Pain Control, Nitrous, Oraquix
advertisement

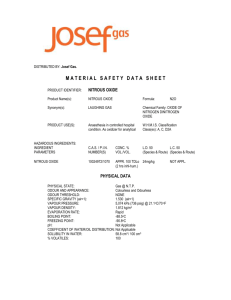
PAIN CONTROL, NITROUS & NON-INJECTABLE’S Lisa Mayo, RDH, BSDH DH102 Clinic II Concorde Career College Reference Wilkins CH37 Mosby’s Handout Topics for Today 1. 2. 3. Pain Psychology and Characteristics Non-injectable Anesthesia: Oraquix, Cetacaine & Topical Nitrous Oxide #1: Pain Psychology and Characteristics Pain Psychology and Characteristics Pain: sensation of discomfort resulting from the stimulation of specialized nerve endings called nociceptors (free nerve endings) Pain perception: process whereby the sensation of pain is transmitted from the periphery to the CNS Pain reaction: result of pain perception. What a person will do about the perceived pain Pain-reaction threshold: amt of pain one must experience before exhibiting a reaction Pain Psychology and Characteristics Pain rxn and threshold varies person to person Pain perception Functional unit: neuron or nerve cell Type of nerve cells: unipolar, multipolar Bipolar: Sensory Cell Fiber transmit dental pain perception neuron characteristics body, nucleus, axon, free nerve endings (nociceptors) diameters: vary, determines speed of impulse conduction and type of pain perceived http://www.youtube.com/watch?v=s6LnDCm1B-A http://www.youtube.com/watch?v=cUGuWh2UeMk Pain Psychology and Characteristics Pain rxn and threshold varies person to person Pain perception Neuron A Fibers (A&C) Fibers: 3-20 microns Myelinated Rapid conduction Require a greater concentration of anes to be blocked Last to be blocked and first to regain sensation C Fibers: 0.5-1 microns Nonmyelinated Slow conduction Have to know this! C Fibers A Fibers Block 1st Block 2nd Regain 2nd Regain 1st Pain Psychology and Characteristics Resting nerve cell membrane Membrane potential: difference in the electrical charge across the nerve membrane Membrane potential maintained by Sodium-potassium pump Permeability of the cell membrane https://www.youtube.com/watch?v=jcZLtH-Uv8M Ions essential to nerve conduction: K+, Na+ Pain Psychology and Characteristics All or None Law Either the nerve fires as strongly as possible or it does not fire at all Minimal threshold stimulus Stimulus: environments change that can be chemical thermal, mechanical electrical Minimal threshold stimulus: magnitude of the stimulus required to initiate a nerve impulse or action potential All-Or-None Law: once the minimal threshold stimulus has been reached, the impulse will travel the entire length of the fiber without stimulation NBQ During an action potential, once the minimal threshold stimulus has been reached, the impulse will travel the entire length of the fiber without stimulation. This explains: a. b. c. d. e. Pain perception Pain reaction threshold Absolute refractory period Membrane potential All-or-none law NBQ During an action potential, once the minimal threshold stimulus has been reached, the impulse will travel the entire length of the fiber without stimulation. This explains: a. b. c. d. e. Pain perception Pain reaction threshold Absolute refractory period Membrane potential All-or-none law Pain Psychology and Characteristics Excitation When minimal threshold stimulus excites the nerve The permeability of the cell membrane changes Influx – Na+ enters the cell Efflux – K+ diffuses to the outside of the cell Depolarization Time interval that exists when ionic concentration are reversing Na enter into the cell (NBQ, exam ques) Reversed polarity Result of a reversal in ionic charges Repolarization Occurs after reversed polarity Membrane becomes hyperpermeable to K+ and impermeable to Na+ K will leave cell (NBQ) Polarity is re-established NBQ The period of time during an action potential of a neuron where potassium becomes hyperpermeable to the cell and sodium becomes impermeable is defined as: a. b. c. d. Depolarization Repolarization Hyperpolarization Refractory period NBQ The period of time during an action potential of a neuron where potassium becomes hyperpermeable to the cell and sodium becomes impermeable is defined as: a. b. c. d. Depolarization Repolarization Hyperpolarization Refractory period Pain Psychology and Characteristics Excitation Action potential Rapid sequence of changes in the membrane potential (negative to positive, then positive back to negative) Depolarization: results in reversed polarity Repolarization Absolute refractory period Period during depolarization and reversed polarity when the cell membrane cannot be re-excited Relative refractory period During repolarization, the nerve cell membrane can be reexcited, but it requires a greater stimulus than the stimulus required for excitation from the resting state Nerve Communication https://www.youtube.com/watch?v=HnKMB11ih2o Pain Psychology and Characteristics Pain Intensity determined by # of fibers stimulated Anatomy of the area Dimensions of the area being stimulated Frequency Duration of excitation of stimulus Pain Psychology and Characteristics Factors affecting pain reaction threshold Emotional state: greater anxiety and negativity = lower pain rxn threshold Fatigue: greater fatigue = lower pain rxn threshold Age: younger = lower pain rxn threshold Nationality Highest: American Indian Lowest: Latin Americans, Southern European Gender: variable Pain Psychology and Characteristics Pain control mechanisms: 5 ways to control, part of DH care plan, goal = utilized before the patient experiences pain 1. 2. 3. 4. 5. Remove the painful stimulus: patient avoids dental appointment; clinician corrects faulty, pain-causing instrument technique. Block the pathway of the pain message: local anesthetic, topical anesthetic Prevent pain reaction by raising pain reaction threshold: Nitrous oxide-oxygen conscious sedation; nonopioid analgesics such as nonsteroidal anti-inflammatory drugs (NSAIDs) Depress central nervous system: general anesthesia Use psychosedation methods (also called iatrosedation): nonpharmacologic technique that reduces patient anxiety, builds a trust relationship, or lets the patient feel more in control. May be used alone or may be combined with pharmacologic pain management Drugs To Aid in Pain Reduction Nonopioid analgesics: OTC analgesics are an effective adjunct for preventing or reducing the mild to moderate discomfort Acetaminophen (Tylenol), Aspirin (but ↑ risk bleeding) NSAIDs (Non-steroidal antiinflammatory) Drugs of choice for dental pain Ex: Ibuprofen (Motrin), naproxen Actions Block prostaglandin synthesis at peripheral nerve endings to inhibit generation of pain message Suppress onset of pain Decrease pain severity Anti-inflammatory, analgesic, antipyretic #2: Non-injectable Anesthesia 1) 2) 3) Oraquix Cetacaine Topical Noninjectable Anesthesia Indications for use Adults only, not been studied in children Pockets where profound pulpal anes not necessary Needle-phobic patients Contraindications Amide allergy Methemoglobinemia Armamentarium and pharmacology Cartridge of 1.7g lidocaine + prilocaine Blunt-tipped applicator 1.) Oraquix Lidocaine + Prilocaine gel Common name = Oraquix® Amide (just like local anes) Used on adults who require limited pain control during root planing in perio pockets Effectiveness limited in deep pockets with more moderate to severe bone loss Need to record in chart and make Dr aware If Dr was to use anes as well, need to know so to avoid medical emergency (cannot overdose on anes) Anesthetic Gel Gel contents Anesthetics: 2.5% lidocaine and 2.5% prilocaine amide Polyxamers: thermosetting agents pH adjuster: hydrochloric acid Purified water Gel characteristics Low viscosity fluid at room temperature Gel at oral temperature Technique Administration Treatment time Dispense a thin layer of the anesthetic gel at the gingival margin Wait 30 seconds Insert blunt-tipped applicator into the subgingival pocket, dispense product until pocket begins to overflow, then repeat in adjacent area Onset: 30 seconds Duration: 20 minutes with a range of 14-31 minutes Maximum dose: 5 cartridges per appointment If local anesthetic is used, will need to add amt of Oraquix carpules used to avoid overdose Oraquix Set-Up 3-13 Opened Items 3-13 Needle and Carpule 3-13 Loaded Handle and Ready To Go! 3-13 You Tube http://www.youtube.com/watch?v=l_Cb-a9Hmsc 2.) Cetacaine Combo of benzocaine, aminobenzoate & tetracaine hydrochloride Esther topical: esthers have more propensity for allergic rxns than amides Indicated in adults who require pre-injection, deep scaling, suture removal anesthesia Available in spray, liquid, gel foam If use as spray: when patient inhales – has immediate absorption Need to have patient hold their breathe while spray Cetacaine 3.) Topical Anesthesia Drug applied to the surface of the mucous membrane to produce a loss of sensation Short acting Not a substitute for local anes Indications for use DH visits where local may not be necessary Prevention gag reflex during x-rays, impressions or procedures Probing if patient discomforted Suture removal Topical Anesthesia Absorption of drug Varies with thickness of stratified squamous epithelial covering, degree of keratinization Highly resistant: skin, lips, palatal mucosa Absorb slowly Attached Prompt Tissue gingiva, buccal mucosa (thick tissues, tissue over bone) absorption without keratinization (soft), such as vestibular mucosa or over the pterygomandibular space (inferior alveolar, lingual, buccal) Agents Used in Surface Anesthetic Preparations Benzocaine or ethyl aminobenzoate Ester type 20% formulation Most widely used Liquid, gel, ointment, spray Not readily absorbed into circulation Potential for toxicity is minimal May cause allergic rxn esp w/prolonged use Agents Used in Surface Anesthetic Preparations Tetracaine hydrochloride Ester type Combo of drugs in liquid, gel, and controlled-dose spray Readily absorbed causing deeper penetration Longer effect More potential for toxicity Should not be used over a large area Agents Used in Surface Anesthetic Preparations Lidocaine and lidocaine hydrochloride Amide Only amide used alone as a topical (NBQ) Ointment, spray, and transoral patch, and in combination with prilocaine Toxicity unlikely from topical alone but would be additive with other amide anesthetics Agents Used in Surface Anesthetic Preparations Lidocaine Transoral patch Delivery system that uses a bioadhesive patch to improve the duration of contact between the topical and oral soft tissue Provides profound soft tissue anesthesia as well as minimal pulpal anesthesia in some cases Agents Used in Surface Anesthetic Preparations Dyclone or dyclonine hydrochloride Ketone type 0.5 or 1% formulation from a compounding pharmacy Available as a liquid As a gargle, it is good for gag reflex suppression Slow onset, up to 10 minutes Long duration, up to 1 hour Application of Topical Patient preparation: consult med hx for allergies Application technique Surface application: Topical is applied with a cotton-tipped swab or cotton roll Excess topical is removed by rinsing or gentle wiping Tissue needs to be dried first!! Application of Topical Aerosol spray NEVER direct completely towards the throat Transoral patch Air dry the tissue for 30 seconds, apply the patch, and hold in place with firm finger pressure for an additional 30 seconds Apply for 5 to 10 minutes prior to most procedures May be left in place for up to 15 minutes Injections should not be given through a patch, remove prior Transoral Lidocaine Patch Placement 2-4mm apical to free gingival margin Completion of Topical Anesthetic Application Wait appropriate length of time for anes to take effects Limit drug exposure: apply only to area of need, use smallest effective amount Remove residual after application Record topical drug information in patient record #3: Nitrous Oxide Nitrous Oxide-Oxygen Synonymous terms Conscious sedation Patient is always awake and able to respond to verbal commands Protective reflexes are intact – including the ability to maintain an open airway, breathe automatically, and cough so that aspiration is avoided Inhalation Nitrous sedation oxide and oxygen gases are inhaled through the nose Nitrous Oxide-Oxygen Synonymous terms Nitrous oxide psycho-sedation Acts on the CNS in such a way that pain impulses are not relayed to the cerebral cortex or the interpretation of pain impulses is altered Relative Refers analgesia to the state of sedation produced Alters the mood and increases the pain reaction threshold but does not totally block pain sensations Nitrous Oxide-Oxygen Produces analgesia, reduced anxiety Loss or reduction on pain sensibility without loss of consciousness Achieves optimum analgesia 30% - 40% nitrous oxide for most patients The need for higher or lower concentrations depends on individual biologic variability Nitrous heavier than air, colorless sweet smelling, nonirritating and non-allergenic Nonflammable but will support the combustion of flammable substances Nitrous Oxide-Oxygen Relatively insoluble in blood Primary saturation of blood occurs in 3-5 minutes The gas molecules at the alveoli-blood interface and blood-brain interface pass readily to the tissue with the lowest concentration of nitrous oxide Results in rapid onset and recovery Results in potential diffusion hypoxia at completion of sedation procedure if 100% oxygen is not administered Condition in which the body or a region of the body is deprived of adequate oxygen supply Not metabolized in the body, remains unchanged in blood and tissues Enters and exits almost entirely through the lungs Nitrous Oxide enters and exits primarily through LUNGS Nitrous Oxide-Oxygen Nitrous INSOLUBLE in the blood = does not attach to a hemoglobin molecule by displacing oxygen and/or CO2 Because of this = nitrous has a very FAST onset of action in the body Also has a very FAST way to eliminate Nitrous Procedure Diffusion hypoxia If patient is returned directly to room air rather than 100% oxygen, diffusion hypoxia can result Nitrous oxide diffuses into an area of lower concentration more rapidly than oxygen, causing inadequate oxygen in the alveoli if the patient is not given supplemental oxygen at the completion of sedation Hypoxia can result in patient discomfort or syncope Inadequate post-sedation oxygen may result in a feeling of lethargy or headache Nitrous Oxide-Oxygen Chemistry Nitrous oxide properties Stored as a liquid at 650-900lbs per square inch (psi) in a blue cylinder and delivered as gas The contents of the N2O cylinder cannot be determined by the pressure gauge until it is almost empty Colorless Tasteless Sweet-smelling Non-explosive but supports combustion If you put a flame to the tank, it will explode! Have to do something to nitrous tank to make it explode Nitrous Oxide-Oxygen NB Alert Nitrous abuse (high doses for prolonged periods of time) can lead to a deficiency in vitamin B-12 due to its interaction with the enzyme methionine synthase Enzyme is necessary for DNA synthesis and erythrocyte production Deficiencies in B12: pernicious anemia and megaloblastic anemia Nitrous Oxide-Oxygen Chemistry Blood-gas solubility coefficient Blood-gas solubility coefficient of nitrous is 0.47, which means that 100mL of blood dissolves 47mL of nitrous This blood-gas solubility coefficient accounts for the rapid onset and recovery from the effects of the analgesic Nitrous is 15x more soluble in the blood than nitrogen, nitrous displaces nitrogen in blood If nitrous does get into the blood, very insoluble Passes primarily in and out of lungs Nitrous does not compete with oxygen and carbon dioxide in combining with the hemoglobin molecule Nitrous Oxide-Oxygen Chemistry Oxygen (O2) Stored as a gas in a green cylinder and delivered as a gas Contents of the oxygen cylinder can be determined by reading the pressure gauge Equipment Cylinders Blue: nitrous Green: oxygen Pharmacology No effects on heart rate, blood pressure, liver or kidneys Nitrous can be used for long periods of time as long as adequate amt of oxygen is delivered simultaneously Nitrous affects all sensations such as hearing, touch Nitrous reduces the gag reflex but does not eliminate it Physiology Nitrous works by depressing the CNS The exact mechanism of action is unknown, however the effect results in either altering the relay of nerve impulses to the cerebral cortex or causing them to be interpreted differently Patient experiences reduced anxiety & increased tolerance to pain Pain perception is not blocked Stages of Anesthesia Stage I: Analgesia Stage Stage II: Delirium or Excitement Stage Hyper-responsiveness to stimuli Exaggerated inhalation and loss of consciousness Stage III: Surgical Anesthesia Patient feels pain but is not bothered by it 3 planes: first 2 are appropriate for DH care Stage nitrous-oxide oxygen sedation keeps pt in OMS 4 planes Stage IV: Respiratory Paralysis Patient no longer breathing independently Indications for Use Mild apprehension Refusal of local anes Allergy to local anes Hypersensitive gag reflex Intolerance for long appts Cardiac conditions Asthma Cerebral palsy Contraindications to use Pregnancy: controversy on nitrous use Communication difficulties Sign language, special needs, age (dementia) Nasal obstruction COPD (emphysema, bronchitis) Cystic fibrosis Pacemaker (unshielded) Multiple sclerosis Emotional instability Negative response to past experience Reformed drug and alcohol abusers Contraindications to use Patients on CNS agents: nitrous can combo w/their effects and can send patient into conscious/general sedation 1. 2. 3. 4. 5. Benzodiazepines: valium, xanax, ambien. Valium ½ life is 20-60HRS (longest ½ life of all drugs on this list). Ambien 2-3HRS Barbiturates Anticonvulsants Antidepressants: Bupropion (Wellbutrin) Antipsychotics Contraindications to use Recent eye/ear surgeries Eye: surgery will drain eye, Dr’s use a gas to fill it back up once stitches removed. In meantime you use nitrous – gas will fill any voided space Ears: Eustachian tubes Respiratory obstruction: sinusitis Nose, ears, eyes, throat, etc… Advantages of Use Hx cardiovascular disease: oxygen enrichment coupled with stress reduction Simple, relatively safe procedure to perform Minimal equipment No restraining straps or pharyngeal airway Patient awake and responsive Rapid onset and recovery No need for someone to bring or take patient home No post-op tests No food restrictions pre-op (would be best to avoid a very heavy meal) No need to spend time in a recovery room Disadvantages of Use Over-sedation causes vertigo, nausea, vomiting (emesis) Difficult behavioral problems cannot always be managed Instrumentation of max ant region difficult due to position of the mask Signs and symptoms of nitrous oxideoxygen sedation Objective signs: directly observed by patient Awake, lessened pain rxn, drowsy, relaxed Normal eye and pupil rxn, normal respiration, normal BP & pulse Minimal movement of limbs Flushing of skin, perspiration Little to no gagging or coughing Speech infrequent or slow Signs and symptoms of nitrous oxideoxygen sedation Subjective symptoms: reported by the patient Mental and physical relaxation Lessened pain awareness Indifference to time and surroundings Floating sensation Warmth Tingling or numbness Sounds seem distant Tag System for Cylinders Equipment Gas machine Yokes Flowmeter Pressure gauge Reservoir bag Portable or piped into tx rooms Equipment Gas delivery system Regulator or reducing valve Converts high pressure of gas in the cylinders to a usable, lower level Subject to extreme high temperature if compressed gas cylinders are opened quickly Equipment Gas delivery system Flow meter: Visual indicator of liters per minute (L/min) flow of oxygen and nitrous oxide Gas flow rates of nitrous oxide and oxygen are adjusted independently The sum of the two is the total gas flow rate A total combined gas flow rate is established and the respective concentrations of the two gases are adjusted concurrently Equipment Gas delivery system Reservoir bag Reservoir of gases to accommodate an exceptionally deep breath Allows for visualization of respirations for monitoring May be used to provide oxygen in assisted ventilation if attached to a full face mask with relief valve Conducting or breathing tubes Equipment: Tubing Equipment Mask 2 hose scavenger systems reduce the nitrous exhaled into the air & breathed in by the operator Scavenging systems reduce environmental nitrous contamination from 900-30 parts per million (ppm) Max allowable contamination in health care environment is 50ppm Good fit around patient nose is a must Disposable or sterilizable Mask Equipment Set-Up Nasal mask Scavenger system Select the appropriate size for optimum comfort and minimum gas leakage Attach to tubing If a portable unit without pre-plumbed scavenger system Our clinic has this system Connect, usually to high-speed volume evacuation, and activate system Adjust setting of scavenger system Turn on gas cylinders Open slowly, first oxygen, then nitrous oxide Centralized gas systems are turned on at the beginning of the day Equipment: Handling Handle carefully No grease, oil, lubricant, or hand cream around the cylinder valves or any fittings that come in contact with the gases Store vertically on a rack or in another stable and secure manner Open cylinder valves slowly in a counterclockwise direction Safety Measures Color-coded tanks: blue & green Pin index system Diameter Index system Ensures that the nitrous cylinder does not fit into the yoke that holds the oxygen cylinder, and vice versa Diameter of hole at top of cylinder fits only with corresponding cylinder head Audible alarm system: when oxygen runs out Automatic turnoff: when oxygen is depleted Oxygen maintained at 2-3L at all times in most units Oxygen flush: fills reservoir bag with 100% oxygen Pin Index System Pressure Gauge Nitrous Procedure Establish volume of gas flow: RDH CAN DO 100% oxygen Gas flow rate 5-7 L/min for adults 3-4 L/min for children Place nasal hood, adjust for comfort; patient may assist in positioning Adjust flow using the inflation of the reservoir bag and feedback from the patient Nitrous Procedure Titration Individualized drug dose is determined by increasing the percentage of nitrous oxide in small increments until the optimum sedation level is achieved based on clinical signs and symptoms. Start titration at 10-15% concentration of nitrous oxide Because of the rapid uptake of nitrous oxide in the lungs and distribution through the body, the effect of each dose can be assessed after 1-2 minutes More next slide Nitrous Procedure Titration Observe the patient for signs of relaxation or other changes, ask the patient what is felt Adjust dose: Increase or decrease the nitrous oxide by 5% to 10% when the optimum individual dose has not been achieved Wait 1 to 2 minutes and reassess Repeat as needed TEXAS: CAN ONLY DECREASE, NOT INCREASE! 70% of patients = 30-40% nitrous oxide range At high altitudes, greater nitrous oxide concentrations will be needed because of the change in the partial pressure of the gases Nitrous Procedure Titration Continue to monitor and adjust the concentration throughout the appointment As the appointment proceeds or during less anxietyproducing parts of the appointment, a lower dose may be more comfortable Avoid excessive fluctuations Never leave a sedated patient unattended Sedation can become deeper without some stimulation or interaction Nitrous Procedure Recovery Return the patient to 100% oxygen for at least 3-5 minutes or longer if needed for full recovery Signs of recovery report of feeling “back to normal” Comparable pre-sedation and post-sedation vital signs Patient’s Factors affecting recovery time Biologic variation Duration of sedation procedure Concentration of nitrous oxide administration Generally, the more nitrous oxide administered, the longer the recovery time Nitrous Procedure Dismissal follows full recovery Usually the patient is able to return to all normal activities, including driving Record keeping and documentation Documentation will vary according to state laws Most should include Tidal volume in Liters Amt of nitrous in L or % Amt of oxygen in L or % Duration of sedation and recovery with oxygen flush Total gas flow rate (L/min) Oxygenation period: Flush with oxygen at end of appt and for how long BP at beginning and end of appt Statement of patient’s recovery status and any post care instructions given Summary of patient’s response to nitrous oxide can be helpful for subsequent appointments Occupational Exposure Chronic occupational exposure to nitrous oxide may have deleterious effects on health Potential health problems Reduced fertility with as little as 3-5 hours of unscavenged nitrous oxide exposure per week Spontaneous abortion Increased rate of neurologic, renal, and liver disease Decreased mental performance, audiovisual ability, and manual dexterity Occupational Exposure Recommended exposure levels Consensus not been reached, currently no exposure standard National Institute Occupational Safety and Heath recommended no more than 25ppm during administration Methods for minimizing occupational exposure Effective scavenging system that can move 45 L/min of air Maintain equipment and inspect regularly for gas leaks, especially at the locations illustrated on the next slide. Shut off and secure equipment at the end of each day Improve general air quality: introduce fresh air, use a nonrecycling air-conditioning system, or open a window Vent the scavenger system gases outside the building and away from windows and air intakes Minimize patient conversations and mouth breathing Fit the nasal hood carefully to avoid leaks Set conservative limits on the duration and concentration of nitrous oxide use per patient (Adapted from National Institute for Occupational Safety and Health (US). Alert: controlling exposures to nitrous oxide during anesthetic administration. Cincinnati: US Department of Health, Education, and Welfare; 1994. p. 5. Publication No. 94–100. Joint publication of Public Health Service, Centers for Disease Control, National Institute for Occupational Safety and Health).