LOWER URINARY TRACT
advertisement

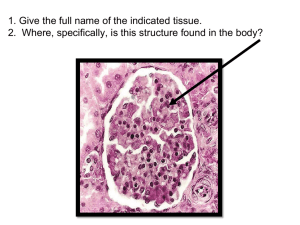
LOWER URINARY TRACT. URETER, BLADDER & URETHRA. By: Abiodun Mark Akanmode LOWER URINARY TRACT. The lower urinary tracts consists of the ureters, urinary bladder and the urethra. These organs are involved in the involuntary storage of urine produced in the upper urinary tract and the voluntary expulsion of urine at an appropriate time and place. LOWER URINARY TRACT There are considerable variations in the anatomy of the male and female urinary tract but we focus our attention on the male lower urinary tract. A thorough knowledge and understanding of the relevant anatomy is essential in understanding the various pathophysiological mechanisms of LUT disorders and their appropriate management URETER. The ureter is a tubular structure ,30cm in length and 0.5cm in diameter. It extends from the renal pelvis to the urinary bladder. The ureters enter the bladder in an obliquely, so that its compressed during micturition to prevent vesico-ureteric reflux. The ureter is lined by transitional epithelium internally and by a fibrous layer which ensheaths the muscular layers. DOUBLE &BIFID URETER. This is a condition in which the upper or the entire part of the ureter is duplicated. Double ureter is associated with double renal pelvis. Most cases are unilateral & of no clinical significance. URETERIC DIVERTICULAR. This is a very rare congenital disorder of the ureter. It is characterized by the presence of saccular outpouchings of the ureteral wall. URETERAL TUMORS & TUMOR LIKE LESIONS Primary tumors of the ureter are very rare. However the malignant tumors of the ureter resemble those arising from the renal pelvis, calyces and bladder. Most of the malignant lesions of the ureter are urothelial carcinomas. Urothelial carcinomas are predominant between the 6th and 7th decades. OBSTRUCTIVE LESIONS OF THE URETER. Various pathologic lesions can lead to ureteral obstruction thus giving rise to hydroureter, hydronephrosis and occasionally pylelonephritis. Sclerosing retroperitoneal fibrosis(RPF):This is an uncommon cause of ureteral narrowing/obstruction characterized by a fibrous proliferation around retroperitoneal structures eventually leading to hydronephrosis. The idiopathic variant of this disease i.e. idiopathic retroperitoneal fibrosis is also called Ormond's disease. OTHER CAUSES OF URETERAL OBSTRUCTION. Intrinsic causes: -calculi/stone. -Strictures. -Blood clots. Extrinsic causes: -Pregnancy. -Endometriosis. -Tumors. URINARY BLADDER. The urinary bladder is the organ that collects urine excreted by the kidneys before disposal by urination. The bladder lies extraperitoneally and the peritoneal surface is reflected on its superior surface. The greater part of the bladder wall is made up of dextrusor muscles while the bladder trigone is a prolongation of the muscle layers from each ureter. CONGENITAL BLADDER ANOMALIES. Bladder or vessical diverticulum: This consists of a pouch-like evagination of the bladder wall. Diverticulum could be acquired or congenital. Congenital diverticulum is mostly ascribed to focal failure in the normal musculature development. Acquired diverticulum is associated with prostatic enlargement & obstruction to urine flow. Although most diverticulum are small are insignificant they might constitute a site of stasis(urine), hence infection and sepsis. BLADDER EXTROPHY. In bladder extrophy developmental defects in the anterior abdominal wall allows for a communication of the bladder with the exterior. The exposed bladder is highly susceptible to infections. CYSTITIS. This refers to the inflammation of the urinary bladder. The common etiologic agents implicated in cystitis are E.coli, proteus, klebsiella and enterobacter. Women are more predisposed to developing cystitis as compare to males because of their shorter urethras. Triad of cystitis is: frequency, lower abdominal pain and dysuria. MORPHOLOGY: ACUTE CYSTITIS. Grossly: Acute cystitis is characterized by a swollen, red and hemorrhagic bladder mucosa. There may be suppurative exudates or ulcer also on the bladder mucosa. Microscopically acute cystitis is characterized by intense neutrophilic exudation admixed with lymphocytes and macrophages. MORPHOLOGY: CHRONIC CYSTITIS. Repeated attacks of acute cystitis lead to chronic cystitis. Grossly: The mucosal epithelium is thickened, red and granular with polypoid masses. long standing cases gives rise to a thickened bladder wall and shrunken cavity. Microscopically: There is a patchy ulceration of the mucosa with the formation of granulation tissue. FOLLICULAR CYSTITIS. This is a type of cystitis characterized by the aggregation of lymphocytes into lymphoid follicles within the bladder mucosa and wall. Follicular cystitis is not necessarily associated with a bacterial infection. SPECIAL TYPES OF CYSTITIS: INTERSTITIAL CYSTITIS. Interstitial cystitis(chronic pelvic pain syndrome):This is a persistent, painful form of chronic cystitis occurring mostly in women. The etiology of which is unknown. Some pt with this condition show chronic mucosal ulcers (Hunner ulcers). Late in this disease, there is transmural fibrosis leading to a contracted bladder . Interstitial cystitis is characterized by suprapubic pain, hematuria, dysuria, frequency without evidence of bacterial infection. INTERSTITIAL CYSTITIS Interstitial cystitis giving rise to a contracted bladder appearance. SPECIAL TYPES OF CYSTITIS: MALACOPLAKIA. This are soft ,flat yellowish lesions found on the surface of the bladder mucosa. They tend to vary from 0.5-5cm in diameter. They are composed of large amounts of foam macrophages, multinucleated giant cells and lymphocytes. Malacoplakia is also characterized by the presence of Michaelis-Gutmann bodies. SPECIAL TYPES OF CYSTITIS: POLYPOID CYSTITIS. This is usually secondary to the irritation of the bladder wall. Its characterized by papillary projections on the bladder mucosa. Indwelling catheters are usually responsible for this variant of cystitis. Polypoid cystitis may be confused for papillary urothelial carcinoma clinically & histologically. METAPLASTIC LESIONS OF THE BLADDER. Cystitis glandularis & cystitis cystica: Here nest (Brunn nests) of transitional epithelium grows downwards into the laminar propria and undergoes transformation into cubiodal or columnar epithelium lining(c. glandularis) or cystic spaces (c.cystica) Both variants are common microscopic findings in a relatively normal bladder. Squamous Metaplasia: injury to the urothelium is often replaced by squamous epithelium. BLADDER NEOPLASM'S. Bladder cancer accounts for 7% of cancer in the US. About 95% of bladder cancers are of the epithelial origin with the rest been of the mesenchymal origin. Most epithelial bladder cancers are of the urothelial (transitional)origin. UROTHELIAL/TRANSITIONAL TUMORS. They account for 90% of all bladder cancers. The 2 major precursor lesions to invasive urothelial carcinoma are: -non-invasive papillary tumors. -flat non invasive urothelial carcinoma(CIS). In about 1/3rd of pt with bladder ca, the cancer has already invaded the bladder wall at the time of presentation and no precursor lesion would be seen. MORPHOLOGY OF UROTHELIAL TUMORS. : The gross pattern of urothelial tumors tends to vary from papillary to nodular or flat. 90% of all urothelial tumors are papillary. Most papillary tumors are low grade and arise from the lateral or posterior wall of the bladder. LOW GRADE PAPILLARY UROTHELIAL CARCINOMA Low grade papillary urothelial carcinoma: characterized by orderly appearance architecturally and cytologically. They tend to recur and they seldomly invade. A B HIGH GRADE PAPILLARY UROTHELIAL CANCER: This variant contains cells that are more architecturally in disarray, areas of larges hyperchromasia seen, abundant mitotic figures etc. 80% of high grade tumors are invasive. BLADDER CANCER EPIDEMIOLOGY. Several factors have been implicated in the etiology of urothelial cancers such as: -Cigarette smoking. -Industrial exposure to napthalamine. -Parasitic infection with shistosoma hematobium. -Drugs: cyclophosphamide etc. -Diet. -Local lesions. -Prior exposure to radiation. -Long term analgesic use. CLINICAL FEATURES OF BLADDER TUMORS. Bladder tumors classically produces painless hematuria. Urgency, frequency and dysuria occasionally accompany the hematuria. Treatment for bladder tumors depends on the stage and whether it’s a flat of papillary lesion. Chemotherapy and radical cystectomy are both proven ways to manage bladder tumors. BLADDER OBSTRUCTION. Obstruction of the bladder neck eventually causes problems with the kidney. Bladder obstruction in males is mostly due to nodular prostatic hyperplasia. Other causes of bladder obstruction include: -Congenital urethral stricture. -Inflammatory urethral strictures. -Bladder tumors. -Mechanical obstruction by foreign body or calculi. -Neurogenic bladder. MORPHOLOGY OF BLADDER OBSTRUCTION. There is hypertrophy & thickening of the smooth muscle of the bladder wall. URETHRA. The urethra runs from the bladder up to the external meatus. The male urethra has 3 major parts-prostatic, membranous and penile. The female urethra is much shorter than the male urethra. The urethra functions to convey urine from the bladder and also as a passage way for various secretions from reproductive organs. URETHRITIS. This is the inflammation of the urethra. Urethritis is divided into gonococcal and non gonococcal urethritis. The bacteria's involved in NGU include E.coli, Chlamydia etc. Urethritis is a component of the REITER’S SYDROME which comprises of arthritis, conjuctivitis and urethritis. TUMORS & TUMOR-LIKE LESIONS OF THE URETHRA. URETHRAL CARUNCLE: this is an inflammatory lesion that presents as a small painful mass around the urethral meatus. its common in older females. PRIMARY CARCINOMA OF THE URETHRA: this is an uncommon lesion, but are mostly of squamous cell origin.