- Andrew Espejo
advertisement

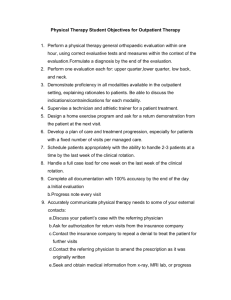
COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS 1 Case Analysis This paper should be high quality, appropriate for an undergraduate study, and suitable for the board of a local health care organization. It must be done alone. Work-in-progress may be reviewed by the instructor for preliminary feedback. The paper should be written in APA style and could be no more than 5 pages long. The content of the paper should educate the audience and at least: a. b. c. d. e. f. g. h. clearly state and explain the underlying case issue (s) and problem (s) to be resolved describe relevant health, economic, finance, and historical background of the case and the importance of the case to the organization describe specific problems identified in the case describe analytical tools and methods used in the case explain the results of the solution and relate them to the original problems and issues explain how this solution (s) is viewed by relevant interest groups in the organization and how it affects (or is likely to affect) various departments suggest what you think will be implemented conclusion/discussion of the presentation with a brief summary of findings, caveats, limitations, etc Name: Criteria Topic: Points Comments/Suggestions Introduction [0 – 3 points] Organization [0 – 5] Content (a- g above) [0 – 35] Original thinking [0 – 3] Writing, grammar, punctuation [0 – 15] Tables, graphs [0 –5] Discussion [0 – 5] Use of references [0 – 2] Timing [0 – 2] ………………………………………………………………………………………………………………… Total [0 –75] Date: COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS Columbia Memorial Hospital - Case Study 6 Andrew Espejo California State University, Long Beach Dr. Sinay May 10, 2013 2 COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS 3 Underlying Case Issue The chief executive officer (CEO), is concerned with one Columbia Memorial Hospital walk-in clinic's financial soundness amongst three other area hospital's walk-in clinics. Currently, Columbia Memorial Hospital is an acute care hospital with 300 beds and 160 staff physicians, and is one of 75 hospitals owned and operated by Health Services of America, a for profit publicly owned company. Columbia Memorial Hospital regardless of the presence of two other acute care hospitals, remains highly profitable because of its well-appointed facilities, fine medical staff, reputation for quality care, and the amount of individual attention to patients. Columbia's stand alone clinic in question is located across the street from the area's major shopping mall, about two miles from the hospital. Walk-in clinics should hope to produce profits quickly as they provide treatment for walk-in patients suffering from ailments such as sprains, cuts and the flu. These clinics charge $60 to $200, depending on procedures. Only three of five walk-in clinics survive today and none of these three appear to be a money maker. Currently the clinic handles 45 patients per day yet it fails to reach its potential of 85 a day. The problem is that the clinic is staffed and ready for 85 patients yet these extra resources end up as extra expenses. This led to Columbia's chief financial officer to look into the matter of the walk-in clinic. The CFO stated three potential outcomes for the clinic. Potential Outcomes for Walk-In Clinic Decision (1) the clinic should be closed (2) the clinic should continue to operate as is - that is without expanding its marketing program (3) the clinic could continue to operate, but with the expanded marketing program. Projected Profitability Possibilities The projected profitability of the walk-in clinic for the entire year if volume continues at its current level is a net profit (loss) of $3,173 and a gross margin (%) of -5.8% at 1,350 visits monthly. So, for an entire year the projected profitability adds up to $38,076 in loss. The amount of additional visits per day that would be required to break even without the new marketing program is 17 with a monthly profit of $777 requiring a total of 62 patients total. The amount of additional visits per day that would be required to break even assuming that the new marketing plan is undertaken is 24 visits with a monthly profit of $581 requiring a total of 69 patients per day. The amount of additional daily visits the new marketing program would have to bring into make it worthwhile, regardless of the overall profitability of the clinic is 26-30 additional patients. Decision-making involves choosing between alternatives and the focus of incremental analysis is to examine what is different between the alternatives in terms of three major amounts: (1) Revenue differences "benefits" (2) Cost differences (3) Cost savings differences. COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS 4 Figure 1 Breakeven without New Marketing Program $120,000 Total Monthly Revenue $100,000 $80,000 Total Monthly Costs $60,000 $40,000 $20,000 Total Monthly Profit $0 0 5 10 15 20 25 30 35 40 ($20,000) ($40,000) Breakeven Without New Marketing Program If the Columbia did not opt to close the walk-in clinic and continue business as usual, the clinic would only have to at least provide for 62 total daily visits, 17 additional visits above its usual 45 visits. The walk-in clinic would collect $777 in monthly profit, but if visits fell below only by a single visit the clinic would incur a loss of ($377). Total monthly visits at an additional 17 visits would total 1,860 monthly visits, $75,623 monthly revenue, and a total incremental cost of $16, 785. Without the new marketing program the total monthly incremental monthly cost is only $0 versus an immediate $7,000 incremental monthly cost in only the first month. An additional 20 visits would have to occur for a clinic with a new marketing campaign in order to start making it worthwhile as stated previously. However, without the marketing program no such loss would be have to faced in the difficult early couple of months of starting a brand new marketing program with a new fixed cost of $7,000 for a marketing assistant's salary and advertising expenses. Advertising and a marketing assistant's salary's can be paid for, but at the cost of a failed marketing campaign. However, assuming the marketing campaign is a success, it will still take more additional visits to cover the cost of the additional expenses of advertising and such salaries expenses. COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS 5 Figure 2 Breakeven with New Marketing Program $120,000 Total Monthly Revenue $100,000 $80,000 Total Monthly Costs $60,000 $40,000 $20,000 Total Monthly Profit $0 0 5 10 15 20 25 30 35 40 ($20,000) ($40,000) Breakeven with a New Marketing Program If Columbia were to implement a new marketing program with a focus on occupational health services (OHS), then the breakeven point would be attained at 24 additional visits on top of the base 45 visits. The clinic would see a monthly profit of $581, but if additional visits fell below to 23 additional visits, then the walk-in clinic would incur a monthly loss of ($534). It seems that the walk-in clinic is doomed if marketing is not implemented well enough or a big hit with the local occupational health services (OSH). An additional patient from the onset would cost the clinic an additional $21,205 from the incremental variable costs that includes additional patient costs and marketing effort costs. However, because marketing is a fixed cost of $7,000, the incremental costs in the long run end up slowing down. If one ignores the fixed costs since the amount stays the same regardless of whether the selling price stays the same, then a new marketing program would seem like a good risk. However, the power and effect of marketing isn't always fixed. Additional costs of the new marketing plan would cause further load to a clinic that is attuned to operating with a low patient volume so that staff is kept to a minimum. Any additional visits would require additional administrative and medical costs and increases. Increases in the incremental costs associated with increased volume would have a lower gross margin of 2% at 25 additional visits at breakeven than a higher gross margin of 5.2% at only 20 additional visits COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS 6 at breakeven for a much more favorable option of continuing as is without an expanded marketing program. As increasing patient volume becomes tantamount to staying financial viable, hospitals must think about how they market their services to potential referring physicians and patients. Conducting market research is important before starting to decide how to market a clinic and the knowledge of what your competitors are doing and who your audience is, in this case local occupational health services (OHS). Prioritizing marketing goals is also important once one has conducted market research. Next, figuring out your budget once you have decided which service line the clinic will use for its campaign. Lastly, marketing assistant will have to create a tactical plan once a strategic plan is in place detailing how to target occupational health services (OHS). Pieces of marketing will come at a cost though as mention previously. The tactical plan will have to have repeatable steps like print ads, direct mail pieces, TV campaigns, and radio campaigns that are influenced by the strategy the clinic is going for. Again, there are many unknown variables part of the marketing process, and additional research usually takes time and money, both of which are already deep concerns for the walk-in clinic. Figure 3 Incremental Breakeven of Marketing Program $60,000 $50,000 Total Monthly Revenue $40,000 $30,000 Total Monthly Costs $20,000 $10,000 Total Monthly Profit $0 0 ($10,000) ($20,000) ($30,000) 5 10 15 20 25 30 35 40 COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS 7 Incremental Breakeven of the Marketing Program The incremental breakeven point displays incremental expenditures per unit contribution. According to Fig. 3, incremental expenditures per visit would turn a incremental monthly profit of $295 at an additional patient volume of 20 for a total of 65 total daily visits. Suggested Solutions/Alternatives It seems that increasing patient volume is important, but at a cost of quality and overworked staff. If the walk-in clinic needs to tame its load, it should consider an after-hours clinic. This after-hours clinic could increase not only patient satisfaction, but also office staff and physicians. Another advantage is that local insurers should be supportive of an after-hours clinic because of the potential for reducing improper use of ERs and utilization rates of hospitals. To help this after-hours clinic grow quickly, some initial marketing will be required within other practices and physicians in the area. It would also help if a local HMO encouraged members to use the after-hours clinic and help with start up costs. The hours of the after-hours clinic would vary from when people get off work around 4 p.m. to 10 p.m. during regular work days in the week, and morning to evening hours on the weekends. By doing this it could curb patient volume during the weekdays and take care of high volumes during the weekends. Obvious downsides to this alternative is staffing, so during heavily scheduled times, staff might be sent home if the patient volume isn't enough to offset the total costs of continuing with a full staff below peak hours. However, if patient volume were to pick up, nurses would have to be available on call. Decision The clinic should continue to operate as is - that is without expanding its marketing program. This is due to the costlier alternative of hiring a marketing team and requiring more time for the effects of marketing and patient volume to kick in. Operating without a marketing program will allow the clinic to breakeven at 17 patients per day compared to a higher 24 patients per day. The opportunity cost of the operating as is decision is much lower than with a marketing plan when comparing the same volume of patients against each other. Opportunity costs are always relevant because they represent the benefit given up as a result of choosing one option over the other. While they are not cash outlays, they represent an increase in profit for one decision over the other. One of the consequences of completely shutting down the walk-in clinic is the potential for inappropriate use of ER as previously mentioned. Another consequence of closing the clinic is the cancellation penalty of three months' rent ($37,500). This is still a difficult decision to make in a volume based system and in the near future, systems perhaps might move into a value based system. COLUMBIA MEMORIAL HOSPITAL BREAK-EVEN ANALYSIS References Gapenski, L. C., & Pink, G. H. (2003). Understanding healthcare financial management. AUPHA. 8