protects & anchors Serous pericardium – double layered membrane with “pericardial fluid” between Fibrous Parietal pericardium – lines the pericardial sac Visceral pericardium – covers the heart; also known as the “epicardium” etal cardium Figure 12.2 Layers of Heart Wall Epicardium (a.k.a. visceral pericardium) Myocardium Endocardium Figure 12.4 Cardiac Muscle Tissue Because of the characteristics of cardiac muscle tissue & the arrangement of connective tissue (fibrous skeleton) within the heart, the heart basically has two functional units: the myocardium of the atria (upper chambers) act as one functional unit the myocardium of the ventricles (lower chambers) act as the other This allows the atria to contract simultaneously while the ventricles are relaxed; then the ventricles contract simultaneously while the atria relax External Features Auricles Coronary sulcus – contains the coronary sinus Anterior interventricular sulcus – contains coronary vessels Posterior interventricular sulcus – contains coronary vessels SVC Interatrial septum Pulmonary veins Lt Atrium Rt Atrium Pectinate muscles Bicuspid (mitral) valve Coronary sinus (opening) Chordae tendineae Tricuspid valve Papillary muscle Chordae tendineae Papillary muscle IVC Deoxygenated blood Oxygenated blood Atrioventricular (AV) valves Tricuspid Bicuspid Lt. common carotid artery Brachiocephalic trunk Lt. subclavian artery Aorta Ligamentum arteriosum Pulmonary artery Pulmonary trunk Pulmonary semilunar valve Aortic semilunar valve Trabeculae carneae Lt ventricle Rt ventricle Interventricular septum Anatomy Coronary Circulation Myocardium receives oxygenated blood from the left & right Coronary arteries – branches off the ascending aorta Deoxygenated blood is drained through Cardiac veins, which all eventually merge into the coronary sinus Fig. 12.7 Conducting System Intrinsic regulating system that generates “heartbeat” comprised of functionally specialized “autorhythmic (conducting) cells” – which can spontaneously generate action potentials Fig. 12.9 The electrical events that occur in the heart can be detected on the surface of the body The resulting pattern of activity is known as an ECG (or EKG) Electrocardiogram (ventricular repolarization) Electrocardiogram (ECG) (atrial depolarization) (ventricular depolarization) The activity of the conduction system results in the contraction (systole) & relaxation (diastole) of the heart chambers The change in volume (size) of the chambers results in changes in pressure within the heart – decreased volume increased pressure & vice-versa. Blood will flow through the chambers (and throughout the cardiovascular system) due to the differences in pressure (blood moves from high low pressure) Cardiac Cycle One complete “heartbeat” is referred to as a “Cardiac Cycle” Average 75 cycles/minute Each cycle lasts approx. 0.8 seconds Continuous, repetitive cycle that can be “divided” into 3 phases for ease of understanding: atrial diastole/ventricular diastole (0.4 sec.) atrial systole/ventricular diastole (0.1 sec.) atrial diastole/ventricular systole (0.3 sec.) Cardiac Cycle atrial systole/ventricular diastole atrial diastole/ ventricular diastole “Lub” “dupp” atrial diastole/ventricular systole Cardiac Output Important physiological measurement of cardiac function Refers to the amount of blood ejected by the left ventricle each minute C.O. = stroke volume X heart rate stroke volume – amount of blood ejected from ventricle each contraction (80 ml average) heart rate – beats (cardiac cycles) per minute (75 bpm average) average C.O. = 6000 ml/min (6 L/min) Cardiac Output Cardiac output is primarily regulated by: 1. Blood volume reflexes – there is a direct relationship between blood entering the heart & amount ejected increased venous return atrial reflex (aka Bainbridge reflex) increased heart rate (through increase in sympathetic activity) increased venous return ventricular reflex (aka Frank-Starling principle) increased stroke volume Cardiac Output 2. Cardiac center of M.O. – ANS input to SA node to increase/decrease heart rate & stroke volume Cardiac center influenced by: baroreceptors – detect blood pressure changes chemoreceptors – detect oxygen/carbon dioxide concentrations higher brain centers – ie. hypothalamus 3. Hormones – epinephrine/norepinephrine, thyroid hormones, glucagon, etc can increase heart rate & force of contraction