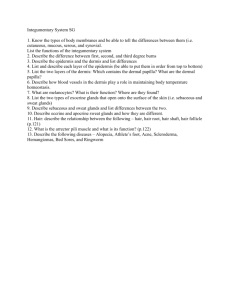
Ch. 5 AP PP
advertisement

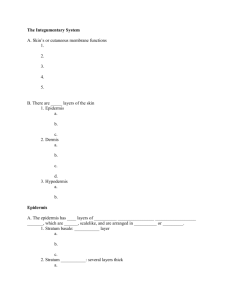
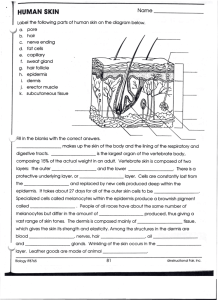
INTEGUMENTARY SYSTEM INTRODUCTION The integumentary system is made up of the skin, hair, nails, and various glands - when something goes wrong with your skin, it is apparent right away - physicians pay attention to the skin because any changes could be signs of a disorder or problem with another body system STRUCTURE AND FUNCTION The integument has 2 major components: 1. CUTANEOUS MEMBRANE- or skin; an organ composed of the EPIDERMIS (superficial epithelium) and underlying connective tissues of the DERMIS 2. ACCESSORY STRUCTURES- include hair, nails, and a variety of exocrine glands - below the dermis is the SUBCUTANEOUS LAYER, which attaches integument to deeper structures (muscle and bone) There are 5 major functions of the integument: 1. Protection- skin protects underlying tissue and organs from impact, chemicals, infection; prevents loss of body fluids 2. Temperature maintenance- skin regulates heat gain or loss to environment 3. Making and storing of nutrients- epidermis makes vitamin D, which aids in uptake of calcium; dermis contains large amounts of lipids (fats) in adipose tissue 4. Sensory reception- receptors detect pain, pressure, and temperature stimuli and relay that info. to the nervous system 5. Excretion and secretion- excretes salts, water, organic wastes; produces milk EPIDERMIS The EPIDERMIS consists of stratified squamous epithelium - WHAT DOES STRATIFIED MEAN? - in THICK SKIN (palms of hands and soles of feet) there are 5 layers - in THIN SKIN (covers rest of body) there are only 4 layers STRATA OF EPIDERMIS STRATA IS ANOTHER NAME FOR LAYERS In order from the basement membrane toward the surface are: Stratum germinativum Intermediate strata (3 layers) Stratum corneum STRATUM GERMINATIVUM - deepest epidermal layer - attached to basement membrane by a type of desmosome - basement membrane separates the epidermis from the dermis - this layer forms EPIDERMAL RIDGES which extend into the dermis, increasing area of contact between the 2 regions - contours of the skin follow these ridge patterns - these ridges in the palms and soles increase surface area of the skin, and help ensure grip Ridge patterns are GENETICALLY DETERMINED, and do not change over a lifetime FINGERPRINTS! You also find large stem cells (germinative cells) in the stratum germinativum, so this is the layer where new cells are generated and begin to grow - these cells replace those lost or shed at the surface - also contains MELANOCYTES- receptors provide info. about objects touching the skin; make MELANIN- a pigment that colors the epidermis INTERMEDIATE STRATA - made up of 3 layers; each becoming specialized to form outer protective covering of skin - find the protein KERATIN here: * extremely durable and water-resistant * coats the surface of the skin, forms basic structure of hair, calluses, and nails STRATUM CORNEUM - outermost layer - consists of 15-30 layers of flattened, dead epithelial cells that have large amounts of keratin these cells are said to be KERATINIZED - dead cells in each layer are tightly connected by desmosomes are usually shed in sheets rather than individually TIMELINE It takes about 2-4 weeks for a cell to move from the stratum germinativum to the stratum corneum - cell is removed from its oxygen and nutrient supply, is filled with keratin, and finally dies - dead cells usually remain in the stratum corneum for about 2 weeks before they are shed - as these layers are lost, they are replaced from below SKIN COLOR Skin color is caused by interaction between: 1. epidermal pigments 2. dermal blood supply PIGMENTATION The epidermis has varying amounts of the two pigments CAROTENE and MELANIN CAROTENE- orange-yellow pigment that normally accumulates in dermal cells - these pigments are found in vegetables such as carrots (eating a large amount of carrots can turn your skin orange!) - can be converted to vitamin A which is required for normal maintenance of epithelial tissue MELANIN- brown, yellow-brown, or black pigment produced by melanocytes - melanocytes make and store melanin and inject it into the epithelial cells of the stratum germinativum and intermediate strata - this colors the entire epidermis Melanocyte activity increases after sunlight exposure FRECKLES- represent areas of larger-thanaverage melanin production - most abundant on surfaces exposed to sun ULTRAVIOLET (UV) RADIATION A small amount of UV radiation is beneficial because it stimulates the making of vitamin D3 - too much UV radiation produces burns - melanin helps to prevent skin damage by absorbing UV radiation before it can reach the deep layers of the integument - despite this protection, long-term damage can result, even in individuals with dark skin EFFECTS OF UV EXPOSURE: - alterations in underlying connective tissue can cause premature wrinkling - skin cancers can result from chromosomal damage to stem cells * one major consequence of depletion of the ozone layer has been an increase in rates of skin cancer * WEAR SPF OF AT LEAST 15; HIGHER FOR BLONDES AND REDHEADS DIFFERENCES IN SKIN COLOR Differences in skin color between individuals is not due to the number of melanocytes, but to the different levels of melanin production - in the inherited condition albinism melanin is not produced by melanocytes DERMAL CIRCULATION - Blood having a lot of oxygen is bright red, and blood vessels in the dermis give the skin a reddish tint that is most obvious in lightskinned individuals - when vessels are dilated (during inflammation), red tones become more pronounced - when vessels are constricted (frightened), skin becomes pale - during a prolonged reduction in circulation, blood loses oxygen and becomes dark red, then blue CYANOSIS VITAMIN D3 Limited exposure to the sun is beneficial: - epidermal cells in stratum germinativum and intermediate strata convert a steroid into VITAMIN D3 - this is modified and converted into a hormone called CALCITRIOL which is essential for the absorption of calcium and phosphorus by the small intestine - deficiency of vitamin D3 causes abnormal bone growth SKIN CANCER BASAL CELL CARCINOMA- malignant cancer that originates in the stratum germinativum - most common type SQUAMOUS CELL CARCINOMAS- less common - metastasis seldom occurs in either; survival is good MELANOMAS- seldom-occurring and lifethreatening - usually begin from moles, but may appear anywhere in the body - can grow rapidly and metastasize through the lymphatic system - survival depends on when condition is detected and treated - AVOIDING UV RADIATION CAN PREVENT ALL 3 TYPES OF CANCER The Dermis The Dermis The dermis lies below the epidermis and has 2 main components: Papillary layer Reticular layer PAPILLARY LAYER - consists of loose connective tissue that supports and nourishes the epidermis - contains capillaries and nerves supplying the surface of the skin RETICULAR LAYER - deeper layer - consists of interwoven meshwork of dense, irregular connective tissue - boundary between reticular and papillary layers is indistinct - collagen fibers of reticular layer extend into the subcutaneous layer - reticular layer provides support and attachment for dermis while allowing flexibility OTHER DERMAL COMPONENTS The dermis contains all of the cells found in connective tissue proper (macrophages, fibroblasts, etc) - accessory organs such as hair follicles and sweat glands extend into the dermis - other systems communicate with the skin through the dermis Ex: reticular and papillary layers contain blood vessels, lymph vessels, and nerve fibers - blood vessels provide nutrients and oxygen, and remove CO2 and wastes - blood and lymph vessels help local tissues defend and repair themselves after injury or infection - nerve fibers control blood flow, adjust gland secretion rates, and monitor nerve receptors The Subcutaneous Layer Subcutaneous Fat The dermis is connected to the subcutaneous layer by an extensive network of connective tissue fibers - the subcutaneous layer is not actually part of the integument, but is important in stabilizing position of the skin in relation to underlying tissue - this layer contains many fat cells (adipose) - these adipose cells provide infants and small children with a layer of “baby fat” which reduces heat loss, and acts as a shock absorber to prevent injury - as we age, we accumulate this fat in different places: * Men- around neck, upper arms, lower back, buttocks * Women- breasts, buttocks, hips, thighs * Both accumulate in abdominal area - the subcutaneous layer is very elastic, has large blood vessels, and contains no vital organs Accessory Structures HAIR FOLLICLES Hair covers the body almost everywhere EXCEPT: Sides and soles of feet Palms Sides of fingers and toes Lips STRUCTURE OF HAIR - hair follicles project into the dermis and often into the subcutaneous layer - walls of each follicle contain all the cell layers found in epidermis - the epithelium at the base of a follicle surrounds the HAIR PAPILLA- a peg of connective tissue containing capillaries and nerves - hair is formed by the repeated divisions of epithelial stem cells surrounding the papilla - as daughter cells are pushed to the surface, the hair lengthens and the cells become keratinized and die - the point at which this occurs marks the boundary of the HAIR ROOT and HAIR SHAFT - hairs grow and are shed according to a HAIR GROWTH CYCLE based on the activity of hair follicles - generally, a hair in the scalp grows from 2 to 5 years at a rate of about 0.3 mm per day, and then its follicle may become inactive for some time - when another growth cycle begins, the old hair is pushed toward the surface to be shed - differences in hair length between individuals depends on variations in growth rate and in the length of the hair growth cycle - other differences in hair appearance result from size of follicles and shape of hairs FUNCTIONS OF HAIR - there are approximately 5 million hairs on the human body - the 100,000 hairs on the head protect the scalp from UV light, cushion a light blow to the head, and insulate the skull - hairs guarding the entrance to the nostrils and ears, as well as the eyelashes, defend against entry of foreign particles and insects - each hair follicle as a sensory nerve associated with it you can feel a single hair move : early warning system - smooth muscles called ARRECTOR PILI MUSCLES are connected to the hair follicle - when stimulated, they pull on follicle and cause hair to stand up- “goose bumps” HAIR COLOR - hair color depends on differences in type and amount of pigment produced by melanocytes in the papilla - color is genetically determined - color may also be influenced by hormonal or environmental changes Ex: pigment production decreases with age, and color of hair lightens - white hair results from lack of pigment, and the presence of air bubbles in the hair shaft - as number of white hairs increases, individual’s color is described as GRAY - on average, about 50 hairs are lost from the head per day SEBACEOUS GLANDS Sebaceous glands are a type of exocrine gland that discharge a waxy secretion into hair follicles and onto the skin - contraction of arrector pili muscles squeezes the sebaceous glands, forcing the secretions into the hair follicles and onto the surrounding skin - the secretion is called SEBUM- it lubricates the hair and inhibits growth of bacteria Sebaceous glands are very sensitive to changes in concentrations of sex hormones - secretions increase at puberty - an individual with large sebaceous glands may be prone to ACNE - in acne, sebaceous glands become blocked and secretions accumulate causing pimples to form SWEAT GLANDS The skin contains 2 types of sweat glands: Apocrine sweat glands Merocrine sweat glands APOCRINE GLANDS - secrete their products into hair follicles in the armpits, around the nipples, and in the groin - at puberty, these glands begin discharging a sticky, cloudy secretion that becomes odorous when broken down by bacteria - antiperspirant works by contracting the sweat gland openings and decreasing the quantity of secretions MEROCRINE GLANDS - far more numerous than apocrine glands - the skin of an adult contains 2-5 million merocrine glands - palms and soles have the highest number - merocrine glands are coiled tubular glands that discharge their secretions directly onto the surface of the skin - secretions are called PERSPIRATION- cool the surface of the skin and reduce body temperature When a person sweats in the hot sun, all merocrine glands are working together: - blood vessels beneath the epidermis are flushed with blood- skin becomes red - skin surface is warm and wet, and as the moisture evaporates, the skin cools - if body temperature falls too low, perspiration stops, blood flow to the skin decreases, and the cool, dry surfaces release little heat to the environment SWEAT IS 99% WATER - but also contains salts, organic nutrients, and waste products such as urea - is what gives sweat a salty taste - when all merocrine glands are working together, perspiration can exceed 1 gallon per hour - you must drink fluids to replenish this loss OTHER TYPES OF SWEAT GLANDS: - mammary glands produce milk - ceruminous glands in the ear produce ear wax NAILS Nails form on dorsal surface of fingers and toes, and protect the exposed tips and help limit their distortion when they are subjected to mechanical stress STRUCTURE - visible NAIL BODY made up of a mass of dead, keratinized cells - it extends below the surrounding epithelium - nail body covers an area of epidermis called the NAIL BED - nail production occurs at the NAIL ROOT- an epithelial fold that you cannot see from the surface - a portion of the stratum corneum extends over the exposed nail nearest the root, forming the CUTICLE - underlying blood vessels give nails their pink color - - vessels may be obscured near the root, leaving a pale crescent known as the LUNULA nail structure CONTROL OF HOMEOSTASIS The integumentary system can respond directly and indirectly to many local influences or stimuli Ex: when skin is subjected to mechanical stresses, stem cells in the stratum germinativum divide more rapidly to increase the thickness of the epithelium CALLUSES FORM INJURY AND REPAIR Skin can regenerate because stem cells are present in epithelial and connective tissue components - speed and effectiveness of skin repair depends on the type of wound * an INCISION (slender, straight cut) may heal quickly * an ABRASION (scrape) may take longer to heal because it involves a greater area 4 STAGES OF SKIN REGENERATION 1. When damage extends though epidermis and into the dermis, bleeding occurs 2. Blood clot or SCAB that forms temporarily restricts the entry of additional microorganisms - clot is made up of protein called FIBRIN - cells of stratum germinativum rapidly divide and migrate along sides of the wound to replace missing epidermal cells - phagocytes patrol damaged area and clear away debris and pathogens 3. Dermal repairs must occur before epithelial cells can cover the surface - fibroblasts and connective tissue stem cells divide to produce mobile cells that invade deeper areas of injury - capillaries follow the fibroblasts, providing a circulatory supply - combination of blood clots, fibroblasts, and capillary network is called GRANULATION TISSUE - over time, the clot dissolves and number of capillaries decreases - fibroblast activity leads to formation of collagen fibers and ground substance 4. Scar tissue is formed - dermis will contain many collagen fibers and few blood vessels - damaged hair follicles, glands, muscle cells, and nerves are seldom repaired BURNS Burns result from exposure of skin to heat, radiation, electrical shock, or strong chemical agents - severity reflects depth of penetration and total area affected FIRST-DEGREE BURN - superficial cells of epithelium are killed - deeper areas of the epidermis and papillary dermis are injured - area appears inflamed and is tender SECOND-DEGREE BURN - superficial and deeper cells of epidermis are killed; dermis may be affected - reticular layer of epidermis may be injured, but most accessory structures are unaffected - blisters are present; very painful THIRD-DEGREE BURN - all epidermal and dermal cells are killed - subcutaneous layer and deeper tissues and organs are injured - skin is charred; individual has no sensation at all AGING SOME CHANGES THAT OCCUR WITH AGING: 1. Skin injuries and infections become more common- epidermis thins 2. Sensitivity of immune system reducedimmune cells are decreasing in number 3. Muscles become weaker, bone strength decreases- decline in vitamin D3 production 4. Sensitivity to sun exposure increases- less melanin produced 5. Skin becomes dry and scaly- sebum and perspiration production decreases 6. Hair thins and color changes- follicles stop functioning; again decreased melanin production 7. Sagging and wrinkling of skin- dermis becomes thinner and elastic fiber network decreases 8. Ability to lose heat decreases- blood supply to dermis is reduced; sweat glands become less active - more prone to overheating 9. Skin repairs slowly