Unit 8: Infection Control
advertisement

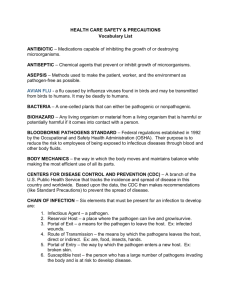
Infection Control: Efforts designed to protect both the patient and care provider. Infectious Disease: Any illness resulting from invasion of a host by disease producing organisms such as bacteria, viruses, fungi, or parasites. Also known as: microbes Small living plant/animal not visible to naked eye Found everywhere in the environment, including in/on human body Many microbes exist on or within us and do not cause disease or infection (are called non-pathogens) Microbes that cause infection/disease are called pathogens Some microbes can be beneficial (Normal Flora)in one body system & become pathogenic in another (ex. E-coli- normal in large intestine, causes UTI in urinary) 5 types: Bacteria Protozoa Fungi Rickettsiae Viruses Simple one-celled organism that can produce disease in a host, can multiply outside of cells on surfaces or objects. Classified by shape and arrangement Bacterium protected by a hard shell is called a spore 3 main types: cocci, bacilli, spirilla Round/spherical in shape 3 types: Diplococci-occur in pairs or 2 circles, causes gonorrhea, meningitis, & pneumonia 2. Streptococci-occur in chains, causes strep throat 3. Staphylococci-occur in clusters/groups, causes boils, wound infections & toxic shock, UTI’S 1. Strep bacteria Staphylococcus aureus (wound) Rod shaped Occur singly, in pairs, or in chains Many have flagella(threadlike projections like tails that allow them to move) Ability to form spores or thick walled capsules(extremely difficult to kill while in spore form) Can cause TB, tetanus, whooping cough, botulism Anthrax with white blood cells Spiral or corkscrew in shape Include corkscrew spirochete Can cause syphilis and cholera One celled animals Found in decaying materials & contaminated water Some are pathogenic & cause malaria, amebic dysentery, Pneumocystis Carini Pneumonia (PCP), Trichomonas Plasmodium: Malaria Simple plantlike organisms Live on dead organic matter Yeasts & molds are common forms of pathogenic fungi Can cause ringworm, athlete’s feet, & histoplasmosis (systemic respiratory infection) Parasitic microbe: 1. Cannot live outside the cells of another living organism 2. Commonly found on fleas, ticks, & mites 3. Transmitted to humans by bites of these insects 4. Can cause typhus fever & Rocky Mountain spotted fever Rocky Mountain Spotted Fever Smallest microbe-only visible with electron microscope Cannot reproduce unless they are inside another living cell Spread mainly from human to human by blood & body secretions Very difficult to kill-resist most disinfectants, not affected by antibiotics Can cause common cold, flu, pneumonia, measles, chickenpox, herpes, warts, hepatitis B, HIV Hepatitis B virus Warm environment Darkness-most are killed quickly in sunlight Source of food & moisture Need for oxygen varies- aerobic(need O2 to live) anaerobic(don’t need O2) Human body is ideal supplier of all of these requirements 1. Some produce poisons (toxins) which harm the body 2. Some cause an allergic reaction resulting in watery eyes, runny nose & sneezing 3. Others attack & destroy the living cell they invade ( ex. Malaria invades RBC & causes it to rupture, HIV invades T-cells) Factors that must exist for disease to occur. Includes: 1. Causative agent 2. Reservoir 3. Portal of exit 4. Means of transmission 5. Portal of entry 6. Susceptible host Chain of Infection Causative Agent / Pathogen Host Reservoir Portal of Entry Transmission Portal of Exit 1. Causative agent- pathogen such as bacteria or virus 2. Reservoir place- where causative agent lives. Common reservoirs include human body, animals, environment, and fomites ( objects contaminated with infectious material that contains the pathogens, i.e. pencil, desk, hand rail, etc.) A Human being or animal that is a reservoir for microorganisms but is not ill with infection/disease is a carrier or host. (Example: HIV) 3. Portal of exit- way for causative agent to escape from the reservoir. Pathogens can leave the body through urine, feces, saliva, blood, tears, mucous discharge, sexual secretions & draining wounds Means of transmission- pathogen must be transmitted to another reservoir or host where it can live. Five main routes of transmission: 1. Contact- direct/indirect 2. Droplet- propelled short distances through air (flu) 3. Airborne- remain suspended in air for long periods of time ( TB, measles, chicken pox) 4. Five main routes of transmission: 4. 5. Vectorborne – Insect bite (fleas/ticks) Common Vehicle – pathogen transmitted through items such as surgical instruments, stethoscopes, blood pressure equipment, etc. Contact: According to the CDC, this is the most frequent method of disease transmission in a hospital environment. Direct- direct contact transmission from one person to another through physical contact. Indirect- transmission from one person to another through an object such as contaminated hands or medical instruments (needle stick, dressings, patient care items). Patients under contact precautions should be placed in a private room or in a room with another patient who has the same infection. If this is not possible, patient placement will depend on the type of infection and an infection control expert should be consulted. Gloves should be worn Change gloves after handling potentially infective material Dispose of gloves before leaving room. NEVER wear gloves in hallways or outside patient’s room A non-sterile gown should be worn when entering the patient's room if clothing may be contaminated. Remove before leaving patients room Avoid touching contaminated areas with uniform/hands Patient movement should be limited, but if it is necessary, care should be taken not to contaminate other patients and surfaces. Whenever possible, patient care equipment should be dedicated to a single patient or group of patients with the same infection. If this is not possible, the equipment must be carefully disinfected after each use. Droplet transmission - Occurs when an infected patient expels droplets into the air and the droplets land in the nasal cavity, mouth, or conjunctiva. The droplets are generated from coughing, sneezing, talking, and by some medical procedures. When you sneeze, millions of tiny droplets are propelled from your mouth and nose. The droplets fly through the air rather than remaining suspended in the air. Measles, mumps, rubella, and Severe Acute Respiratory Syndrome (SARS) can all be transmitted through droplet transmission. Almost all common diseases may be spread through droplet transmission. Placed in a private room Or room with patient who has the same infection. Three foot separation between the infected patient and other people It is not necessary to keep the door closed. Health care personnel should wear a mask and goggles The patient should wear a mask if moved Airborne transmission - when tiny particles containing pathogens remain suspended in the air for long periods of time. Examples: Measles and chickenpox One of the worst outbreaks of disease in human history was the influenza pandemic of 1918. Historians believe it began in America. At least 21 million people died, and possibly as many as 50 million. Many of them drowned to death when fluid from the infection filled their lungs. Some airborne pathogens can be spread in the wind, and affect huge areas. Placed in a private room or, if necessary, OR: In a shared room with another patient who has an active infection of the same type. Door should be kept closed Air circulation system must prevent spread of unfiltered air to other areas Negative Air Pressure System Patient movement around the facility should be minimized. If the patient must be moved, he or she should wear an N95 mask. Everyone entering the room should wear a N95 respirator. Examples: pulmonary tuberculosis, chickenpox, A vector - organism that carries pathogens from one host to another. Examples: fleas, ticks, and rats. Malaria, yellow fever, and bubonic plague are all diseases that can be spread through vectors. This type of transmission occurs when pathogens are spread to several hosts through a single contaminated item such as food, water, or surgical instruments. Example E. coli spread through food. 5. Portal of entry- way to enter a new reservoir or host Different portals of entry: Breaks in the skin or mucous membrane Respiratory tract Digestive tract Genitourinary tract Circulatory system 6. Susceptible host- individual who can contract the disease Most susceptible- elderly, newborns, persons with weak immune systems, persons with cancer Humans become host when large numbers of pathogens invade the body and body defenses are weak If any part of the chain can be eliminated, the spread of disease/infection will be stopped Follow practices to interrupt or break this chain (wash your hands) Asepsis- absence of disease producing microbes or pathogens Common aseptic techniques: handwashing & good personal hygiene, using disposable gloves when contacting contaminated objects, proper cleaning of instruments & equipment Handwashing: the single most effective way to prevent the spread of pathogens 1. Antisepsis - prevent/inhibit the growth of pathogenic organisms. Usually not effective against spores & viruses Can be used on the skin Example; Alcohol & betadine 2. Disinfection - process that destroys or kills pathogenic organisms Used mainly on objects not people Not always effective against spores & viruses Can irritate and damage the skin, Example; Bleach solutions 3. Sterilization - process that destroys all microorganisms both pathogenic and nonpathogenic. Kills spores & viruses Steam under pressure, gas, radiation, and chemicals can be used to sterilize objects Autoclave is the most common piece of equipment used for sterilization CDC (Center for Disease Control) has identified 2 levels for infection control. Standard Precautions Transmission-Based Precautions Goal: Keep pathogens within a specific area Standard precautions: treat all patients as though they may be infected. Standard precautions combine the major features of : 1. Universal Precautions - reduces the risk of transmitting bloodborne pathogens 2. Body-Substance Isolation (BSI)reduces the risk of transmitting pathogens from moist body substances Wash hands: Before/after examining patients After contact with blood, body fluids & contaminated items. Wear gloves: if there could be contact with blood, body fluids, mucous membrane, or broken skin. Remove gloves: Before going to another patient, wash hands and put on new gloves. Wear a mask protective eyewear and gown: when splashes or sprays of body fluids are likely. Do not recap needles. EVER! Clean and disinfect frequently touched surfaces including beds, bed rails, patient examination tables and bedside tables Launder soiled linens and avoid direct contact with soiled items Use oral rather than injectable medications whenever possible Universal Precautions - introduced in 1985 as a response to the appearance of AIDS. Treat all materials as though they are infected with diseases such as HIV or HBV. Use gloves and gowns, masks and eye protection during medical procedures. Standard precautions include: 1. Protective work practices - 2. 3. 4. 5. handwashing, handling sharps, good hygiene Use of personal protective equipment (PPE) - gloves, gowns, face shields, masks Protective housekeeping (disinfectants) Protection: Hepatitis B vaccination Exposure reporting Transmission-Based Precautions are used in addition to standard precautions. Categories include airborne, droplet, contact Place patient in private room Keep their door closed Wear masks & gloves to enter the room, Move patient only for essential purposes Have patient wear mask outside of the room