Document
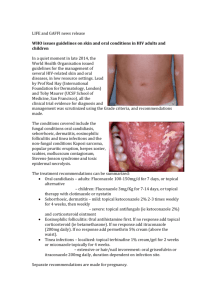
advertisement

Dermatotherapeutics - Topical Digital Lecture Series : Chapter 30 Dr. Pallavi Utekar-Telavane Assistant Professor, Department of Dermatology, Rajiv Gandhi Medical College and Chatrapati Shivaji Maharaj Hospital, Thane CONTENTS Introduction Cytotoxic and Immunomodulatory Drug delivery Keratolytic agents Patient information Moisturizers Steroids Sunscreen Anti acne Depigmenting agents Anti-bacterial Anaesthetic Anti-fungal Miscellaneous Anti-viral MCQs Anti-parasitic Photo Quiz Calcineurin inhibitors Introduction Topical therapy implies delivery of medicines at the site of the lesion It’s a mainstay of treatment in most dermatological disorders. While prescribing topical agent to the patient a physician must consider the product itself , the disease to be treated and the patient. Advantages and disadvantages of Topical Therapy Advantages Disadvantages Reduced systemic side effects Requires lots of counselling Accessibility & visibility of the therapy on skin Expected results might not be achieved due to lack of compliance Few medicines which cant be used systemically can be used topically e.g. salicylic acid Allergic reactions can be noted not because of drug but because of vehicle as well Penetration of molecule is affected by multiple factors which can affect the desired results Factors affecting drug delivery Age of patient: Absorption is more in neonates and children as compared to adults Traumatised or diseased skin allows easier penetration Site of application : Absorption is better in the following sites in descending order : mucous membrane, scrotum, eyelids, face, chest & back, upper arms & thighs, lower arms & legs, dorsa of hands & feet, palmar & plantar skin followed by nails. Potency : Higher the concentration of the drug in the topical formulation better is the absorption and therapeutic effect. Vehicle used : Ointments have better penetration than creams, lotions, gels or pastes Factors affecting drug delivery Occlusion : increases hydration and temperature of stratum corneum, thus increasing penetration of the drug. Hydration: Simple immersion in water for 5 min prior to application of topical agent increases absorption. Frequency of application : doesn’t significantly increases effectiveness of molecule except that for emollients. Quantity of drug applied has negligible effect on absorption. Massaging: vigorous rubbing or massaging increases the penetration. Presence of hair follicles : enhances drug penetration. Vehicle Vehicle is the substance which brings the topical medication in contact with the skin. Types of vehicles : Liquids : Solutions , Lotions, Liniments, Suspensions Semisolids : Creams, ointments, Pastes, Gels Solids : Powders Liquids Solutions : Wet dressings : These are of 2 types Open and Closed dressings. Solutions of choice are Normal saline, burrow’s solution, Condy’s compresses etc. Bath : method used when a part or all of the body has to be treated e.g. 8-MOP bath. Tinctures and Paints : these are liquid preparations which are applied over skin or mucous membrane with a brush and left to evaporate. Liquids Lotions : These are liquid or semisolid preparations and consist of solutions of drug in water, alcohol or other liquids. On evaporation drug is deposited on skin surface. Liniments : These are non aqueous solutions of drugs in oil or alcoholic solutions of soap. Poultices : These are wet solid masses of particles, sometimes heated, that are applied to diseased skin. These are used as cleansers and absorptive agents in chronic exudative lesions such as leg ulcers. Semisolids Creams : These are semisolid emulsions containing two immiscible liquids (suspension of water and oil). There are of 2 types: Oil in water type (O/W) Water in oil (W/O) Ointments : These are semi-solid, soft to firm, greasy preparations that carry active ingredients in concentration of up to 40%. They are occlusive and act as emollients. Semisolids Pastes : These are semisolid preparations of finely powdered material in a greasy base, in approximately 1: 1 ratio. Pastes protect the skin from mechanical forces, absorb moisture and aid drying of oozing and weeping lesions. Gels : Gels are soft, semisolid preparations, translucent to transparent in appearance, that liquefy on contact with the skin and dry as thin, greaseless films. Solids Powders : Powders are solid preparations used to promote drying or reduce friction. Newer Drug Delivery System Nanotechnology : • Solid or liquid lipid nanoparticles act as carriers. • Drugs are entrapped within lipid core matrix. • It improves cutaneous bioavailability as it has ability to penetrate follicles. Microemulsions : • This is a thermodynamically stable mixture of oil and water stabilized by surfactants. • Can solubilize many poorly soluble drugs. Newer Drug Delivery System Liposomes : • These are vesicles which consist of one or more concentric lipid bilayers separated by aqueous buffer compartment. • These either get adsorbed over skin and release the drugs or penetrate via lipid rich channels. Microsponges : • These have porous beads which encloses the active drug. • Cosmetically better acceptance. Instruction provided to patients Frequency of application. Timing of application. Quantity for every application. Common side effects seen with the medication. Total duration of use. Not to self-treat. Quantity of application It is described in terms of Finger Tip Unit and Hand areas. Finger Tip Unit (FTU) : If a cream or ointment is squeezed out of a tube which has a nozzle of 5mm, over the distal section of an index finger from distal skin crease to tip of finger, the amount is roughly equal to 0.5g. Quantity of application Site for an adult Quantity in FTU No. of Hand Areas Face and Neck 2.5 5 Front and Back of Trunk 14 28 One arm 4 8 One hand 1 2 One leg 8 16 One foot 2 4 Topical Steroids Mechanism of Action It acts by binding to specific DNA sequence i.e. Glucocorticoid responsive elements (GRES) and transcription of specific mRNA. Anti-inflammatory Immunosuppressive Anti-proliferative Vasoconstriction Potency ranking of topical corticosteroids Class 1 (Super potent) Halobetasone Propionate (0.05%) Clobetasol propionate (0.05%) Class 2 (Potent) Mometasone Furoate oint (0.1%) Betamethasone dipropionate (0.05%) Class 3 (Potent) Fluticasone Propionate (0.005%) oint Class 4 (Mid-strength) Mometasone Furoate cream (0.1%) Triamcinolone Acetonide oint (0.1%) Potency ranking of topical corticosteroids Class 5 (Mid strength) Fluticasone Propionate cream (0.05%) Hydrocortisone Butyrate (0.1%) Class 6 (Mild) Desonide (0.05%) Fluocinolone Acetonide cream (0.01%) Class 7 (Least potent) Dexamethasone cream (0.1%) Hydrocortisone (0.5%,1%, 2.5%) Intralesional corticosteroids When topical applications are ineffective, few preparations can be directly injected into the skin lesion. Preferred agent : Triamcinolone acetonide. Properties : Long acting, small particle size, stable at room temperature, Easy resuspension by shaking, lesser effects on pituitary- adrenal axis. Indications : Nodulocystic acne, keloid, hypertrophic scar, prurigo nodularis, etc. Nodulocystic Acne Indication Eczematous disorders Papulosquomous disorders – Psoriasis, Lichen planus, etc. Bullous dermatoses Connective tissue Neutrophilic dermatoses Alopecia Insect bite reaction Photodermatoses Pigmentary disorders – Vitiligo and many more… Contraindications : Absolute – h/o hypersensitivity to tropical corticosteroid. Relative – Local untreated bact, fungal, viral, mycobact infection, infestatation, ulceration. Chronic Eczema Psoriasis Alopecia Areata Lichen Planus Side effects of Topical Steroids Striae Contact dermatitis Telangiectasia Tachyphylaxis Stellate pseudoscars Facial hypertrichosis Hypopigmentation Folliculitis Fragile skin, purpura Miliaria Impaired wound healing Increased susceptibility to bacterial fungal and viral inf. Steroid dependency Perioral Dermatitis Glaucoma and cataract Rosacea Atrophy Topical Steroid induced hypopigmentation Topical steroid induced hypopigmentation and telangiectasia Topical steroid induced telangiectasia Topical steroid induced perioral dermatitis Intralesional steroid induced atrophy Topical steroid induced atrophy Tinea Incognito with striae Acneiform Eruption Acneiform Eruption with Hypertrichosis Systemic side-effects of topical steroids Suppression of hypothalamic – pituitary – adrenal axis Cushing’s syndrome Hyperglycemia Intracranial hypertension Growth retardation in children Reduced bone mineral density Oedema Hypocalcemia Hypertension Anti acne medicines Class Mechanism of Action Retinoids : Block inflammatory Tretinoin cream cascade (0.025%- 0.05%) Decrease Adapalene gel (0.1%) hyperproliferation in the follicles Stimulate dermal collagen production Benzoyl peroxide Oxidising agent so direct toxic action on P. Acne Lipophilic so penetrates sebaceous follicles better No resistance has been noted Side Effects Causes irritation Are photo irritants Irritation, erythema, scaling, burning, dryness,stinging Contact dermatitis Anti acne medicines Class Mechanism of Action Side Effects Topical antibiotics Erythromycin (2%) Clindamycin (1%) Clarithromycin (1%) Azithromycin (2%) Nadifloxacin Dapsone (5%) Metronidazole gel Reduce population of P. Acne Few have antiinflammatory action Should not be used continuously for 3 months for the fear of resistance Azelaic Acid 10%-20% Antibacterial Anti-keratinizing effect Inhibit tyrosinase enzyme Irritation Nicotinamide gel 4% Anti-inflammatory Not specific Anti acne medicines Class Mechanism of Action Side Effects Salicylic Acid Keratolytic Inhibits comedogenesis Promote follicular desquamation Lipid soluble so penetrate sebum laden follicles better Irritation, erythema Ivermectin gel ( used in rosacea) Anti parasitic action on Demodex folliculorum Grade 2 Acne Antibiotics Name Bacterial coverage Mechanism of action Bacitracin Bactericidal against Gram (+) and Neisseria species Interferes with bacterial wall synthesis; inhibition of phospholipid receptors involved in peptidoglycan synthesis Polymyxin B Bactericidal against Gram (-) Increases permeability of bacteria only; effective bacterial cell membrane; by against P. aeruginosa interacting with phospholipid components of membrane Neomycin Bactericidal against Gram (+) Inhibits protein synthesis; and Gram (-) bacteria; good binding to 30s subunit of S. aureus coverage ribosomal RNA Antibiotics Name Bacterial coverage Mechanism of action Metronidaz Anaerobic bacteria, ole (0.75parasites 1%) Forming free radicals that damages DNA ; Immunomodulatory Sodium fusidate (fusidic acid) 2% Interfere with bacterial protein synthesis by preventing translocation of elongation factor G from ribosome Anti staphylococcal Impetigo Contagiosa Antibiotics Name Bacterial coverage Mechanism of action Mupirocin Bactericidal against methicillin-resistant S. aureus; S. pyogenes Inhibits bacterial RNA and protein synthesis; occurs by reversibly binding to bacterial isoleucyl transfer RNA synthetase Retapamulin Bacteriostatic against S. pyogenes, mupirocin-resistant and methicillin-resistant S. aureus, anaerobes Inhibits bacterial protein synthesis; occurs by binding to protein L3 on 50s ribosomal subunits Antibiotics Name Bacterial coverage Mechanism of action Gentamicin Bactericidal against Gram (+) Inhibits bacterial protein and Gram (-) organisms; synthesis; by irreversibly binding coverage includes to 30s ribosomal subunits P. aeruginosa Silver sulfadiazine Bactericidal against Gram (+) Binds to bacterial DNA and and Gram (-) organisms inhibits its replication Antifungal Agents Class and Prototypes Spectrum of action Azoles Eg. Fluconazole, Ketoconazole, Sertaconazole, Eberconazole ,etc. (Fungistatic) Dermatophytes, candida, pityrosporum, erythrasma, some action against staphylococcus Allylamines Eg. Terbinafine, naftifine Dermatophytes (fungicidal), Candida albicans (fungistatic) Morpholines Eg. Amrolfine Onychomycosis caused by dermatophytes, scytalidium spp.,Scopularis spp.,dimorphic fungi, C. Albicans, Cryptococcus neoformis, dematiaceous fungi. Antifungal Agents Class and Prototypes Spectrum of action Benzylamines e.g. Butenafine Dermatophyte (fungicidal), C. Albicans (fungistatic), P. versicolor Polyenes Eg. Nystatin Oral and Vaginal Candidiasis Miscellaneous 1. Ciclopirox olamine Dermatophytes, yeasts, molds e.g. Scytalidium spp. Scopulariopsis spp. 2. Zinc pyrithione 1% 3. Selenium disulfide 2.5% P. Versicolor Sterol pathway in fungi and steps at which antifungal drug act. Allylamines (terbinafine, naftifine) Benzylamines (butenafine) Tolnaftale Acetyl coenzyme A Squalene Squalene epoxide Squalene epoxidase Triazoles (fluconazole, itraconazole) Imidazoles (ketoconazole) Lanosterol 14 α Demethylase 14 α Dimethyl Lanosterol Amorolfine Zymosterol δ14-Reductasee Amorolfine Fecosterol Episterol δ7 δ8 Isomerase Amphotericin B Fungal cell membrane synthesis Griseofulvin Fungal cell replication Ergosterol Antivirals Agent Indications Acylovir (5%) cream Herpes labialis, herpes genitalis Penciclovir (1%) cream Herpes labialis, herpes genitalis (longer duration of activity) Cidofovir Human papilloma virus, herpes and pox virus infections, Useful in HIV positive patients Foscarnet In acyclovir resistant cases Idoxuridine Herpes simplex, herpes zoster, human papilloma virus infections Topical and intralesional antiviral agents Viricidal Cytodestructive Immune Enhancer Acylovir Bleomycin Imiquimod Penciclovir Podophyllin Inteferon Cidofovir Trichloroacetic acid Foscarnet Cantharidin Idoxuridine Salicylic acid 5-Fluorouracil Herpes simplex Antiparasitic agents Agent Mechanism of Action Side effects Permethrin (5% cream and 1% lotion) Acts on nerve cell membranes of the parasite causing paralysis and death. Burning, Itching, Numbness, stinging, tingling, Hypersensitivity Gamma-benzene Hexachloride (1% lotion) CNS excitation, Inhibit inositol to produce agitation, delirium, CNS excitation convulsions etc. Benzyl benzoate (25% emulsion) Not known Pruritus, redness, ACD, Seizures Malathion (0.5% lotion) Cholinesterase inhibition in a parasite Irritation to skin Antiparasitic agents Agent Mechanism of Action Side effects Crotamiton (10% solution) Not known Pruritus, swelling, redness Precipitated sulfur (6% lotion) Kills the mite by unknown Hypersensitivity to mechanism sulfur Ivermectin (1% cream and shampoo) GABA-nergic action to block chloride channels Nil and causes tonic paralysis Scabies Calcineurin Inhibitors Prototypes : Tacrolimus (FK 506), Pimecrolimus Mechanism of Action : Immunosuppression - by inhibiting proliferation and activation of CD4+ T Helper cells by inhibition of cytoplasmic enzyme calcineurin. Immunomodulation - by inhibition of mast cell adhesion and inhibition of mediators release from mast cells and basophils. Release of local neuropeptides and transmission of pain and itch. On Keratinocytes- increase stem cell factor release which causes proliferation of melanoblasts and melanocytes. Side Effects : Local burning, Pruritus, Infections, Risk of malignancy (Black Box Warning) Calcineurin Inhibitors Indications Contraindications Eczemas, Atopic Dermatitis Pregnancy Vitiligo Infected lesions Facial and flexural psoriasis Prolonged exposure to sunlight Oral and Genital lichen Planus, Lichen Conditions causing breach in skin striatus, Lichen sclerosus et barrier properties atrophicus Morphea, lupus erythematosus,Bullous disorders H/o contact sensitization Steroid induced Rosacea, Chronic actinic dermatitis Pimecrolimus cream should not be applied to mucous membrane or eyes Cytotoxic and Immunomodulatory agents Imiquimod - 5% cream Mechanism of action Trigger immune system to recognize the presence of a vital infection or tumor and mounts Th1 weighted cellular immune response. Application : 3 times a week ( 6-10 hrs ) for 8 – 12 weeks. Indication : General warts, Actinic Keratoses, Molluscum contagiosum, intraepithelial neoplasia, Bowenoid papulosis, verrucous carcinoma, SCC etc. Side effects : Local : Erythema, irritation. Systemic : Fatigue, fever, myalgia, central and peripheral nervous system disorder, Influenza like symptoms Cytotoxic Agents Agent Mechanism of Action Indication Bleomycin Binds to DNA causing cell to accumulate in G2 phase 5-Fluorouracil Antimetabolite to uracil thus block synthesis of DNA in hyper proliferative keratinocytes Intralesional injection Keratoacanthom a Recalcitrant warts Genital warts Actinic keratosis, BCC, bowenoid papulosis, erythroplasia of queyrat, leukoplakia, etc. Side effects Pain swelling Raynaud’s ph. syst Myelosuppression Pulm fibrosis, hyperthermia, hypotension Local - erythema, crusting, scaling, pain, swelling, pruritus hyper and hypo pigmentation photosensitivity Systemic - Stomatitis, myelosuppression cardiac toxicity, alopecia, etc. Keratolytic Agents Used to treat hyperkeratosis These break cell to cell adhesions, thus help to remove scales Few of these have hydrating effect, thus used as moisturisers Few have anti-inflammatory, anti-ageing effect e.g. Salicylic acid, urea, alpha hydroxy acids such as glycolic acid, lactic acid, coal tar etc. Moisturizers Moisturizers hydrate the skin. Classification : Emollients and Humectants Emollients : These are greasy substances, which hydrate stratum corneum by forming a greasy layer over the skin surface, thereby preventing transepidermal water loss and retaining moisture in the skin. E.g. Liquid paraffin, almond oil etc. Humectants: Humectants are the substances which hydrate stratum corneum by absorbing water from the external environment or from deeper layers of the skin. E.g. Glycerin, urea, lactic acid and sodium lactate etc. Sunscreen Protects skin from Ultraviolet radiations Sun Protection Factor (SPF) : Minimal erythema dose of UVB light with sunscreen applied Minimal erythema dose of UVB light without sunscreen Broad spectrum protection : Full spectrum UVB/UVA protection Water resistant sunscreen : SPF maintained after 40 minutes of water immersion Waterproof sunscreen : SPF maintained after 80 minutes of water immersion Sunscreen Ingredients in sunscreen UVB blockers Octinoxate Octisalate UVA blockers Avobenzone Oxybenzone Physical Blockers Titanium dioxide Zinc oxide Sunscreen Methods of Application : Quantity required is 2g/cm2 30 min before exposure to sunlight Reapplication after every 3-4 hours Reapplication after swimming or sweating Indications : Photodermatoses e.g. polymorphic light eruption Photosensitive eruptions, rosacea , etc. Systemic Lupus Erythematosus Xeroderma pigmentosum Depigmenting Agents Agent Mechanism of Action Side effects Hydroquinone [2% - 5%] Inhibiting tyrosinase thus inhibiting conversion of dopa to melanin Alteration of melanosome function Generation of ROS ICD and ACD Nail discoloration Paradoxical PIH and surrounding hypopigmentation Exogenous ochronosis Permanent depigmentation Depigmenting Agents Agent Mechanism of Action Monobenzyl ether Cytotoxic action on of hydroquinone melanocytes 20% [Residual pigmented areas in residual vitiligo] Retinoids Tretinoin 0.05% Adapalene 0.1% Induced dispersion of keratinocyte pigment granules Interference with pigment transfer Acceleration of epidermal turnover Induce desquamation Side effects Permanent depigmentation Depigmentation at sites other than those being treated Contact dermatitis Erythema Peeling in areas of application PIH Depigmenting Agents Agent Mechanism of Action Azelaic Acid (9-carbondicarboxylic acid isolated from cultures of P.ovale) 10% and 20% Kojic acid (Fungal metabolite derived from acetobacter , aspergillus Penicillium) 1% - 4% Inhibit Tyrosinase Side effects ROS Scavenger capacity Burning, stinging, itching Alteration of hypopigmentation mitochondrial hypertrichosis metabolism Contact dermatitis, Stinging erythema Depigmenting Agents Agent Mechanism of Action Side effects a - Hydroxy Acids Glycolic - 5% - 20% Lactic - 8% - 12% Inhibit tyrosinase Accelerate turnover of stratum corneum Mild irritation, burning sensation. Ascorbic acid Antioxidant Interaction with copper ions at tyrosinase active site Reduce Dopaquinone Liquorice extract e.g. Glabridin Decrease tyrosinase activity Inhibit UVB induced skin pigmentation Mild irritation Depigmenting Agents Agent Mechanism of Action Side effects Arbutin B-Glycoside of hydroquinone In higher concentration greater risk for paradoxical hyperpigmentation Niacinamide (derivative of niacin) Inhibits melanosome transfer from melanocytes to keratinocytes Inhibit tyrosinase Inhibit melanosome maturation Common Indications Melasma, solar lentiginosis post inflammatory hyperpigmentation Most of these agents work best in combination Kligmann’s formula – This is a triple formula being used or melasma (4% hydroquinone, 0.1% tretinoin and 0.1 % Dexamethasone) Melasma Topical Anaesthetic Agents Analgesic Indication Side effects Capsaicin Acts by exhaustion of substance P after repeated application Post herpetic neuralgia pain Redness, burning sensation EMLA ( Eutectic Mixture of Local Anaesthetic creams) 50% lidocaine and 50% prilocaine in an oil in water emulsion Multiple small skin procedures e.g. Needling and extraction, Dermatosurgeries e.g. Radiocautery, dermaroller therapy Transient skin blanching, erythema, urticaria, Allergic contact dermatitis, Irritant contact dermatitis, purpura, hyperpigmentation Miscellaneous Vitamin D derivatives (Calcipotriol) : Inhibits epidermal proliferation, induces differentiation and has anti- inflammatory effects. Indications : Psoriasis, Morphea, etc. Anthralin : Synthetic derivative of Chrysarobin. Affects DNA synthesis and thus reduces keratinocyte proliferation. Used as short contact therapy (5-10min). Indication : Psoriasis. Miscellaneous Coal Tar : By-product of petroleum distillation. Suppresses DNA synthesis in keratinocytes thus decreasing their proliferation. Side effects : folliculitis, acne, allergic sensitization, staining of clothes and phototoxicity. Miscellaneous Antipruritic : Doxepin 5% cream H1 and H2 receptors,adrenergic, muscarinic receptor antagonism Menthol – upto 16% Agonist of thermally sensitive receptor, gives cooling sensation Phenol low concentration (0.5 - 2%) Acts through its anaesthetic effect. Soothing agent : It reduces itching burning and discomfort of skin. e.g. Calamine lotion. Anti – perspirants Aluminium chloride hexahydrate , Formaldehyde soaks, Botulinum toxin injections. Miscellaneous Astringents : These are compounds used to reduce exudation. Mechanism of action : Coagulating proteins Coagulated proteins forms a protective coat Reduces oozing Examples : Potasium Permaganate - 1:4000 to 1:25,000 Condy’s compresses Aluminium acetate ( 1:10 to 1:40 ) ( Burow’s Solution ) Silver Nitrate ( 0.1% - 0.5% ) Miscellaneous Minoxidil : Mechanism of action : Vasodilator by opening potassium channel Increases duration of anagen phase Converts vellus hairs into terminal hairs Uses: Androgenetic alopecia, alopecia areata, Female pattern baldness Available as 2%, 5%, 10% solution, gel, foam. Miscellaneous Topical contact allergens Mechanism of action : Antigen competition: Immune reaction to one antigen may inhibit the development of immune response to another unrelated antigen. Also can stimulate cell mediated cell response in viral infections Agents : Diphenylcyclopropenone Squaric acid dibutyl ester (SADBE) Dinitrochlorobenzene (DNCB) Uses : Alopecia areata, Viral warts MCQ’s Q.1) Which is the measure for the quantity of drug to be applied topically? A. Finger Tip Unit B. Hand Area Measurement C. Both of these D. None of the above Q.2) Sunscreens provide protection against A. UVA B. UVB C. UVC D. UVA and UVB MCQ’s Q.3) All are indications of steroids except A. Papulosquamous disorders B. Pemphigus vulgaris C. Telangiectsia D. Polymorphous light eruptions Q.4) All are keratolytic agents except A. Glycolic acid B. Lactic acid C. Uric acid D. Salicylic acid MCQ’s Q.5) Following factors affect the drug delivery except A. Time of application B. Site of application C. Hydration D. Massaging before application Q.6) 28 year old female patient complains of multiple erythematous papules and pustules in perioral region since last 20 days which is the medication to be avoided in this patient? A. Clindamycin B. Framycetin C. Mometasone furoate D. Silver sulfadiazine MCQ’s Q.7) The following drug is commonly used as a first line therapy for melasma. A. Salicylic acid B. Hydroquinone C. Benzoyl peroxide D. Urea Q.8) A 4 year old child presented with pustular and crusted lesions on the chin. MRSA was isolated on pus culture. Topical therapy of choice:A. Mupirocin B. Povidone iodine C. Silver sulfadiazine D. Framycetin Photo Quiz Q. 7) Which topical agent can be used to treat this condition? Q. 8) Identify the topical preparation and describe its indications? Thank You!