Teens and Self Injury - Wisconsin Family Ties
advertisement
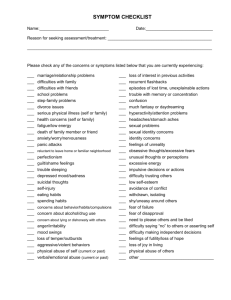
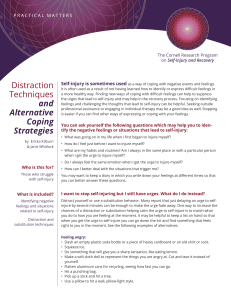
Teens and Self Injury Dale Kaufman, MSSW School Social Worker Middleton-Cross Plains Area Schools dkaufman@mcpasd.k12.wi.us Agenda 1. 2. 3. 4. General information regarding Self-Injury View “Cut: The Movie” (56 minutes) Resources Evaluations Please provide me with your email address if you would like a copy of the PowerPoint for this presentation. DEFINITION of Self-Injury: • Deliberate self-inflicted harm resulting in tissue damage without the conscious intent of suicide • Behaviors include (but are not limited to): – – – – – – Cutting, scratching Burning Interfering with the healing of wounds Hitting or biting oneself Head banging Hair pulling Incidence and Onset • 4% in the general population • = numbers of males and females (though more females present for treatment) • Typical onset: puberty – though can be seen in young children and adults • Often lasts 5-10 years – But can last longer without treatment Background Factors in Teens who Self-Injure: Generalized • Found in = numbers in all ethnic groups • Nearly 50% report physical/sexual abuse (At least 50% have NOT reporting abuse) • Many report that they were discouraged from expressing emotion, particularly anger and sadness – Feelings of emptiness, over/under stimulated – Unable to express feelings – Lonely, fearful of intimate relationships or adult responsibility – Feeling invalidated/disconnected from parents Behavior Patterns • Cutting arm/legs most common practice • May attempt to conceal injuries (long sleeves/pants) • Often make excuses • Significant # also struggle with eating disorders/substance/alcohol abuse – Big difference between self decorating (tattoos/piercings) and self harm – Teens who self harm are seeking relief from emotional distress Warning Signs • Unexplained, frequent injuries including cuts and bruises • Wearing of long pants/sleeves in warm weather • Low self-esteem • Overwhelmed by feelings • Inability to function at home, school or work • Inability to maintain stable relationships Dangers • Can become desperate about lack of selfcontrol and addictive-like nature of acts • May lead to true suicidal attempts • Self-injury may cause more harm than intended. Can result in medical complications or death • Eating disorders/AODA intensifies threat to overall health and quality of life Why? Purposes of Self-Injury: • • • • • • • • • Analgesic Connecting body and mind Control Cleansing Punishment Words cannot express pain Combating a sense of invisibility Rescue fantasy Vengeance Why? Reasons for Behavior: • • • • • • • • • • • • • Feelings of emptiness Over/under stimulated Unable to express feelings Lonely Not understood by others Fearful of intimate relationships and adult responsibilities Way to cope with or relieve painful/hard to express feelings Relief is temporary Self-destructive cycle often develops without treatment Wanting to fit in Feeling emotionally dead inside Self harm feels alive and confirms existence Coping strategy Stigma • Self-injury is not a behavior that “works” for someone who is not in acute emotional distress • Important for caregivers to recognize that there is NO safe amount of self-injury • Self-injury, like substance abuse and eating disorders, is a coping strategy used by people who are in emotional distress • Those who self-injure feel great amounts of pain and often, shame CUT: Teens and Self Injury • A documentary produced and directed by Wendy Schneider • www.cutthemovie.com Parents…what you need to know 1. Injuring is a coping strategy and not the problem itself • Instead of focusing on behavior understand that the child needs help to identify and express emotional issues verbally Parents…what you need to know 2. Some parents find it hard to deal with their own emotional response.. • Don’t minimize the problem (assuming that he/she is just doing it “for attention” • Know that self-injury is never a healthy coping strategy. It is an indication that the child is having trouble coping with stressful issues and emotions. • Some teens are more open with a professional than their parent • Don’t overreact…result could be more hiding of behavior Parents…what you need to know 3. Fear, anger and guilt are all normal reactions. Try to process your own feelings and remain understanding of your teen • Remember…your child is in a great deal of emotional pain that he/she has not been able to express directly Parents…what you need to know 4. Have appropriate expectations of your teen • Adolescents generally find it difficult to indentify, much less discuss feelings and issues that underlie self-injury • It takes time and work Parents…what you need to know 5. Don’t expect to be able to fix the problem yourself • Be available to listen and empathize but… • Teens are usually in need of professional assessment and possibly treatment – Parents are NOT betraying their child by seeking help – By seeking help, you are modeling healthy parental attitudes and showing that you can accept problems and deal with them constructive Parents…what you need to know 6. Try not to threaten or overprotect your teen in an effort to stop the behavior • Power struggles rarely work • Openly express concern • Indicate that you want to help • Encourage teen to talk to you and/or another trusted adult • Get professional help, if warranted • If you observe an actual injury, you can, if necessary transport teen to ER or doctor Parents…what you need to know 7. Don’t hesitate to seek help • Therapy • Hospitalization Parents…what you need to know 8. Take care of yourself!!!!!! • Affects the entire family • Therapy can help both parents and siblings • Important to identify and express your own feelings in a healthy way 9. Don’t expect a quick cure…it takes time to heal Parents…what you need to know • If you believe your child is suicidal, IMMEDIATELY contact your therapist, if you have one or call 911 • Self-injury is a strong risk for suicide • Take suicidal statements seriously